![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
|
When does labor and birth happen?
|
When the baby is mature enough to handle extrauterine life but is not too big to cause a problem.
|
|
|
labor
|
physiologically--
• process of moving the fetus, placenta, and membranes out of the uterus clinically-- • progressive contractions (longer, faster, stronger) resulting in progressive cervical change (dilation & effacement) |
|
|
factors affecting labor
|
• passenger- baby
• passageway- cervical canal • powers- contractions • position • psychological response |
|
|
fetal lie
|
**relationship b/w the long axes of the fetal & maternal spine
• longitudinal • transverse; cannot deliver • oblique; baby is oriented diagonally and usually covert during labor process >> longitudinal |
|
|
fetal presentation
|
**part of fetus that will enter the pelvis first
• cephalic/vertex • breech, e.g. butt, foot • shoulder |
|
|
fetal head
|
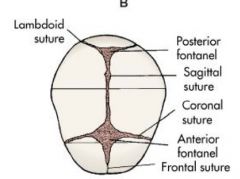
feel for suture lines to determine head positions--
• posterior- 2 branches • anterior- 3 branches **suture lines exist for ease of birth pressure >> molding |
|
|
fetal attitude
|
**relationship of fetal body parts to reach other
• flexed; when flex, baby's head is size of pelvis • extended • military |
|
|
fetal positioning
|

**relationship of denominator (landmark) of the presenting part to the four quadrants of the mother's pelvis
"junk in the trunk" 1/ baby on R or L side of mother's pelvis? 2/ landmark/presenting part? think of fetal attitude 3/ is the butt/spine anterior/posterior/transverse? |
|
|
fetal station
|
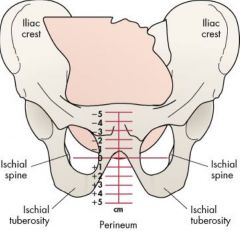
**relationship of presenting part to the ischial spines of maternal pelvis
• cm bove or below • @ station 0, baby is in true pelvis and makes commitment to deliver |
|
|
passageway
|
• bony pelvis- cannot be changed
• birth canal • soft tissues |
|
|
pelvis type
|

gynecoid--
• normal; 50% of females • good prognosis for VD android-- • male pelvis; 23% of females • angular & narrow • poor prognosis for VD anthropoid-- • longer AP diameter • 24%, good prognosis for VD platypelloid-- • shorter AP diameter • 3%, poor prognosis for VD |
|
|
maternal position
|
• affects adaptation to labor
• encourage frequent position changes to (+) perfusion, comfort, & relieves fatigue |
|
|
positive positions for labor
|

**all upright >> gravity aids labor
"hands & knees" position takes pressure off perineum |
|
|
birthing positions
|

**squatting position is best b/c it opens up pelvic outlet
• lateral recumbent takes pressure off perineum • medical model tries to mimic squatting during contractions w/ stirrups |
|
|
powers
|
primary powers--involuntary
• uterine contractions >> cervical changes secondary powers--voluntary • expulsive uterine contractions • maternal pushing efforts |
|
|
ferguson's reflex
|
urge to push @ station 0
|
|
|
primary powers
|
characteristics--
• frequency • duration • intensity |
|
|
Which part of the cervix stretches out during effacement?
|
cervical canal
|
|
|
T/F. Primips efface before they dilate.
|
True; multips do both at the same time and delivery more quickly
|
|
|
true v. false labor
|
quality of contractions--
• false labor- contractions w/o cervical change; cervix should be anterior and thinning • if mom is "LCP" long closed posterior >> not anytime soon location of contractions-- • true labor is @ funds • false labor is @ groin/leg response to movement/position change-- • true labor does not stop w/ activity; false labor will |
|
|
impending labor s&s
|
• lightening
• stronger braxton-hicks • mucus plugs • bloody shows • cervical ripening • burst of energy • SROM • GI upset |
|
|
lightening
|
• baby drops down cervical canal >> pressure on sciatic nerve >> shooting pain down lower extremities
• lightens mom's load >> she can breathe better |
|
|
braxton-hicks
|
**false labor contractions
• uterus is practicing • not as painful • promotes cervical ripening • starts @ 4-5 mos |
|
|
mucus plugs
|
**occludes cervical canal
• estrogen has build-up secretion that prevents bacteria from entering • attached to baby's capillaries; when it passes during effacement/dilation >> bloody show |
|
|
stages of labor
|

• starts w/ first true sign of labor
• most placental delivery is within 30 mins; if longer than one hour >> manual removal |
|
|
1st stage of labor
|
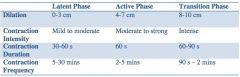
**for onset of regular uterine contractions to full dilation; include three phases; total duration can be prolonged for total of one hour w/ anesthesia
1/ latent 2/ active 3/ transition |
|
|
2nd stage of labor
|
**full dilation to birth of fetus
• the pushing stage • physiological; ferguson's reflex |
|
|
cardinal movements
|
1/ engagement
2/ descent 3/ flexion for smallest head diameter 4/ internal rotation fetal head must rotate to fit the diameter of pelvic cavity 5/ extention due to resistance of pelvic floor, mechanical movement of vulva opening, & pressure from synthesis pubis 6/ restitution shoulders of fetus enters pelvis and remains oblique when head rotates to AP diameter through internal rotation >> head becomes twisted and will untwist once pressure is gone 7/ external rotation as shoulders rotate into AP diameter >> head is turned further to one side 8/ lateral flexion |
|
|
3rd stage of labor
|
**from birth of newborn to birth of placenta
|
|
|
placental separation
|
**can be spontaneous or manually removed
signs-- • change in shape as uterus contracts & appears more globular • gush of blood from vessel dilation • cord lengthening • change in position of uterus |
|
|
placenta, membranes, & cord
|
dunkin side--
• maternal • vascular, attached to uterine wall schultz side-- • newborn side • attached to umbilicus wharton's jelly-- • protective covering of vessels |
|
|
T/F. Placenta of a smoker is smaller than that of a non-smoker.
|
False; it is larger b/c smoking causes vasoconstrictions >> placenta needs to increase surface area to deliver sufficient blood
|
|
|
4th stage of labor
|
**maternal stabilization/homeostasis
• physical readjustment; first hour is most critical >> monitor for PPH • initial bonding & interaction w/ baby • initiate feeding |
|
|
perception of pain
|
factors include--
• culture • anxiety/fear • previous birth experience • childbirth preparation >> when medicating, earlier is better to decrease anxiety and fear |
|
|
nonpharmacological relief
|
• relaxation/breathing techniques
• imagery • music • touch • hydrotherapy • TENS • accupressure • heat & cold • hypnosis • biofeedback • aromatherapy **senses are heightened during delivery, esp. in transitional phase >> coping mechanisms may no longer work >> make sure you get rid of item when mom no longer wants it |
|
|
pharmacological relief
|
systemic analgesia--
• opioids • ataractics; tranquilizer, analgesic potentiator • barbituates • benzodiazapines anesthesia-- • local, general • pudendal block- used during sutures • spinal anesthesia • epidural block • combined spinal-epidural blocks • general anesthesia |
|
|
Why is having an antagonist so important when administering narcotics?
|
**narcan is narcotic antagonist
narcotics (-) RR, HR, and perfusion >> want an antagonist just in case |
|
|
analgesics v. anesthetics
|
analgesia--
• relief of pain w/o total loss of feeling or muscle movement • usually offered to women in labor or s/p surgery or delivery anesthesia-- • blockage of all feelings, i.e. pain • mainly used during surgical procedures, e.g. cesarean delivery |
|
|
systemic analgesics
|
**not given right before delivery b/c they slow baby’s reflexes & breathing
• often given as IM or IV • act on nervous system ADEs-- • nausea • drowsiness/trouble concentrating |
|
|
local anesthesia
|
• provides numbness or loss of sensation in small area
• does not lessen pain of contraction • used during episiotomy • does not affect baby; usually no side effects |
|
|
regional anesthesia
|
**most effective during labor
epidural analgesia-- • aka epidural block causes loss of feelings in lower areas of body while patient remains awake & alert • can be given soon after start of contractions or later as labor progresses • can increase dose of anesthetics for cesareans or if vaginal birth requires forceps or vacuum extractions spinal block-- • rapid effects but only lasts 1-2 hours • much thinner needle; smaller dose of drug • injected into sac of spinal fluid below spinal cord usually only given once during labor >> usually given during delivery combined spinal-epidural blocks-- • has both effects; fast acting & longer lasting • injected into spinal fluid & into space below the spinal cord • some women are able to walk after the block is in place |
|
|
general anesthesia
|
**loss of consciousness
used when regional block is not possible; often used for urgent cesarean deliveries |
|
|
anesthesia for cesarean births
|
factors--
• health of mother and baby • why cesarean is performed |
|
|
epidural placement
|
• given in epidural space below spinal cord
• back is curved outward and patient is not allowed to move |
|
|
systemic analgesia risks
|
• fetal depression
• prolonged labor • n/v >> give zofran • itchiness >> give benadryl |
|
|
anesthesia risks
|
• maternal hypotension >> RN should be nearby to administer IV fluids if needed
• fetal bradycardia • prolonged labor; (-) urge to push during 2nd stage |
|
|
OB rules
|
1/ massage fundus
2/ turn on L side to (+) perfusion; IV; O2 3/ is baby better off in or out? 4/ what happens in previous pregnancy will happen in another |
|
|
L&D admission
|
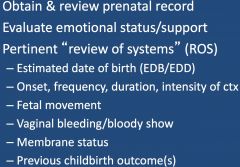
• if unable to obtain prenatal record >> urine test
• fetal movement is sign of baby's well being |
|
|
How can you tell if membrane is ruptured?
|
swab and analyze under a microscope >> amniotic fluid looks like a fern tree
|
|
|
admission assessment
|
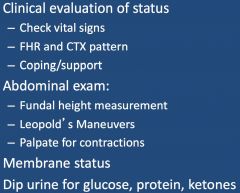
fundal height measurement--
• @ 20 wks, umbilicus will start to ascend 1 cm/wk • measured from fundus to synthesis pubis leopold's maneuvers-- • feel baby inside the uterus to see what position s/he is in urine dip-- • glucose >> DM? • protein >> BP, kidney function? • ketones >> dehydration? |
|
|
rupture of membranes
|
• SROM or AROM
• note time, color, odor, & amount; anything w/ a foul odor indicates infection • check FHR & perform vaginal exam to check for cord prolapse • if meconium is in fluid, prepare suction for birth & call peds |
|
|
1st stage management (active phase)
|
• check patient q 15-30 mins
• document FHR and contractions q 15-30 • BP q 1-2 hours • temperature q 4 hrs if membranes intact v. q 1-2 hrs if membranes ruptured; if membrane ruptured > 12 hours, give antibiotics • void q 2 hrs • frequent position change |
|
|
2nd stage management
|
• FHR q 5 mins or b/w contractions
• BP q 5-15 mins • support & encourage • positional changes • room preparation; make sure laryngoscope is present in case infant aspirates on meconium |
|
|
perineal outcomes
|
>> intact, laceration, episiotomy
whether you tear or not depends on-- • previous tears • nutrition- high protein diet decreases risks |
|
|
types of episiotomies
|
midline (MLE)--
• goes into perineal body >> high risk of going through rectum • better healing, less pain mediolateral (RML/LML)-- • goes into gluteal muscles • slower healing, more pain • more blood loss |
|
|
Why can't the fundus be pushed during contractions?
|
It may cause uterine expulsion.
|
|
|
3rd stage management
|
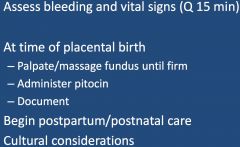
PIT--
• 1000 cc w/ 20 units of PIT; 100-125 cc/hr • mother will usually get 2 bags |
|
|
giving report to PP RN
|
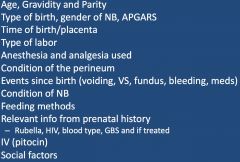
|

