![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
|
|
|
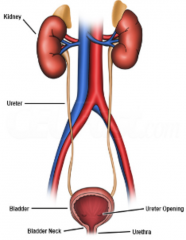
What is the function of the ureters? What forces transport urine through the ureters? |
transportsurine from the renal pelvis of each kidney to the urinary bladder persistalticcontraction of smooth muscle in the ureter walls, and to a lesserdegree, hydrostatic pressure and gravity |
|
|
What prevents infection in the ureters? |
- primitive valve - Pressureproduced when the bladder is full presses against the opening, sealing the bladder off from the ureters |
|
|
What are the three layers of the ureters? |
-mucosa made of transitional (variable) epithelium (deep) -intermediate muscularis made of inner longitudinal and outer circularlayer of smooth muscle. - superficialadventitia made of connective tissue and contains blood vessels,lymphatic vessels and nerves for the mucosa and muscularis. |
|
|
Describe the structure of the bladder |
-hollow, distensible and muscular organ -anterior to the rectum in males; anterior to the vagina in females -it is smaller in females due to the superior uterus -the floor of the urinary bladder contains a triangular region calledthe trigone (with the point facing forward). The two posterior pointssignify the two ureteral openings. The single, anterior point, is theopening to the urethra (the internal urethral orifice) - hasrugae (folds) which allow distension of the bladder. |
|
|
Describe the micturition reflex |
- involves voluntary andinvoluntary contractions - when the volume exceeds200-400-ml, stretch receptors relay nerve impulses to the spinal cord,and into the micturition centre in the sacral spinal cord (S2 andS3). This triggers the micturition reflex: (1) parasympatheticimpulses propagate to the wall of the urinary bladder and internalurethral sphincter (2) the impulses causethe detrusor muscle of the muscularis to contract and the internalurethral sphincter to relax (3)at the same time, the micturition centre inhibits the motor neuronswhich innervate the skeletal muscle of the external urethralsphincter (4)overall, contraction of the urinary bladder and relaxation of thesphincters causes urination |
|
|
What is the difference between the male and female urethra? |
Female -female urethra is much shorter (4cm vs 20cm) -the wall of the female urethra contains a deep mucosa and asuperficial muscularis (circular muscle) -near the urinary bladder, the urethra is made of transitionalepithelium; near the external urethral orifice, the epithelium ismade of non-keratinised stratified sqaumous epithelium Males - urethra in males alsodischarges semen - passes through theprostate - composed of a deepmucosa and a superficial muscularis. The muscularis has threeregions: prostatic urethra (passes through prostate), the membranousurethra (passes through the deep muscles of the peritoneum(shortest)), and the spongy urethra (passes through penis (longest)). -prostatic urethra contains (1) ducts that transport secretions fromthe prostate, and (2) seminal vesicles (holdsthe liquid that mixes with sperm to form semen)andvas deferens (duct which carries sperm). - various glands in thespongy urethra secrete alkaline substances to neutralise the acidityof the urethra, and mucous to produce lubrication for intercourse. |
|
|
Give 8 functions of the kidney |
(1)regulation of blood ions: sodiun, potassium, calcium, chloride andphosphate (2)regulation of blood pH: done by regulating excretion of hydrogen ionsand conservation of bicarbonate ions (3)regulation of blood volume: done by regulating water (4)regulating BP: release of renin activates therenin-angiotensin-aldosterone system, causing increasedvasoconstriction and reabsorption of water (blood volume) (5)Regulation of blood osmolarity (number of dissolved particles perlitre): regulates water loss and solutes individually – thus beingableto regulate osmolarity. (6)Hormone production: produced calcitrol (active vitamin D) for theregulation of calcium, and erythropoietin for the production of RBCs (7)Regulates blood glucose: can use glutamine for gluconeogenesis andrelease new glucose into the blood (8)excretion of wastes and foreign substances: e.g. urea, ammonia,bilirubin, creatinine and uric acid |
|
|
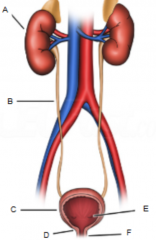
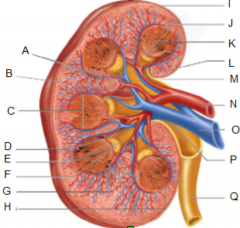
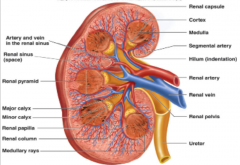
Describe the external, macroscopic anatomy of the kidneys |
-bean-shaped, retroperitoneal organs -partially protected by the 11th and 12th ribs -each kidney contains a hilum with blood and lymphatic vessels,nerves, and a ureter-the kidneys have three layers :- a deep renal capsule: made of irregular connective tissue; continuouswith the outside of the urethra; provides a barrier for protection -a intermediate adipose capsule: fatty tissue; holds kidney inposition and provides protection -a superficial renal fascia: irregular connective tissue; anchorskidney into position |
|
|
|
|
|
Describe the passage of blood flow through the kidney |

|
|
|
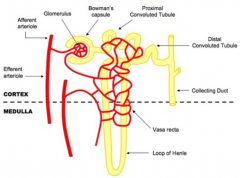
Draw and label a nephron |
|
|
|
What are the two types of nephron? What is the difference between them? |
- cortical and juxta medullary - cortical nephrons are confined to the cortex and have short loop's of Henle. They also do not have a thick ascending limb - juxtamedullary nephrons have longer loops which extend in to the medulla. They have a thick ascending limb - most nephrons are cortical (85%) |
|
|
Name 2 important cell types in the collecting duct and describe their function |
- principal cells andintercalated cells. - Principal cells have receptors for antidiuretichormone and aldosterone - intercalated cells are involved in blood pHhomeostasis. |
|
|
Describe the structure and function of the glomerulus |
- glomerular capillariesand the podocytes (visceral layer) form the filtration membrane - the filtration membraneis leaky. Allows the filtration of water and small solutes. Bloodcells, platelets and large proteins are too large to be filtered. - substances are filteredacross three barriers: glomerular endothelial cells, the basal laminaand a filtration slit formed by podocytes -glomerular endothelial cells have fenestrations and are very leaky –let most solutes through but not blood cells and platelets.Contractile mesangial cells help to regulate the amount filtration. -basal lamina has collagen fibres and proteoglycans in a glycoproteinmatrix – the negative charges in the matrix prevent larger,negatively charged proteins -slit membrane is formed by spaces between extension of podocytescalled pedicles. They prevent filtraiton of medium sized proteins |
|
|
Describe the three layers of the filtration membrane in glomerulus |
|
|
|
What three factors determine glomerular filtration rate? |
(1) Glomerular bloodhydrostatic pressure (GBHP): pressure in the glomerilar capillaries(increase) (2) Capsular hydrostaticpressure (CHP): pressure of fluid already within Bowman's space andrenal tubule (decrease) (3) Blood colloid osmoticpressure (BCOP): caused by the presence of proteins such as albumin,globulins, and fibrinogen in the blood plasma (decrease) |
|
|
What is glomerular filtration rate? |
total amount of filtrateproduced by all renal corpuscles in both kidneys per minute |
|
|
What are the three main mechanisms for adjusting GFR? |
- renal autoegulation e.g. stretch receptors and chemical receptors (macula densa) to adjust vessel diameter - neural regulation e.g. sympathetic stimulation causing noradrenaline-induced vasoconstriction - hormonal e.g. angiotensin II (decrease), atrial natriuretic peptide (increase) |
|
|
Briefly describe the two types of reabsorption which occur |
-when reabsorption occurs inbetween tubule cells it is called paracellular reabsorption and occurthrough leaky tight junctions - when reabsorptionoccurs through tubule cells it is called transcellular reabsorption - reabsorption of solutes through tubule cells is enabled by symporters and antiporters. Flow is one-way. - water follows by obligatory reabsorption (osmosis), or facultative reabsorption (using energy) |
|
|
Describe reabsorption in the PCT |
- most of the solute andwater reabsorption occur in the proximal convoluted tubule. - most reabsorptioninvolves sodium via symports and antiports - different types ofsodium sodium symporter bring glucose, amino aicds, lactic acid,water-soluble vitamins and other nutrients along with sodium. A majorone is the sodium-glucose symporter in the apical membrane. It uses 2Na for one glucose. The glucose then leaves the tubule cell viaATP-driven facilitated diffusion. - as water leaves theproximal convoluted tubule, the concentration of ion increases. Thismeans that remaining solutes – notably, chlorides, potassiums,calciums, and magnesiums – flow by diffusion into the (second halfof the) proximal convoluted tubule. Large amounts of negative Cl-flows into the tubule cells – promoting diffusion of positivelycharged potassium, calcium and magnesium. - also susceptible to regulatioon by hormones e.g. renin and ANP - overall, concentration begins to increase |
|
|
Describe reabsorption in the descending loop of Henle |
- osmolarity of the tubularfluid is similar to that of the blood because thereabsorption of water has occurred at a similar pace. - water begins to be reabsorbed into the peritubular fluids by obiligatory reaborption |
|
|
Describe reabsorption in the ascending loop of Henle |
- impermeable to solutes and water - Na+ and Cl- actively transported out of the tubule by sodium-potassium-(2x)chloridesymporters, reducing the osmolarity of the tubular fluid. Concentration of urea therefore increases in the tubules |
|
|
Describe reabsorption in the DCT and collecting duct |
- 80% of water has been reabsorbed by this point. A further 10-15% occurs in the DCT - Na+ and Cl- are also actively reabsorbed by Na-Cl symporters - Ca2+ reabsorption is regulated by Parathyroid Hormone - osmotic concentration of the tubular fluid in the collecting duct is fine-tuned by action of aldosterone, ADH, and ANP e.g. insertion aquaporin 2 channels for reabsorption |
|
|
Describe counter current multiplication |
- due tosodium-potassium-(2x)chloride symporters in the thick ascending limb,and the fact that tubules here are impermeable to water, there is abuild up of solutes and ions in the interstitial fluid of themedulla. It is this build up of ions which produces the gradient inthe medulla – about 300 milliosmoles/L higher up in the medulla,and about 1200 milliosmiles/L deeper in the medulla. - the descending limb ispermeable to water but relatively impermeable to solutes – excepturea. As such, water is increasingly reabsorbed as it moves down thedescending tubule, due to the osmotic gradient produced by the thickascending limb. This makes the inside of the tubule increasinglyconcentrated. - the collecting duct(and distal convoluted tubule) have receptors for antidiuretichormone. ADH increases the permeability of the tubules here, causingwater to leave the tubules through osmosis. As the water leaves, theconcentration of urea increases. However, the cell in the ducts arepermeable to urea, so they also become reabsorbed. - the build up urea inthe interstitial fluid causes some of it to diffuse into thedescending and thin ascending limb. The urea remains in the lumen asit cannot diffuse through the cells of the thick ascending limb,distal convoluted tubule and cortical portion of the collection duct– UNTIL it gets to the more distal regions of the collection duct. - the above means thaturea is constantly being recycled and contributing to the osmoticgradient in the medulla. By changing the amount of water which isable to be absorbed by using ADH, increasing amounts of water areable to leave the tubules – producing increasingly concentratedurine as it moves down the collection duct. |
|
|
What is the function of the prostate gland? |
-secretes a milky, slightly acidic fluid (6.5) -secretion contains various substances; (1)citric acid which is used by sperm for the citric acid cycle (2)proteolytic enzymes e.g. prostate specific antigen, pepsinogen,lysozyme, amylase and hyalurinidase (3)secretes acid phosphate. Has a function in countering tumourogenesis:dehosphorylates phosphotyrosine residues in prostate cancer cells.Can subsequently be used as a biomarker for prostatic cancer. Hasalso been shown to be a far better therapy for chronic pain thanmorphine. (4)contains seminalplasmin, an antibiotic which can reduce the number ofbacteria in semen and in the lower vaginal tract (5)makes up about 25% of semen and contributes to sperm motility andviabiity |
|
|
What is benign prostatic hyperpllasia and what causes it? |
-a non-neoplastic lesion - aetiology is driven bydihydrotestosterone, which acts as a transcription regulator topromote growth and cell survival |
|
|
Where does BPH originate and who is affected by it? |
- begins in theperiurethral (transitional zone) and is commonly a cause of symptomsfrom 60 onwards. ~50-75% of men aged 80 onwards will have BPH. |
|
|
What are the symptoms of BPH and what causes them? |
- primary symptoms arecaused by the inflammation of the prostate, and the hyperplasticnodules impinging on the urethra - involvement of theperiuretheral zone also interferes with sphincter function - main symptoms arehesitancy, poor prolonged flow, and sensation of incomplete emptying - the following may alsooccur, though are not specific to BPH; urinary frequency, urgency tourinate and urge incontinence - in some cases theobstruction can lead to distension of the urinary bowel whichrequires draining with a catheter |
|
|
Give 10 criteria required to implement a screening programme |
-should be an important health problem -Epidemiology and natural history of the disease needs to be suitablyunderstood, including development from latent to declared disease,and there should be detectable risk factors, disease markers, latentperiod (or early symptomatic stage. -cost effective primary prevention strategies should have beenimplemented as far as practical. -if the carrier of a mutation are identified through screening, theirnatural history should be understood – including psychologicalimplications -screening process needs to be simple, safe, precise and validated -distribution of test values for a target population should be known,with a suitable cot-off level defined and agreed -test should be acceptable to the population -should be an agreed policy on further diagnosis and intervention, andon the choices available to the patient -if the disease is base on genetic mutation, the mutations which arebeing screened for should be clearly determined. - should be an effectivetreatment or intervention for those with early detection, withevidence showing that early intervention improves outcomes. - there should be agreedevidence regarding which patients should receive treatment, and thetype of treatment they should receive - clinical management andtreatment strategies should be optimised prior commencing a screeningprogramme - should be evidence fromhigh-quality random controlled trials that the screening programme iseffective and at reducing morbidity and mortality. When the screeningis designed solely to provide information for the patient to make adecision (e.g. screening mothers for Down's syndrome, cystic fibrosiscarrier status), the test needs to be subject to high-qualityrandomised controlled trials. The results of the test must be ofvalue to the patient and understandable. - there should beevidence that the screening test – in its entirety – isclinically, socially and ethically acceptable to the healthprofessionals and the public. - the benefit of thescreening test/process should outweigh any physical or psychologicalharm - the cost of thescreening process should be balanced against other options available(i.e. cost-effective) - a plan needs to be inplace for monitoring and managing the screening process, with anagreed set of quality assurance standards. - adequate staff andfacilities for diagnosis, treatment and management, should beavailable prior to commencing screening - other options regardinghealthcare should be considered to ensure that the treatment suppliedis most cost-effective. - implications ofscreening, based on evidence, should be clearly communicated to thepatient to allow them to make an informed decision. |
|
|
How would you screen of BPH? |
- digital rectal exam –check the size and firmness of the prostate - urinalysis – look forurinary tract infection which may correlate with symptoms - Prostate SpecificAntigen (PSA) test to assess potential involvement of neoplasia |

