![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
258 Cards in this Set
- Front
- Back
- 3rd side (hint)
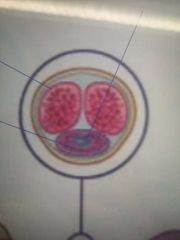
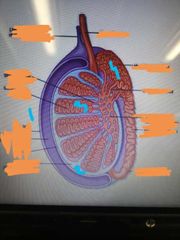
Annotate the transverse section of a penis: |
-The eyes are the corpus cavernosa -The purple of the mouth is the corpus spongiosum -the blue part is the ejaculatory duct |
|
|
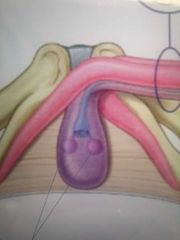
What are these: |
Bulbourethral glands |
|
|
|
What do bulbourethral glands do? |
Produce pre-ejaculate to neutralise the acidity of the urethra to protect the sperm in passage |
|
|
|
What are the corpus cavernosa made up of? |
Spongy erectile tissue |
|
|
|
What arteries are running through the corpora cavernosa? |
Cavernosa arteries |
|
|
|
What facilitates the erection? |
The two corpora cavernosa |
|
|
|
What is the function of the single corpus spongiosum? |
To prevent the the urethra from pinching closed in erection therefore maintain the urethra as a viable channel for ejaculation |
|
|
|
What is another word for foreskin? |
Prepuce |
|
|
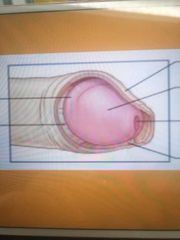
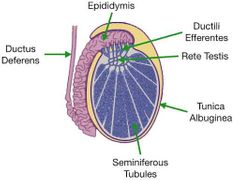
Label this diagram: |
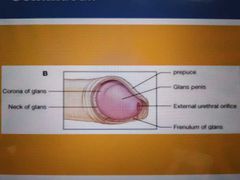
|
|
|
|
What is the body of the penis is covered by? |
Skin |
|
|
|
What is the tip of the body of the penis covered by? |
Glans penis |
|
|
|
What is the name of the sagittal slit at the tip of the glans? |
The external urethral orifice |
|
|
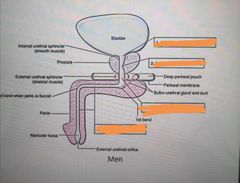
Name the blanks: |
1) preprostatic part of urethra 2) prostatic part of urethra 3) membranous part of urethra 4) spongy part of urethra |
|
|
|
How does an erection occur? |
When the corpora cavernosa becomes engorged with Venous blood due to parasympathetic |
|
|
|
What sort of control is an erection under? |
Autonomic control |
|
|
|
Describe the physiology of an erection happening |
Acetylcholine is released upon stimulation which releases nitric oxide from endothelial cells in the trabecular arteries.
Nitric oxide diffuses to the smooth muscle of the arteries (trabecular smooth muscle) acting as a vasodilation agent.
The arteries dilate, filling the corpus spongiosum and corpora cavernosa with blood.
Simultaneously muscles compresses the veins of the corpora cavernosa, limiting the Venous drainage of blood |
|
|
|
What is the innervation causing acetylcholine release? |
Parasympathetic branches from the Sacral plexus |
|
|
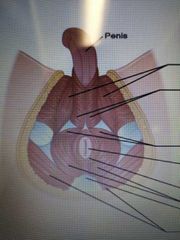
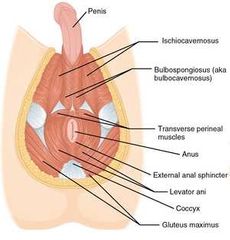
Label all the parts of the male pelvic floor:
|
|
|
|
|
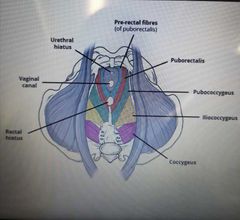
What are the 3 holes named in the female pelvic floor? |
Urethral hiatus Vaginal canal Rectal hiatus |
|
|
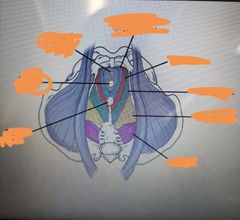
Name the parts of the female pelvic floor:
|
|
|
|
|
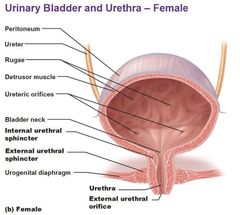
How many sphincters do male and females have? |
2 - internal urethral sphincters and external urethral sphincters |
|
|
|
What is the function of the urethral sphincters? |
Inhibit the release of urine. In males, the internal urethral sphincter functions to prevent reflux of seminal fluids into the male bladder during ejaculation |
|
|
|
What is the female sphincter made up of? |
3 parts:
Sphincter urethrae Urethrovaginal muscle Compressor urethra |
|
|
Label the different parts of the external female genitalia:
|
|
|
|
|
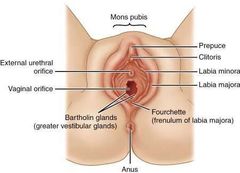
How is the Mon pubis formed? |
By the fusion of the labia majors |
|
|
|
What is the labia majora? Where is it embryologically derived? |
Two hair bearing external skin folds. Derived from the labioscrotal swellings |
|
|
|
What is labia minora? What do they merge to form? |
Two hairless fils of skin which lie within the labia majora. They merge posteriorly to form the fourchette. |
|
|
|
Where is the labia minora embryologically derived from? |
The urethral folds |
|
|
|
What is the vestibule? |
Area enclosed by the labia minora. Contains the opening to the vagina and urethra |
|
|
|
What are bartholin's glands? |
Secrete lubricating mucus from small ducts during sexual arousal. Located in either side of the Vaginal oriface |
|
|
|
What is the clitoris formed from? What happens during sexual stimulation? |
Erectile corpora cavernosa tissue which becomes engorged with blood during sexual stimulation |
|
|
|
Where is the clitoris embryologically derived from? |
Genital tubercle |
|
|
|
What is sexual differentiation? |
The process of development of differences between males and females from an undifferentiated Zygote |
|
|
|
What determines testicular formation? |
A gene in the sex determining region of the short arm of Y, known as SRY leads to the formation of testis determining factor (TDF), which binds to DNA and induces differentiation of cells derived from the genital ridges into the testes |
|
|
|
By what point of gestation can the gonads be distinguished? |
6-8 weeks of gestation |
|
|
|
Where do the testes get transferred from to where? What time of the pregnancy does this happen? |
From the Lumbar area to the future scrotum. This happens between the 3rd month and the end of the pregnancy |
|
|
|
How is the transfer of the testes into the scrotum region brought around? |
Through a combination of growth processes and hormonal influences |
|
|
|
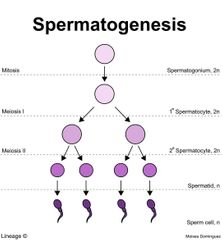
What is Spermatogenesis? |
Process by which spermatoza are produced from spermatogonial stem cells through mitosis and meiosis |
|
|
|
How long does it take for sperm to form? |
74 days at the beginning |
|
|
|
Where are sperm produced? |
Seminiferous tubules |
|
|
|
Where are sperm cells matured and stored until ejaculation? |
Epididymis |
|
|
|
Describe the pathway of testosterone production |
Hypothalamus releases GnRH So Anterior pituitary releases LH So LH causes Leydig cells to produce testosterone |
|
|
|
Describe process of sperm production? What other hormone is produced alongside sperm from the cells? |
Hypothalamus releases GnRH So Anterior pituitary releases FSH So Sertoli cells stimulate Spermatogenesis and releases inhibin |
|
|
|
What does testosterone do? |
Stimulates sertoli cells and stimulates reproductive tract and other organs |
|
|
|
What does testosterone inhibit? |
Production of LH from anterior pituitary. And production of the GnRH from the hypothalamus. |
|
|
|
What does inhibin inhibit? |
FSH production from the anterior pituitary GnRH production from the hypothalamus |
|
|
Label the important parts: |
1- tunica vaginalis (like the peritonium but thrown over the testes 2- tunica albuginea surrounds the testis and extends inwards following lobules 3- eachlobule contains seminiferous tubules 4- head of epididymis |
|
|
|
What does the seminiferous tubules contain? |
Spermatogenic cells and sertoli cells |
|
|
|
Describe the pathways of a sperm out of the testes |
Produced in the sertoli cells and released into the lumen of the seminiferous tubule. Goes to the rete testis in mediastinum testis. Through efferent ductules to head of epididymis. Through to vas deferens/ ductus deference |
|
|
|
What are leydig cells also known as? |
Interstitial cells |
|
|
|
Where are the leydig cells found? |
On the outside of the sertoli cells between the seminiferous tubules in the interstitium (a fluid filled space found found between cells or walls) |
|
|
|
What does testosterone do in males? |
Stimulates development of male characteristics Increases muscle growth, bone growth and thickness of skin Stimulates new blood cells |
|
|
|
What type of cells are sertoli cells |
Simple columnar cells |
|
|
|
Describe process of Spermatogenesis |
Spermatogonium are germ cells present around the circumference of the cylindrical, tube like sertoli cells. These sertoli cells are linked together end to end to form a lumen in the middle.
The spermatogonium undergo mitosis to form primary spermatocytes. Then meiosis 1 (forming secondary spermatocyte) and meiosis 2 to form a spermatid. The point where the sperm has a head but no tail it is called a spermatid
When the sperm cell has been fully formed it's called a spermatoza. At this point the sperm can't penetrate to the surface anymore so it has to pass down through the lumen. This sperm is completely matured and is stored in the epididymis until ejaculation. |
|
|
|
The sertoli cells maintain the environment necessary for development and maturation of the sperm via what? |
The blood testis barrier |
|
|
|
What is the blood testis barrier? |
It stops certain things entering the sertoli cells, limiting it to only things like testosterone and substances which are necessary for development and maturation of gamete |
|
|
|
What do the sertoli cells secrete? |
Substances that initiate meiosis Secrete supporting testicular fluid Secrete androgen-binding protein (ABP) Secrete anti-mullerian hormone Inhibin and activin |
|
|
|
What does androgen binding protein do? |
Binds and concentrates testosterone in close proximity to the developing gametes |
|
|
|
What do inhibin and activin do? |
Inhibit and activate FSH secretion from the pituitary gland |
|
|
|
What does the anti-mullerian hormone do? |
Causes deterioration of the mullerian duct |
|
|
|
How are the spermatids protected from the immune system? |
Blood testis barrier |
|
|
|
What is the outermost layer of the sertoli cell? |
Basal lamina |
|
|
|
Difference between spermatids and spermatozone? |
The spermatids don't have a tail |
|
|
|
What is the name of the tubule that carries away sperm from the epididymis? |
Vas deferens |
|
|
|
What is the ejaculatory duct? |
Point of union of vas deferens/ ductus deferens with the duct of the seminal vesicle |

|
|
|
What is the seminal vesicle? What cells does it have? |
Lateral of the vas deferens. Pouch shaped and it is lined with the secretary and goblet cells |
|
|
|
What do the seminal vesicles secrete? |
Seminal fluid which contains fructose, citric acid, prostaglandins and fibrinogen |
|
|
|
Describe process of sperm emission |
1) vas deferens empties sperm into ejaculatory duct and seminal vesicles empty seminal fluid into the ejaculatory duct 2) the sperm and seminal fluid goes through the ejaculatory duct through the prostate. 3) Through the bulbourethral glands (cowpers's glands), then through the urethra |
|
|
|
What does prostate add to the ejaculation? |
Nutrients and enzymes to activate sperm to the semen along with PSA |
|
|
|
What does bulbourethral glands add to the semen? |
Secretes an alkaline fluid into the urethra during arousal to protect the sperm. Also secretes mucus that protects and lubricated the end of the penis and lining of the urethra |

|
|
|
Show the pathways of semen |

|
|
|
|
What are the two phases of sperm emission? |
Emission stage Ejaculation proper |
|
|
|
What happens during the emission stage? |
Sperm are moved from the testes and epididymis to the beginning of the urethra |
|
|
|
What happens during ejaculation proper? |
Semen is moved through urethra and expelled from the body |
|
|
|
What are the muscles that are used in the emission phase? |
Muscles around the epididymis and ductus deferens contract to push sperm into the prostate and the urethra |
|
|
|
What are the muscles involved in the ejaculation proper? |
Semen is expelled by the spasmodic contractions of the bulbocavernosus muscle which encircles corpus spongiosum |
|
|
|
What type of reaction is it when ejaculation starts? |
A reflex reaction - can't be voluntarily interrupted |
|
|
|
What is a primary oocyte? Where is it developed? |
Diploid cell In the foetus |
|
|
|
What happens to most of the primary oocyte by birth? |
Break down |
|
|
|
Follicular development is arrested at what stage? Till when? |
Prophase of Meiosis I Until sexual maturity |
|
|
|
What triggers puberty? |
LH and FSH release Follicular development is restarted, and the primordial follicles begin to mature. |
|
|
|
How many cells mature at once? |
About 20 but only one matures fully and undergoes ovulation |
|
|
|
What hormone causes follicular maturation? |
FSH |
|
|
|
What are the names of the oocytes through the ovarian cycle? |
Primordial follicle Primary follicle Secondary Tertiary Pre ovulatory |
|
|
|
What is the structure of the primordial follicle? |
A primary oocyte (arrested in prophase 1) surrounding by a layer of granulosa cells |
|
|
|
How is the primordial follicle turned into the primary follicle? |
Female hits puberty: A surge of FSH happens and meiosis 1 is restarted. |
|
|
|
Describe the structure of the primary follicle |
A secondary oocyte surrounded by granulosa cells. A Zona pelludica forms between the oocyte and the granulosa cells. A basal lamina forms on the outside of the granulosa cells |
|
|
|
In the primary follicle, what shape are the granulosa cells? |
Cuboidal |
|
|
|
How does the secondary follicle form from the primary follicle? |
Granulosa cells proliferate producing multiple layers around the oocyte. A outer theca layer forms. |
|
|
|
What are the co-responding phase of the follicular and Luteal phase in terms of the uterine cycle? |
Follicular = proliferative phase in the uterine cycle
Luteal = secretory phase in the uterine cycle |
|
|
|
What is the menstrual phase in terms of dates? |
Days 1-5 |
|
|
|
What happens in the overies during the menstrual phase? |
Oestrogen begins to rise, and primordial follicles begin to mature |
|
|
|
Which hormone causes the lining of the endometrium to become thicker? |
Oestrogen |
|
|
|
Time for pronephros |
Early week 4 |
|
|
|
Time for mesonephros? |
Late week 4 |
|
|
|
Time for metanephros? |
Week 5 |
|
|
|
Time the metanephros blastomes and utereic buds appear? |
Week 4-8 |
|
|
|
Time for kidney ascent? |
Week 4-8 |
|
|
|
Mesonephros as functioning kidney |
Weeks 6-10 |
|
|
|
Time the collecting duct system is complete |
28-40 |
|
|
|
Time during which the prostate, seminal vesicles and bulbourethral glands develop |
Week 8-13 |
|
|
|
Definitive kidney begins working? |
Week 14 |
|
|
|
Time the gubernaculum draws the testix down into the scrotum |
Week 28-40 |
|
|
|
How does the counter current multiplier system work? |
-descending limb is permeable to water -ascending limb actively transports sodium out into the medulla -as more sodium is transported out more water is diffused into the medulla which makes the filterate more hypertonic which means more sodium is transported out -leads to multiplication effect |
|
|
|
What is the name of the blood vessels which remove the water from the medulla? |
Vasa recta |
|
|
|
What is the secondary function of the vasa recta? |
Keeps the salt in the medulla to maintain the concentration gradient |
|
|
|
What is the max osmolality? Where is this reached? |
1200 mOsm/1 Lowest part of the loop of Henley |
|
|
|
What is the normal osmolality of the blood? |
300 mOsm/ 1 |
|
|
|
Countercurrent multiplier system is a type of what Feedback? |
Positive |
|
|
|
Where is renin released from in the kidneys? |
Juxtaglomerlus cells |
|
|
|
What does the RAAS system do? |
Increase blood pressure in response to low blood pressure |
|
|
|
Describe RAAS pathway |
-juxtaglomerlus cells in the kidneys detect low BP and release renin -the liver releases angiotensinogen -renin converts angiotensinogen into angiotensin 1 (inactive) -ACE (angiotensin converting enzyme) is released from the lungs -it converts angiotensin 1 into angiotensin 2 (active) -this acts on the Adrenal gland and causes aldosterone to be released
|
|
|
|
What part of the Adrenal gland releases the aldosterone? |
Zona glomerulas |
|
|
|
What does aldosterone do? (steroid hormone) where does it do this? |
Increased Na+ resorption from distal tubules and collecting ducts of the kidneys. So more water is pulled out and reabsorbed.
Increases potassium excretion so more potassium is urinated out |
|
|
|
Angiotensin 2 also increased BP by 2 other ways. Name them |
Through stimulating ADH/ vasopressin secretion
Through vasoconstriction of the arterioles |
|
|
|
Why is the descending limb permeable to water? |
Due to aquaporin channels |
|
|
|
How does angiotensin 2 vasoconstrict arterioles |
Binds to AT1-R (receptor) in the surface of vascular endothelium |
|
|
|
What is the secondary function of ACE towards increasing bp |
ACE degenerates bradykinin. Which is a molecule that synthesises NO. And NO is a vasodilator |
|
|
|
What Feedback mechanism does RAAS use? |
Negative feedback |
|
|
|
What is the function of the kidneys? |
-Filter the blood -Make erythropoietin which make red blood cells -Vitamin D metabolism |
|
|
|
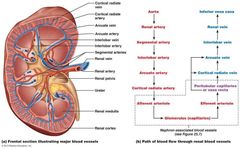
Which artery goes to the kidneys? |
Renal artery |
|
|
|
Pathway of the blood away from kidneys? |
Venous blood Renal vein Inferior cava |
|
|
|
Pathway of urine formed from kidneys? |
Kidneys Ureter Bladder Urethra |
|
|
|
Where are the kidneys located in terms of the vertebrae? Where are they found in regards to the peritonium |
T12 - L3 Behind the peritoneum (are a Retroperitoneal structure) |
|
|
|
Which kidney is lower than the other and why? |
Right is lower Because liver is on the right |
|
|
|
What is the pathways of arteriol blood supply of the kidneys? |
Aorta Renal artery Segmental artery Interlobar artery Arcuate artery Cortical radiate artery Afferent arteriole Glomerulus Efferent arteriole Vasa recta (peritubular capillaries) |
|
|
|
What is the Venous pathway of the kidneys? |
From (vasa recta) Cortical radiate vein Arcuate vein Interlobar vein Renal vein Inferior vena cava |
|
|
|
Which artery doesn't have an associating vein? |
Segmental vein |
|
|
|
Label all the arrows for arteriol and Venous blood supply |
|
|
|
|
What do theca cells respond? What do they produce? |
The theca cells surround the secondary follicle respond to LH and produce androgen |
|
|
|
What do granulosa cells respond to? What do they produce? |
FSH and produce oestrogen from androgen produced by theca cells |
|
|
|
How do granulosa cells produce oestrogen? |
By converting androgen (synthesised from acetate and cholesterol) into oestrogen using the enzyme aromatase |
|
|
|
Describe the formation of the tertiary follicle |
During the transition from secondary to tertiary follicle, Meiosis 1 ends and meiosis 2 starts, arresting in metaphase 2 until fertilisation.
Formation of Antral follicle occurs in the most dominant secondary follicle. Cumulus oophorous forms.
|
|
|
|
Which follicle is the most dominant? |
The one that expresses the most FSH receptors and LH receptors |
|
|
|
What parts of the ovarian cycle is the Antral phase? |
The tertiary follicle to preovulatory follicle |
|
|
|
Hormonally what happens in the Antral phase? |
-FSH binds to granulosa cells and they convert androgen into oestrogen. This in turn causes proliferation of granulosa cells and thus a high level of oestrogen circulation.
-high levels of FSH causes LH receptors to appear of granulosa cells (they already have FSH receptors)
-LH binds to theca cells and granulosa cells to promote further oestrogen production
-this causes a surge in LH right before ovulation |
|
|
|
Summarise the hormones involved in the uterine cycle: |
1) GNRH ➡️LH and FSH production 2) LH stimulates theca➡ androgen 3) When FSH binds to granulosa, they take up androgen and convert them into oestrogen 4) oestrogen stimulates release of GnRH so more LH is releases. Also causes receptors on granulosa cells to appear 5) LH surge triggers ovulation |
|
|
|
What is the follical that is remaining now called? |
Corpus luteum |
|
|
|
What does corpus luteum produce? What is it stimulated by to produce this? |
Progesterone Oestrogen Relaxin Inhibin
Stimulated by LH |
|
|
|
What happens to corpus luteum eventually? |
It's broken down and corpus albicans is formed |
|
|
|
What is day 0 in menstrual cycle? |
The period |
|
|
|
What day does ovulation occur? |
Day 14 |
|
|
|
What are the 2 phases of the menstrual cycle? |
The follicular phase Luteal phase |
|
|
|
What is the range of dates for the follicular phase? |
1-13 |
|
|
|
What is the range of dates for the Luteal phase? |
15-28 |
|
|
|
The menstrual cycle can also be known as? |
The uterine cycle |
|
|
|
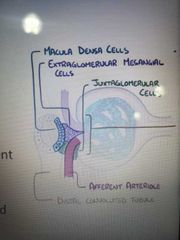
Where are the macula densa cells located? |
DCT |
|
|
|
What is the function of macula densa cells? |
They sense low Na/Cl levels and send signal to the juxtaglomerular cells |
|
|
|
Where are the juxtaglomerlar cells located? |
The afferent arteriole |
|
|
|
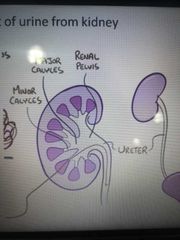
What is the exit pathway of urine from the kidney? |
-Urine leaves nephrons via collecting duct -drains into minor calyx -drains into major calyx -drains into Renal pelvis -flows through ureter -stored in bladder |
|
|
|
What is the name of the entry and exit point in the kidney for everything? |
Hilum |
|
|
|
What does the hilum allow entry and exit into the kidney for? |
Ureter Renal arteries Renal veins Lymphatics Nerves |
|
|
|
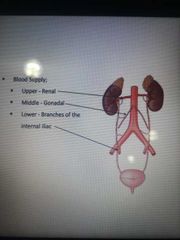
What is the blood supply to the ureter? |
3 arteries;
-Renal -gonadal -branches of the internal iliac |
|
|
|
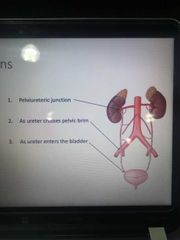
What are the 3 ureteric constrictions? |
Top = pelviureteric junctions Middle = across pelvic brim End = ureter entering brim |
|
|
|
Why is it important to know the ureteric constrictions? |
These are spots where kidney stones can lodge |
|
|
Label the anterior relations of the kidneys: |
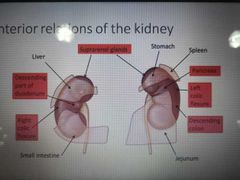
|
|
|
|
Through which mechanisms is Renal blood flow automatically regulated? (meaning even if the blood pressure of the body is altering, what mechanisms maintain a regular Renal blood pressure?) |
These are intrinsic: only effect kidney -Myogenic -Tubuloglomerular
These are extrinsic: effect whole body -Hormonal -Neural |
|
|
|
What does intrinsic mean? |
Directly regulates GFR despite moderate changes in BP (80-180 mm Hg) |
|
|
|
What does extrinsic mean? |
Indirectly regulates GFR by maintain systemic B. P |
|
|
|
Describe the myogenic autoregulation of GFR |
1) BP increases, GFR increases 2) Stretching in afferent arteriole 3) In response smooth muscle contracts, narrowing afferent arteriole 4) GFR decreases
|
The smooth muscle of the blood vessels reacts to the stretching of the muscle by opening ion channels, which cause the muscle to depolarize, leading to muscle contraction. This significantly reduces the volume of blood able to pass through the lumen, which reduces blood flow through the blood vessel. Alternatively when the smooth muscle in the blood vessel relaxes, the ion channels close, resulting in vasodilation of the blood vessel; this increases the rate of flow through the lumen. |
|
|
Describe the Tubuloglomerular mechanism of autoregulation? |
1) Macula densa detects high BP 2) Greater conc of Na+ and Cl- in filtrate as its had less time to be reabsorbed 3) Macula densa Inhibits release of NO from juxtaglomerular cells / causes NO release if GFR is too low |
|
|
|
Describe the hormonal mechanism? 2 ways |
Angiotensin II is a vasoconstrictor and narrows afferent and efferent arterioles, reducing Renal blood flow and as a result reducing GFR. Aldosterone causes Na+ reabsorption and water follows so blood volume increases
ANP (Arterial Natriuretic Peptide) triggers the relaxation of the glomerular mesangial cells, thus in creasing capillary SA and hence increasing Renal blood flow and GFR |
|
|
|
Describe the neural control in lower BP? |
1) baroreceptors in carotid and aorta detect high bp, sending signals to medulla 2) medulla sends signals via sympathetic fibres to kidneys to secrete Noraadrenaline 3) a-1 receptors detect this and cause vasoconstriction of afferent arteriole to maintain GFR |
|
|
|
What is the countercurrent multiplier system? |
A system designed to ensure that the Na+ Cl- is always lower in the Vas recta (blood) than in tubule. So the blood first travels past DCT and ascending limb where blood ion conc is low and so is tubule ion conc. By the time the blood arrives to descending limb where ion conc is high, the ion conc in vasa recta is also high. Encouraging water to move into capillary via osmosis |
|
|
|
What does the Renal capsule consist of? |
Glomerulus Bowman's capsule |
|
|
|
What is the difference in the lumen sizes between the afferent and efferent arteriole? |
Afferent arteriole is bigger |
|
|
|
What does the afferent arterioles increases lumen size mean for the glomerulas? |
There is increased osmotic pressure inside the glomerulas |
|
|
|
What are the 3 layers that make up the filtration bed of the capillaries in the Glomerulus? |
Lumen side -
Capillary endothelium Basement membrane Podocytes (specialised epithelium) |
|
|
|
How is the capillary endothelium leaky? How is the Podocytes leaky? |
It has large pores/ fenestrations
They form filtration slits |
|
|
|
How are Podocytes specialised? |
Modified epithelial cells which have footlike processes called pedicels. |
|
|
|
What are the types of movements of substances in the kidneys? |
Paracellular transport - movements through gaps between tightly packed epithelial cells (no channels or transporter required)
Transcellular movement - moving via membranes across the epithelial cells |
|
|
|
What molecules are reabsorbed at the PCT? |
100% of glucose 100% of amino acids 60-80% phosphate 66% K+, Na+, Cl-, H2O |
|
|
|
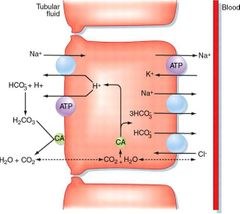
Which transporter are used to reabsorb at the PCT? |
Sodium - (glucose/amino acids/ Cl-) transporters out of the lumen into cells. All but Na+ passively diffusion into blood.
Na+/K+ ATPase to pump Na+ out of cells into blood
Na+/H+ antiporters
CO2 passively diffuses into cells, reacts with water to form ions. H+ moves into lumen and HCO3- into blood. Both using Na+ transporters |
|
|
|
Apical vs basolateral |
Apical the part of the membrane orientated towards the lumen of the PCT
Baso lateral is part of the membrane orientated towards the basement membrane |
|
|
|
What substance completely passively passes through the PCT into the interstitial fluid, then blood stream? |
Water Urea |
|
|
|
What is the only thing the thin descending limb of the loop of henle is permeable to? |
H2O |
|
|
|
Thin ascending limb of the loop of Henley permeability? |
Na+ and Cl- only These passively leave |
|
|
|
Thick ascending limb |
Na+, 2Cl-, K+ transporter brings these ions from lumen to cell. K+ diffuses back into lumen passively Cl- leave straight through the cell into blood Na+ is actively transported out of cell into lumen |
|
|
|
Sodium reabsorption percentages: |
PCT - 65% Loop of henle - 25% DCT and Collecting duct - remaining 10% but this is controlled by aldosterone |
|
|
|
What happens at the DCT and Collecting Duct? |
Aldosterone stimulats cells in DCT to transport Na+ into blood and K+ into lumen More Na+ = more water reuptaken increasing blood volume |
|
|
|
Where can a store of potassium be found in the nephron? |
DCT and Collecting Duct - waiting in case it needs to be exchanged for Na+ to allow it to re-enter the blood |
|
|
|
Which cells detect low BP (low fluid flow) or low Na+ concentration? |
Macula densa cells |
|
|
|
What other substances are secreted into the DCT from the capillaries? |
Ions Acids Drugs Toxins |
|
|
|
What is the name of the most distal part of the collecting tube? Feeds into the minor calyx? |
Papillary duct |
|
|
|
What is the normal composition of urine? |
96% water 2% Urea 2% : uric acid, creatinine, ions |
|
|
|
What is the principle or filtration? |
Use pressure to force fluids and solutes through a membrane |
|
|
|
Why is the volume of fluid filtered by the Renal corpuscle larger than in other blood capillaries? |
- Glomerulus capillaries have large surface area for filtration because they're long and extensive -membrane is thin and porous -efferent arteriole is smaller than afferent arteriole so capillary BP is high |
|
|
|
What cells in the glomerulus regulate how much surface area is available? |
Mesangial cells - when relaxed SA is max and glomerular filtration is high. When contracted, available SA decreased and glomerular filtration decreases |
|
|
|
Kidneys and pH balance: |
Due to resp: H+ is produced when CO2 joins with water. To overcome this the kidneys reabsorb HCO3- and excrete H+ and ammonium |
|
|
|
What does ADH do? |
Causes aquaporins 2 to appear in collecting duct for water reabsorption |
|
|
|
What is kidney secretion? |
Transfer of materials out of the blood into the urine Kidneys also secrete renin, Calcitriol and EPO |
|
|
|
What is GFR? |
How much fluid passes from the glomerulas into the Renal capsule in both kidneys per min |
|
|
|
What is the normal GFR? |
100- 125 ml / min |
|
|
|
What does a GFR of 0 mean? |
Kidneys failed - needs dialysis or will die |
|
|
|
What is the GFR like on healthy people? |
Constant - GFR is regulated regardless of blood pressure or fluid intake due to auto regulation |
|
|
|
What can be used to measure Renal function? |
Inulin (for true GFR) Creatinine (used for EGFR cos its produced by the body already in low levels) |
|
|
|
Why are inulin and creatinine good for measuring GFR? |
Aren't at all reabsorbed by the body |
|
|
|
How is inulin used to work out GFR? |
-inulin drip @ steady rate -measure blood inulin -measure urine inulin -time
Use inulin clearance via:
Urine conc x urine volume/ Plasma conc x time
= GFR |
|
|
|
How is creatinine eused to work out GFR? |
-is released by skeletal muscles -freely filtered at flomerulus -rougly = GFR -low GFR means high creatinine clearence |
|
|
|
Limitations of measuring creatinine |
-Need to collect urine for 24 hrs -Different dependent on muscle mass of people -age -sex -ethnicity -serum creatinine |
|
|
|
What is hypertonic, isotonic, hypotonic? |
Hyper- more water leaves Isotonic - neutral Hypo- more water enters |
|
|
|
Which type of epithelium lines the ureters and bladder? |
Transitional |
|
|
|
Which type of epithelium lined the endocervix? |
Simple columnar |
|
|
|
Which type of epithelium lines the vas deferens? |
Ciliated pseudostratified columnar epithelium |
|
|
|
Which type of epithelium lines the thin segment of the descending limb of the loop of henle? Also ascending |
Simple squamous |
|
|
|
Approximately what percentage of sodium, chloride and potassium is actively absorbed at the thick ascending loop of henle? |
25% |
|
|
|
What is a potent vasoconstrictor that causes rise in blood pressure? |
Angiotensin II |
|
|
|
Which hormone is both responsive to positive and negative feedback from the ovary and gonads as well as the anterior pituitary gland? |
GnRH |
|
|
|
What is a peptide hormone that stimulates the expression of LH receptors on granulosa cells? |
FSH |
|
|
|
During pregnancy, where is beta HCG produced? |
Placenta |
|
|
|
Which hormone produced by the corpus luteum relaxes the interpubic ligament and softens the cervix in Labour? |
Relaxin |
|
|
|
what is the mechanism by which blood pressure tends to rise in the last trimester of pregnancy? |
Increased plasma volume due to increased aldosterone production |
|
|
|
What level do the kidney hilum sit? Is the Renal vein or artery anterior? Is the left or right Renal vein longer? |
L1 Vein is anterior Left is longer due to position of IVC |
|
|
|
What does the Renal vein empty into? |
Inferior vena cava |
|
|
|
What are the cells located between glomerular capillaries? What is their function? |
Mesangial cells Changes SA of glomerular capillaries Keep the basement membrane free if aggregated proteins etc |
|
|
|
What is present between the filtration slits of the Podocytes? |
Slit diaphragm (final filtration) |
|
|
|
What is the ureter vasculature supplied by? |
Tetsicular/ ovarian arteries Common iliac internal iliac arteries |
|
|
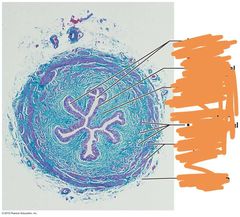
Histology of ureter: |
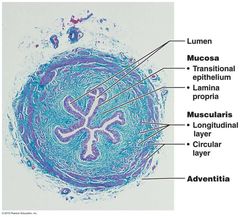
|
|
|
|
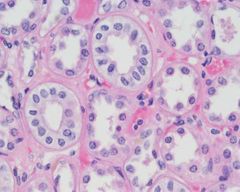
What are tubular cells? |
Renal tubular cells baso line the outside of Renal tubule |
|
|
|
What does it mean if: 1)clearence of a substance > inulin clearance 2)clearence of a substance < inulin clearence |
1) substance has been secreted by tubular cells 2) reabsorbed by tubular cells |
|
|
|
What are some basic kidney function? |
Erythropoietin secretion in response to hypoxia for red blood cell synthesis
Calcium regulation
Regulation of blood composition
Regulation of pH |
|
|
|
What are the two types of nephrons? |
Juxtamedullary nephrons - delve deeper into the Renal medulla so more water is reabsorbed (20-30% of nephrons). Cortical nephrons don't delve as deep into medulla so less waste ris reabsorbed |
|
|
|
How does the PCL regulate pH? |
By exchanging H+ for HCO3- in the filtrate Secreting NH3+ which combines with H+ and the NH4 is urinated out |
|
|
|
What is the PCT cell? |
Simple cuboidal epithelium with brush border (literally looks like toothbrush bristles) |
|
|
|
What causes the release ADH? |
Angiotensin 2
Posterior pituitary releases it in response to low blood Na+ by osmoreceotors |
|
|
|
What is proteinuria? |
Protein in the urea. Suggests damage to glomerulas |
|
|
|
Which ligaments hold male and female bladders in place? |
Male: puboprostatic Female: pubovesical |
|
|
|
What muscles in the bladder contract to bring around micturition? |
Detrusor muscles |
|
|
|
What type of cells lines DCT? |
Cuboidal cells |
|
|
|
What type of cells make the collecting duct? |
Columnar cells |
|
|
|
Where are the different types of aquaporins found? |
1- apically in the PCT and thin descending loop 2- ADH sensitive found apically in the collecting duct 3- found mainly on the basolateral side of the collecting duct 4- found on the inner medullary part of the basolateral collecting duct |
|
|
|
What does the mullerian duct form? |
Structures of the female reproductive tract |
|
|
|
What does the prostate convert testosterone into? Using what enzyme? |
Into DHT using 5-alpha reductase which is important in development of male genitalia - but increases risk of prostate cancer |
|
|
|
What does DHT cause? |
Prostate enlargement Body hair Hair loss and scalp recession |
|
|
|
What does oestrogen do? |
-promotes development of female reproductive structure -lower blood cholesterol -moderate levels in blood inhibits release of GnRH by hypothalamus |
|
|
|
What does progesterone do? |
-Works with oestrogen to maintain endometrium -prepares mammary glands for milk secretion -high levels of progesterone also Inhibits GnRH |
|
|
|
What does relaxin do? |
-Inhibits myometriun contractions and relaxes the uterus -allows increases flexibility of public symphysus and dilation of cervix during delivery of the baby |
|
|
|
What secretes Inhibin in females and what does it do? |
Secreted by granulosa cells of the dominant growing follicles and corpus luteum after ovulation
Inhibits secretion of FSH and LH and GNRH to ensure no more follicles can mature |
|
|
|
What produces HCG? |
Chorion of the embryo starting 8 days after fertilisation and stimulates secretion of corpus luteum |
|
|
|
What happens when there is no fertilisation? |
Without HCG stimulating CL, it turn into corpus albician and progesterone, Inhibin, oestrogen decrease. So GnRH, LH and FSH are no longer inhibited and rise again to start the cycle. The withdrawal of oestrogen and progesterone caused menstruation. |
|
|
|
What are the two major post ovulation hormones? What do they do? |
Progesterone Oestrogen
Maintain endometrium and get body ready for a pregnancy |
|
|
|
What is the major preovulation hormone? |
Oestrogen (estrogen causes production of more FSH, which caused more oestrogen production etc... Positive feedback) |
|
|
|
What 4 follicles recieve FSH? |
Primordial Primary Secondary Tertiary
(makes sense this is the follicular phase. After this, FSH is inhibited by Inhibin) |
|
|
|
What four follicles does LH supply? |
Secondary Tertiary Ovulation Corpus luteum (not to the follicles before because there was no LH receptors and Oestrogen inhibits LH production) |
|
|
|
Another hormone summary: |
Low levels of oestrogen and Inhibin Inhibits GnRH and associate hormones
High levels of estrogen without progesterone stimulates GnRH and associated hormones |
|
|
|
What causes morning sickness |
HCG |
|
|
|
What are the respiratory changes in pregnancy? |
Decreased residual volume Increases tidal volume Mild respiratory alkalosis |
|
|
|
GI changes in pregnancy |
Delayed gut motality and constipation Increases alkaline phosphate |
|
|
|
Hormonal changes in pregnancy |
Progesterone promotes uterine quiescence (inactivity) and thicken cervical mucus Relaxin soften ligaments and acts like a vasodilator Oestrogen causes cervical development, thickening of Vaginal epithelium and increased Vaginal discharge |
|
|
|
What does labour begin with? |
The onset if regular painful uterine contractions with cervical change |
|
|
|
What is parturition? |
Action of giving birth |
|
|
|
Role of Parathyroid hormone on Renal function? In which parts of the kidneys? |
It blocks reabsorption of phosphate in the PCT and promoted Ca2+ reabsorption in ascending loop of henle, distal tubule, collecting tubule |
|
|
|
What is the difference between male and female pelvis? |
Females have a much wider pelvic I let to allow the passage for the baby during birth |
|
|
|
What cells release Inhibin in males? |
Sertoli |
|
|
|
Which hormone stimulate prostaglandin release during a period? Why? |
During the period, oestrogen stimulates prostaglandin release causing uterine arteiroles to constrict so cells don't recieve oxygen and die |
|
|
|
Calcium reabsorption in kidneys |
More than 95% of filtered calcium is reabsorbed along the renal tubules. In the proximal tubules, 60% of filtered calcium is reabsorbed by passive mechanisms. In the thick ascending limb, 15% of calcium is reab |
|
|
|
UG histology: |
Endocervix: simple columnar
Ureters and bladder: transitional
Vas deferens: ciliated pseudostratified columnar epithelial
Descending & thin ascending: simple squamous
DCT: cuboidal
Collecting duct : columnar cells
PCT: simple cuboidal epithelium with brush border (Microvilli) |
Simple cuboidal |
|
|
What channels does glucose enter blood vessels into, coming out of PCT? |
Glut 2 |
|

