![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
375 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
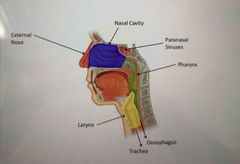
Gross anatomy of the nose and surrounding regions |
|
|
|
|
What are the functions of the nose? |
-adjusts temperature and humidity of inhaled air -traps and removes particles -olfaction (smell) |
|
|
|
What is the external nose made up of? Lateral profile |
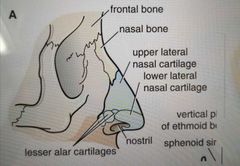
|
|
|
|
What is the front profile of the external nose? |
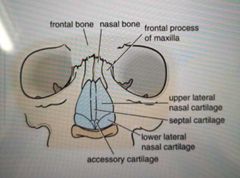
|
|
|
|
What is the internal, lateral profile of the nose? |
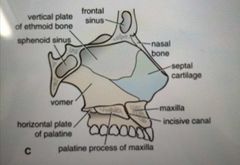
|
|
|
|
Describe the anatomical position of the nasal cavity |
-Extends from anterior apertures (nostrils) to posterior apertures (chonae) |
|
|
|
What is the choanae? |
Spot it at the beginning of the throat |
|
|
|
What is the nasal cavity seperated from the oral cavity by? |
The hard palate - horizontal plate of palatine/ palatine process of maxilla |

|
|
|
What is the nasal cavity divided in the midline by? |
The septum |
|
|
|
What bones separate the nasal cavity from the cranial cavity? |
Frontal Ethmoid Sphenoid bones |
|
|
|
The nasal cavity is divided into 3 distinct functional regions. Name them |
Nasal vestibule Respiratory Olfactory |
|
|
|
Nasal vestibule |
The green part on the pic -internal to nostrils -lined by skin and covered in short hair follicles |

|
|
|
Respiratory region |
Blue in the pic below -largest part of nasal cavity -rich neurovascular blood supply |

|
|
|
What are the bony structures present in the nasal cavity? |
|
|
|
|
Olfactory region of the nasal cavity |
Pink in the pic below -small region at the apex of the nasal cavity |

|
|
|
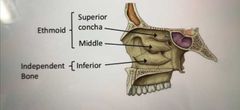
Nasal cavity - lateral walls |
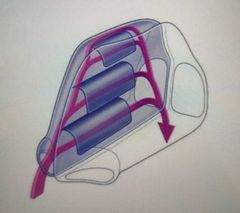
-characterised by 3 curved shelves of bone called the chonchae: projected off the lateral wall |
|
|
|
What is the function of the chonchae? |
Divide the cavity into four air channels in order to increase contact surface area with inspired air |
|
|
|
What is the space below each chonchae called? |
Meatus |
|
|
|
Name of meatuses |
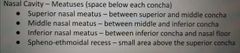
|
|
|
|
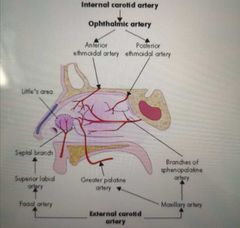
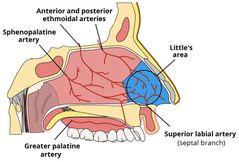
Briefly describe the blood supply to the nose |
The superior part is supplied by the : internal carotid artery - then opthalmic artery
The Inferior part is supplied by the external carotid artery |
|
|
|
What are the 2 branches of the opthalmic artery? |
Anterior and posterior Ethmoidal artery |
|
|
|
Where are the lateral nasal branches derived from? (Check this) |
Facial artery |
|
|
|
What does the sphenopalatine artery branch into? |
Septal branches (no I don't think they do) |
|
|
|
What is kisselbach's/ little's area? |
Area where arteries link on the septum. It's a come site of epistaxis (nose bleed) |
|
|
|
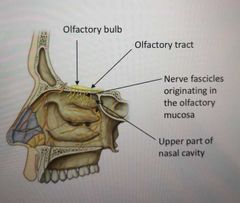
Describe the innervation to the nose |
Olfaction - sense of smell supplied by the olfactory nerve (CN1) Only occurs in the olfactory region of the nasal cavity |
|
|
|
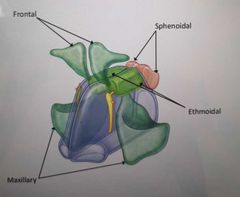
What is a sinus? |
Sack / cavity |
|
|
|
How many paranasal sinuses are there? What are the names? |
4 (each named after the bone they are found in)
Frontal Maxillary Ethmoidal Sphenoidal |
|
|
|
What are the paranasal sinuses lined with? |
Respiratory mucosa (ciliated and mucus secretion) |
|
|
|
What are the functions of the paranasal sinuses? |
Lighten the skull Resonace (quality of sound) Absorb shock |
|
|
|
What do the paranasal sinuses connect to? |
Open into nasal cavities to allow drainage of mucus |
|
|
|
Paranasal sinuses drainage |
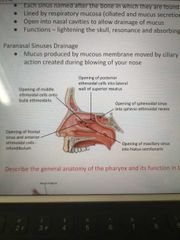
Learn this more: |
|
|
|
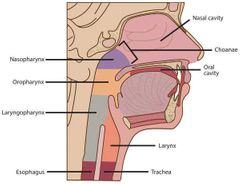
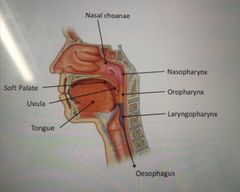
Label the gross anatomy of the pharynx |
|
|
|
|
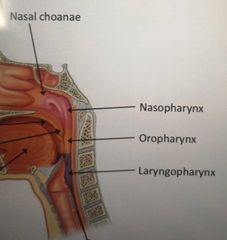
What are the 3 parts of the pharynx? |
Nasopharynx Oropharynx Laryngopharynx |
|
|
|
What are the muscles of the pharynx? |
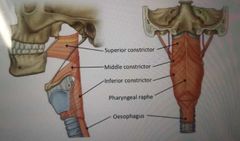
Oesopwis also a muscle of the pharynx (?) |
|
|
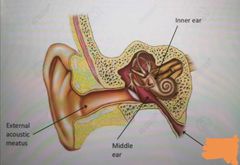
What is the covered up orange thing? |
Eustachian tube/ pharyngotympanic |
|
|
|
What is the eustachian tube? |
A tube that links the nasopharynx to the middle ear The middle ear is not in direct contact with the atmosphere |
|
|
|
How does the structure of the eustachian tube change shape during swallowing? What pressure? |
Normally the tube is collapsed but opens during swallowing and with positive pressure |
|
|
|
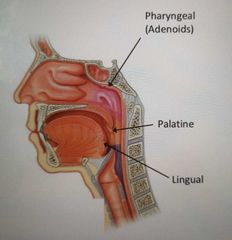
What are tonsils? |
Collections of lymphoid tissue in mucose of pharynx Surrounds openings of the nasal and oral cavities |
|
|
|
What are the 3 sets of tonsils? |
Pharyngeal Palatine Lingual |
|
|
|
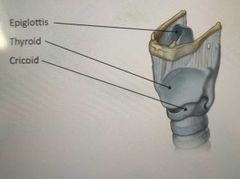
What is the function of the larynx? |
-conducts air from pharynx to trachea -keeps food and liquid out of the lower respiratory tract -facilitates the production of speech |
|
|
|
What are the 3 unpaired cartilages present in the larynx |
Epigolottis Thyroid Cricoid |
|
|
|
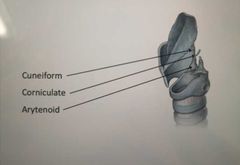
What are the 3 paired cartilages of the larynx? (+order from top to bottom) |
Cuneiform Corniculate Arytenoid |
|
|
|
What bone is the larynx suspended from? |
Hyoid bone - makes the larynx highly mobile |
|
|
|
Vasculature of the larynx (learn the diagram) |
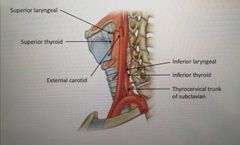
Superior part of larynx: External carotid Superior thyroid artery Superior laryngeal Inferior part of larynx: Thyrocervical trunk of subclavian Inferior thyroid artery Inferior laryngeal |
|
|
|
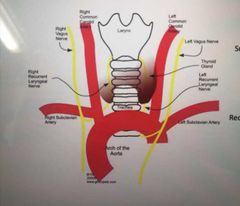
Branches of which cranial nerve innervates the larynx? |
Branches of the vagus nerve (CN 10) |
|
|
|
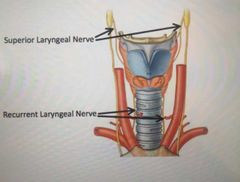
What is the name of the sensory nerve above the vocal cord? |
Superior laryngeal |
|
|
|
What is the sensory nerve below the vocal cords? What does it loop under? |
The recurrent laryngeal
-The left nerve loops under aortic arch then upwards -right nerve loops under right subclavian artery then upwards |
|
|
|
What is the motor supply to all muscles except the cricothyroid? |
Recurrent laryngeal |
|
|
|
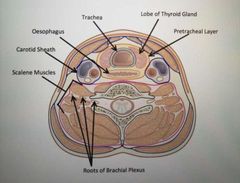
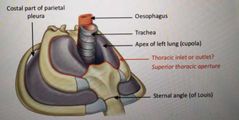
Describe the position of the trachea in the neck |
-Commences at the lower border of the larynx -Anterior to oesophagus |
|
|
|
Which compartment does the trachea lie in? |
Lies within the visceral compartment of the neck, surrounded by a pre-tracheal layer of fascia |
|
|
|
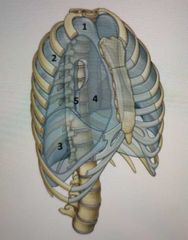
What is the position of the trachea in the Thoracic cavity? |
-Trachea enters the superior thoracic cavity (which connects the root of the neck with the thorax) |
|
|
|
Where are the superior aspects of the pleural cavities found? |
Surrounding lungs, on either side of the entrance to the mediastinum |
|
|
|
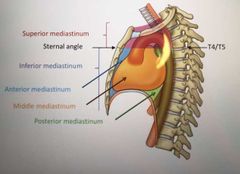
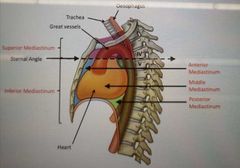
How many parts is the mediastinum split into? |
2
Superior Inferior |
|
|
|
Where is the sternal angle found? |
T4/T5 |
|
|
|
What is the sternal angle also known as? |
Angle of Louis |
|
|
|
What point does the trachea bifurcate? What is this point called? |
T5 - Carina |
|
|
|
How many parts is the Inferior mediastinum split into? |
3 Anterior Middle Posterior |
|
|
|
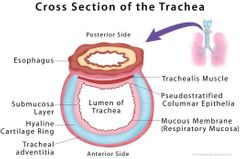
What is the trachea made of? |
It's a mobile cartilagionous and membranous tube |

|
|
|
What are the dimensions of the trachea? |
11 cm long 2.5 cm diameter |
|
|
|
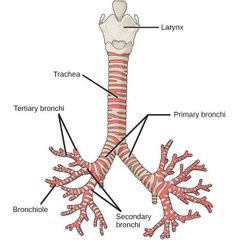
What does the trachea split into? |
Left and right bronchi at the sternal angle |
|
|
|
What is the fibroelastic tube kept up by? |
U-shaped bars (rings) of hyaline cartilage |
|
|
|
What are the posterior free ends of the U-shaped rings of hyaline cartilage connected by? |
Smooth muscle: trachealis |
|
|
|
What are the 4 layers of the trachea? |
Mucose Submucosa Fibrocartilage (hyaline?) Adventita |
|
|
|
What is the mucosa layer formed of? |
By psedostratified ciliated columnar epithelium with many goblet cells who secrete mucin |
|
|
|
What does adventita do? |
Binds trachea to adjacent structures in the neck and mediastinum |
|
|
|
What protects the alveoli from desiccation? (drying out) |
Secretions of mucous and serous glands which moisten the air |
|
|
|
What is the Submucosa? |
Connective tissue with seromucous glands |
|
|
|
Histology of the cross section of the trachea |
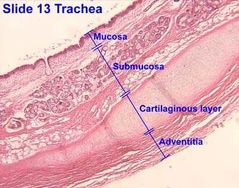
|
|
|
|
Describe the splitting of the bronchi |
Main bronchus (primary) Lobar bronchus (secondary) Segmental bronchus (tertiary) Terminal bronchus Bronchioles |
|
|
|
Which bronchus is wider and shorter? |
Right main bronchus |
|
|
|
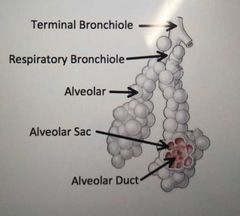
What does each respiratory bronchiole divide into? |
2-11 alveolar ducts that enter alveolar sacs |
|
|
|
Order of bronchioles |
Terminal bronchiole Respiratory bronchiole Alveolar ducts Alveolar sacs Alveoli |
|
|
|
What is each lung protected by? |
The pleural membrane |
|
|
|
From where to where do the lungs span? |
From the diaphragm to slightly superiorly to the clavicle and lie against the ribs anteriorly and posteriorly |
|
|
|
What is the base of the lungs? |
Broad inferior portion of lung that is concave and fits over convex diaphragm |
|
|
|
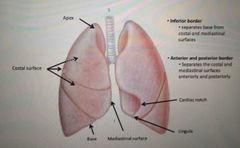
What is the name of the surface that is in contact with the ribs? |
Costal surface |
|
|
|
What is the name of the surface that is not in contact with the ribs? |
Mediastinal surface |
|
|
|
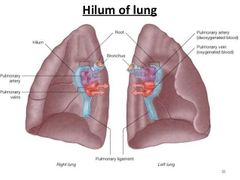
Which surface contains the hilum? |
Mediastinal surface |
|
|
|
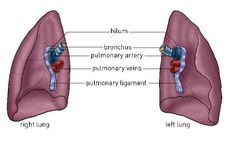
What is the hilum of the lungs the point of entry for? |
The lung root, consisting of:
Bronchi Pulmonary arteries (on top) Pulmonary veins |
|
|
|
Where are the vagus and phrenic nerves found in relation to the lung |
Vagus nerve runs posterior to lung root and phrenic nerve runs anterior to lung root |
|
|
|
What is the name of the space where the heart is found? |
Cardiac notch |
|
|
|
What is the Inferior border? |
Seperates base from costal and mediastinal surfaces |
|
|
|
What is the anterior and posterior border? |
Seperates the costal and mediastinal surfaces anteriorly and posteriorly |
|
|
|
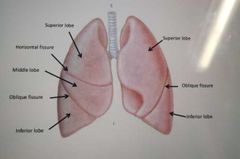
What divides the lungs into lobes? |
Fissures |
|
|
|
Which fissure is present on both lungs? |
Oblique fissure (extends inferiorly and anteriorlyl |
|
|
|
What fissure is present only on the right lung? |
Horizontal |
|
|
|
What are the lobes on the left and right lungs? What are the names? |
Right: Superior Middle Inferior Left: Superior Inferior |
|
|
|
What is the functional unit of the lung? |
Each Lobar bronchus gives rise to Segmental bronchi which supply a bronchipulmonary segment (10 in each lung) containing lobules |
|
|
|
What is each lobule wrapped in? |
Elastic connective tissues |
|
|
|
What does each lobe contain? |
Lymphatic vessel Arteriole Veunule Branch of the terminal bronchus |
|
|
|
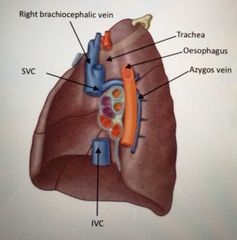
What are the specific features of the right lung? |
Presence of azygos vein (which bypasses IVC), SVC and IVC on right side |
|
|
|
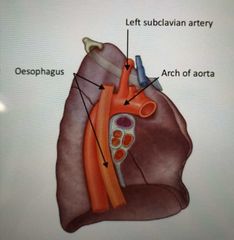
Specifics of the left lung? |
Presence of the arch of aorta depression, left subclavian artery depression |
|
|
|
What is the Pulmonary ligament made of? |
Fold of pleura |
|
|
|
Pulmonary ligament position |
Projects inferiorly from root of lung |
|
|
|
Function of the Pulmonary ligament |
Stabalises Inferior lung and permits movements during respiration |
|
|
|
What are the general rules of the Hila (Hilum) of the lungs? |
Pulmonary arteries are superior Pulmonary veins are Inferior Bronchi are posterior However in the RIGHT hilum: bronchi branch is before the root In the left: bronchi branch is withun the lung itself |
|
|
|
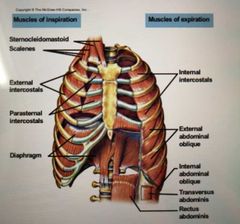
Muscles of Inhalation |
Sternocleidomastoid Scalenes External intercostal Diaphragm |
|
|
|
Muscles of exhalation |
Internal/ innermost intercostals External oblique Internal oblique Transversus abdominis Rectus abdominis |
|
|
|
Diaphragm action |
Contracts to increase lung volume |

|
|
|
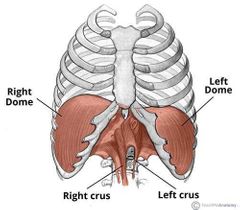
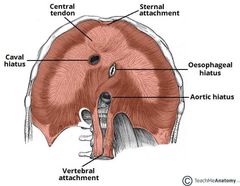
What is the diaphragm attached to? |
It is attached anteriorly to the xiphoid process of the sternum
Costal cartilages of ribs (7-10)
Laterally to the 11th and 12th ribs
Posteriorly to the lumbar vertebrae |
|
|
|
What is a Crura/ crus? Where is it attached to the lungs at? |
The crus of diaphragm (pl. crura), refers to one of two tendinous structures that extends below the diaphragm to the vertebral column. There is a right crus and a left crus, which together form a tether for muscular contraction
Right - L1-L3 Left - L1-L2 |
|
|
|
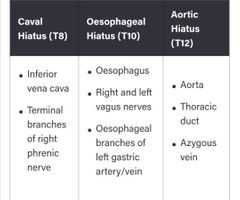
There are three openings of the diaphragm. What vertebrae does the inferior vena cava pass through the diaphragm? What is their opening called? |
Caval haitus T8
(vena cava has 8 letters) |
|
|
|
What general part of the diaphragm does the vena cava pass through? |
Central Tendon |
|
|
|
Which vertebrae does the oesophagus and vagus nerve pass through? |
T10 (oesophagus has 10 letters) |
|
|
|
What part of the diaphragm do the oesophagus and vagus nerve pass through? |
The diaphragm muscle |
|
|
|
Where is the aortic hiatus found? |
T12 through the diaphragm muscle
(aortic hiatus has 12 letters) |
|
|
|
What is the diaphragm innervated by? |
By the left and right phrenic nerves |
|
|
|
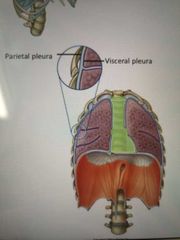
What type of nerve supply feeds the parietal vs visceral pleura? What do the nerves respond to? |
Parietal- Somatic nerve supply. Responds to touch/ temperature/ pressure Visceral- autonomic nerve supply. Responds to distention (stretch) |
|
|
|
Parietal pleura innervation? Different surfaces innervction |
Costal and peripheral pleural is innervated by intercostal nerves
Mediastinum and central diaphragmatic are innervated by phrenic nerve (C3-5) |
|
|
|
Visceral pleura innervation |
Pulmonary plexus Vagus nerve |
|
|
|
What type of membrane is the pleura? |
A serous membrane (a smooth membrane which secretes serous fluid) |
|
|
|
What is the pleura? |
Two membranes of epithelial cells which line and enclose body cavities. One continuous layer lines each cavity. |
|
|
|
What does the parietal and visceral parts of the pleura line? |
Parietal (lines body walls) Visceral (lines organs) |
|
|
|
Development of the pleural cavities: |
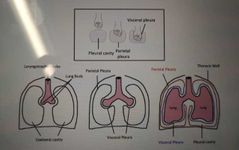
|
|
|
|
What are the parietal pleura regions? |
1) Cervical 2) Costal 3) Diaphragmatic 4) Mediastinal 5) Pulmonary ligament |
|
|
|
What is the extent of the visceral pleura? How far does it go? |
-Extends into the interglobar fissure -Parietal and visceral pleura are continuous around the hilum of the lung |
|
|
|
What is the space between the parietal and visceral layer called? |
Pleural cavity |
|
|
|
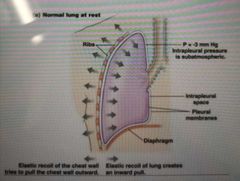
What is the normal pressure state in the pleura? |
Intra-pleural pressure is less than atmospheric pressure. Thus is said to be 'negative pressure' |
|
|
|
What keeps the lungs inflated? |
The elastic recoil of the chest wall which tries to pull the chest outwards
And
The elastic recoil of lungs which creates an inwards pull
Pulling the chest wall and lungs away from each other |
|
|
|
What is the pressure inside the Intra-pleural space? |
-3 mm Hg Said to be subatmosphereic |
|
|
|
What happens if Intra-pleural pressure becomes equal to or exceed atmospheric pressure? |
Lungs will collapse causing pleural effusion/ pneumothorax |
|
|
|
What is pleural effusion? |
-Excess fluid in the pleural cavity -Limits breathing as it hinders lung expansion -Main causes are infection or inflammation of pleura or left ventricular heart failure |
|
|
|
Muscles of inspiration. For normal/ quite breathing in. |
External intercostals Parasternal intercostals Diaphragm |
|
|
|
Muscles of inspiration for forced breathing in |
Scalenes Sternocleidomastoid |
|
|
|
Muscles of forced expiration? |
Internal intercostals Rectus abdominis (strongest) Transversus abdominis Internal oblique External oblique |
|
|
|
Mechanism of inspiration? Vertical and horizontal increase in volume |
Volume of Thoracic cavity increases vertically when the diaphragm contracts Volume increases laterally when the Parasternal intercostals raise the ribs Intra-pulmonary pressure decreases, hence air moves into the lungs |
|
|
|
Mechanism of expiration. Vertical and horizontal volume |
Volume of Thoracic cavity decreases vertically when the diaphragm relaxes Laterally when the external and Parasternal intercostals relax for quite expiration |
|
|
|
In forced expiration what muscles relax? |
Internal intercostals Abdominal Oblique muscles Lower the ribs in forced expiration |
|
|
|
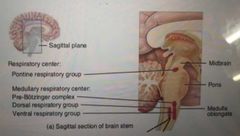
What in the brain is responsible for the nervous control of breathing? |
The medullary respiratory centre |
|
|
|
What does the medullary respiratory centre consist of? |
The dorsal respiratory group (DRG) Ventral respiratory group (VRG) |
|
|
|
What is the nervous control during normal quite breathing? |
Dorsal respiratory group generate impulses to the diaphragm via the phrenic nerve (C3/4/5) And To the external intercostals via intercostal nerves |
|
|
|
The ventral respiratory group is split into 3 regions. What are they? |
Rostral Intermediate Caudal |
|
|
|
What complex is responsible for the generation of respiratory rhythm? |
The pre-botzinger complex - it provides input into the DRG |
|
|
|
Where is the pre-botzinger complex found? |
In the rostral VRG |
|
|
|
What initiates the contraction of muscles involved in forced inspiration? |
The intermediate VRG |
|
|
|
What initiates the contractions of muscles involved in forced expiration? |
Caudal VRG |
|
|
|
Diagram for medullary respiratory Centre? |

|
|
|
|
What does the pontine respiratory Centre consist of? |
Apneustic Centre Pneumotaxic Centre |
|
|
|
Apneustic Centre. Function and location? |
Lower pons Limits lung expansion |
|
|
|
What is apneuses? |
Gasping inspiratory breaths |
|
|
|
Pneumotaxic Centre |
Upper pons Shortens inspiration/ increases ventilation rate |
|
|
|
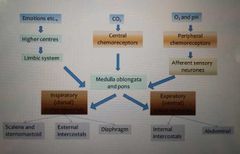
What are the receptors involved in ventilation control? |
Central chemoreceptors Peripheral chemorreceptors Stretch receptors |
|
|
|
Where are the central chemoreceptors found? |
Ventral surface of medulla |
|
|
|
What do the Central chemoreceptors respond to? How do they overcome this? |
Increased pCO2 Respond by increasing ventilation and depth |
|
|
|
Where are peripheral chemoreceptors found? |
At carotid bodies At the aortic arch |
|
|
|
Which nerve does the carotid bodies send signals down? |
Glossopharygeal nerve to the respiratory Centre in the brain |
|
|
|
What does the aortic arch send signals down? |
Vagus nerve to the respiratory Centre |
|
|
|
What do peripheral chemoreceptors detect? |
Decreased pO2 Increased H+ Respond by increasing rate and depth of breathing |
|
|
|
Why are there central and peripheral chemoreceptors? |
They're present in different environments, because they have different sensitivities |
|
|
|
Where are stretch receptors found? |
In the bronchi |
|
|
|
What role do the stretch receptors play in the ventilation control? |
Stretch receptors become overstretched due to breathing too deeply - impulses are sent to DRG via the vagus nerve |
|
|
|
Diagram to describe ventilation |
|
|
|
|
What are the other influences on breathing? |
Limbic system stimulation Temperature |
|
|
|
Lymbic system stimulation |
Anticipation of activity may stimulate the limbic system which sends excitatory impulses to DRG increasing rate |
|
|
|
How does temperature effect breathing rate? |
Increase in body temperature increases breathing rate |
|
|
|
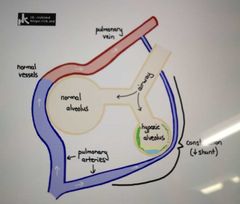
What is hypoxic vasoconstriction? |
This is when an alveoli or bronchiole is damaged and so is under ventilated. Blood passing by this has very low pO2 so it converges with another artery for oxygenation at a different alveoli
Blood flow is diverted to other healthy alveoli |
|
|
|
Inspiration in terms of pressures |
Intra-pulmonary pressure < atmospheric pressure and air moves into the lungs |
|
|
|
Expiration in terms of pressure |
Intra-pulmonary pressure > atmospheric pressure and air moves out of the lungs |
|
|
|
What is transpulmonary pressure? |
Difference between Intra-pulmonary (within the the lung) and Intra-pleural (between the layers) pressure keeping lungs against Thoracic wall and allows lungs to expand as Thoracic wall expands. |
|
|
|
Is Intra-pleural pressure neg or pos |
Intra-pleural pressure is negative. Part of the mechanism that maintains the structure of the lungs and allows them to expand in inspiration |
|
|
|
What's is hassle backs equation? |
CO2 + H2O - - > H2CO3 - >HCO3- +H+ |
|
|
|
What catalyses CO2 + H2O - > H2CO3 |
Carbonic anhydrase |
|
|
|
Where are central chemoreceptors found? What do they detect? |
Brain Detects carbon dioxide levels in CSF |
|
|
|
What does CSF do? |
Provide nutrients to the central nervous system |
|
|
|
What do peripheral chemoreceptors detect? |
Oxygen Carbon dioxide PH |
|
|
|
What does the medulla contain? |
The dorsal and ventral respiratory groups |
|
|
|
What is Boyle's law? |
Pressure of a gas is inversely proportional to its volume (a container with air in it, then when it is squished so volume is lower, the pressure has become greater) |
P1V1 = P2V2 |
|
|
Boyle's laws in terms of inspiration and expiration? |
Inspiration: an increase in lung volume during inspiration decreases Intra-pulmonary pressure to sub atmospheric levels so air goes in Expiration: a decrease in lung volume during expiration increases Intra-pulmonary pressure above atmospheric levels so air goes in |
|
|
|
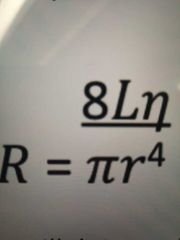
Poiseuille's law |
Calculates resistance to airflow, essentially saying that resistance is higher when radius of airway is smaller |
|
|
|
What is pulmonary/ lung compliance? |
A measure of the lungs ability to stretch and expand
|
|
|
|
Changes in elasticity during breathing |
Elastic tension increases during inspiration and is reduced by elastic recoil during expiration. |
|
|
|
Why are the lungs always under elastic tension? |
Because the lungs are stuck to the thoracic wall |
|
|
|
Surface tension in the lungs? |
Surface tension is exerted by pulmonary surfactant fluid secreted on the alveoli to resist distension |
|
|
|
What is the law of laplace |
Pressure is directly proportional to surface tension and inversely proportional to radius of alveoli |
|
|
|
What is surfactant? |
Fluid like substance which reduces surface tension between water molecules by reducing the number of hydrogen bonds between the water molecules |
|
|
|
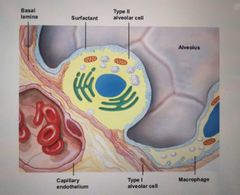
What secretes surfactant? |
Type II Alveolar cells |
|
|
|
What is surfactant made up of? |
Hydrophobic protein and phospholipids |
|
|
|
When is surfactant most concentrated? |
As alveoli get smaller during expiration. This prevents collapse of alveoli hence allows a residual volume of air to remain in lungs |
|
|
|
Explain the A-a gradient |
A = Alveolar a = arterial Its a measure of the difference in the Alveolar concentration of oxygen and the arterial concentration of oxygen |
|
|
|
Why is the A-a gradient clinically useful? |
A useful indicator of the cause of hypoxia (low oxygen concentration in the blood) |
|
|
|
How is the A-a gradient measured? |
pAO2 - paO2 Alveolar - arterial pO2 |
|
|
|
What is the A-a gradient usually? |
5-10 mmHg |
|
|
|
How can you measure paO2? |
By taking arterial blood gas |
|
|
|
What is piO2? |
Partial pressure of O2 in the inspired air delivered to the patient |
|
|
|
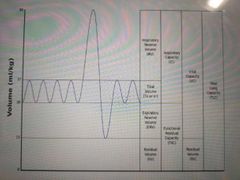
What is tidal volume? |
Amount of air in a single inspiration or expiration (~500ml) |
|
|
|
What is Functional Residual Capacity |
Volume of air that remains in lungs at the end of normal expiration (2400) |
|
|
|
What is vital capacity? |
Volume of air that can be exhaled after a maximal inspiration (4800) |
|
|
|
What is residual volume? |
Amount of air remaining in lungs after maximal expiration (1200ml) |
|
|
|
What is total lung capacity? |
Maximum volume of air in the lungs after a maximal inspiration (6000ml) |
|
|
|
SPIROMETER TO LEARN OFF BY HEART |
|
|
|
|
How is spirometry performed? |
Take deepest breath in possible, exhale into sensor as hard and fast as possible, for as long as possible (preferably at least 6 seconds). Followed by a rapid inhalation (inspiration) |
|
|
|
What is Forced Expiratory Volume (FEV1) |
Volume of air than can be forcibly be blown out in one second after full inspiration measured in litres |
|
|
|
What is Forced Vital Capacity (FVC) |
Volume of air that can forcibly be blown out after full inspiration measured in litres |
|
|
|
Criteria for normal spirometery |
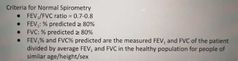
|
|
|
|
What is obstructive disease? |
When the FEV1/ FVC ratio: <0.7 (regardless of FEV1 % and FVC % predicted) |
|
|
|
What are diseases associated with with obstructive disease? |
Emphysema Chronic bronchitis Uncontrolled asthma Bronchiectasis (permenant enlargement of parts of airways) Cyctic fibrosis |
|
|
|
What does the volume x time trace for obstructive disease look like? |
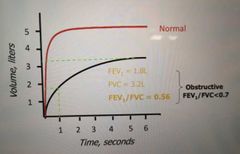
|
|
|
|
Flow vs volume graph for instructive diseases |

|
|
|
|
What is restrictive disease? |
FEV1/ FVC ratio >0.8 FEV1 % PREDICTED : reduced (<80%) FVC PREDICTED: reduced (<80%) |
|
|
|
What are some associated diseases to restrictive disease? |
Lung fibrosis Pneumoconiosis (coal miners lungl Pulmonary oedema (heart failure) Thoracic cage deformity Obeasity Pregnancy |
|
|
|
What does the volume x time trace for restrictive disease look like? |
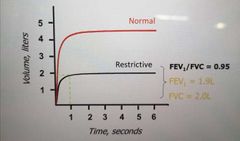
|
|
|
|
What is the flow x volume trace for restrictive disease? |
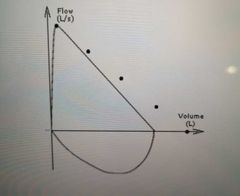
|
|
|
|
How can respiratory muscle strength be tested? |
Through assessing Maximal inspiratory pressure (MIP) Or Maximal expiratory pressure (MEP) |
|
|
|
What does maximal inspiratory pressure tell? |
Reflects the strength of the inspiratory muscles |
|
|
|
What is maximal expiratory pressure? |
Reflects the strength of the expiratory muscles |
|
|
|
What is used to measure MIP and MEP? |
A mechanical pressure gauge |
|
|
|
What is Diffusion Capacity in pulmonary ventilation? |
Measure of the the ability of the lungs to extract O2 from inhaled air and into pulmonary capillaries |
|
|
|
How is diffusion capacity determined? |
By surface area Length of diffusion pathway Haemaglobin levels |
|
|
|
How is diffusion capacity measured? |
By testing how much CO is up taken by the lungs in a given time |
|
|
|
What affects diffusion capacity? |
Since its determined by surface area, in conditions where SA is reduced (Pulmonary fibrosis, emphysema) diffusion capacity is also reduced |
|
|
|
What is VO2? |
Maximum amount of O2 that someone can utilise during peak exercise (L/min) |
|
|
|
What is VO2 limited by? |
By how fast the cardiovascular system can deliver oxygen to the exercising skeletal muscles Also by how fast exercising muscles can extract oxygen from the blood |
|
|
|
How to detect when VO2 has maxed? |
When O2 uptake remains constant despite workload increasing |
|
|
|
What is Pulmonary ventilation? (PV) |
The volume of air that moves in (or out) of lungs per minute
PV =volume of air per breath x number of breaths per minute |
|
|
|
What is Alveolar ventilation (equation) |
(Tidal volume - dead space) x breaths per min |
|
|
|
What is anatomical dead space? |
Space occupied by the conducting Airways - Trachea, bronchi and bronchioles (approx 150 ml) |
|
|
|
What is physiological dead space? |
Decreased number of alveoli participating in gaseous exchange
Dead space is the volume of air that is inhaled that does not take part in the gas exchange, because it either remains in the conducting airways or reaches alveoli that are not perfused or poorly perfused. In other words, not all the air in each breath is available for the exchange of oxygen and carbon dioxide. Mammals breathe in and out of their lungs, wasting that part of the inhalation which remains in the conducting airways where no gas exchange can occur. |
|
|
|
What are the cells of the alveoli? |
Type 1 Alveolar cells Type 2 Alveolar cells |
|
|
|
What are Type 1 Alveolar cells? |
Squamous Pulmonary epithelial cells Most common type and almost entirely line the Alveolar wall |
|
|
|
What are Type 2 Alveolar cells? |
Septal cells They secrete Alveolar fluid |
|
|
|
What is one thing that Alveolar fluid contains? |
Surfactant |
|
|
|
What do Type 1 cells do? |
Gas exchange |
|
|
|
Histology of the alveoli? |
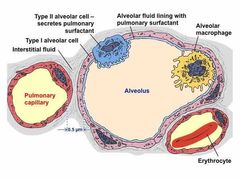
|
|
|
|
What is the role of surfactant in the alveoli? |
Surfactant coats luminal surface of alveoli |
|
|
|
What force does surfactant exert? |
Surface tension |
|
|
|
What does surface tension do to the alveoli? |
Causes it to assume the smallest possible diameter. During breathing, surface tension must be overcome to expand the lungs during each inhalation |
|
|
|
What is Dalton's law? |
The total pressure is equal to the sum of the partial pressure |
|
|
|
How does altitude affect partial pressure? |
With higher altitude, there's a falling partial pressure of oxygen. This reduces the partial pressure gradient driving O2 uptake and causes hypoxia |
|
|
|
What is the impact of hypoxia? |
Causes sensory and cognitive functions to decline |
|
|
|
What is hypoxia sensed by? What response to the stimuli |
Peripheral chemoreceptors and the respiratory Centre responds |
|
|
|
What is the response driven from the respiratory centre when hypoxia is sensed |
Responds by increasing ventilatory drive which increases oxygen uptake and carbon dioxide emission |
|
|
|
What does acute mean? |
Sudden Probably short term Urgent |
|
|
|
What are the acute responses of high altitude? |
-Hypoxia -Suppression of the cardioinhibitory centre |
|
|
|
What is the cardioinhibitory centre suppressed by? |
The respiratory centre |
|
|
|
What is the response of the respiratory centre suppressing the cardioinhibitory centre? |
Increase in heart rate/ Cardiac output and hence increasing oxygen uptake by Pulmonary perfusion |
|
|
|
What is perfusion? |
Refers to the flow of blood to Alveolar capillaries |
|
|
|
What are the adaptive responses of the body at high altitude? (days to weeks) |
-Central chemoreceptors adapt slowly over a period of 8-24 hours -decreases pCO2 (an acid) causing respiratory alkalosis |
|
|
|
How does the adaption in the central chemoreceptors help the effect of high altitude? |
Allows ventilation rates to climb to address altitude-induced hypoxia |
|
|
|
What is the body's response to respiratory alkalosis? |
Kidneys compensate by decreasing acid secretion in the urine. So more acid stays in the blood. Renormalizing pH. |
|
|
|
What does alkalosis also stimulate? |
2,3-DPG production |
|
|
|
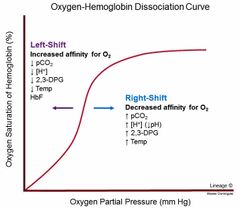
What is the influence of 2,3-DPG? |
Decreases Hb's O2 affinity causing O2 Hb dissociation curve to shift to the right and this enhances O2 unloading to the tissues |
|
|
|
Altitude aclimation (months-years). What does hypoxia stimulate? |
Hypoxia stimulates the release of erythropoieton from the kidneys which increases Hb concentration - increasing blood O2 capacity Hypoxia also stimulates angioneogenesis |
|
|
|
What is angioneogenisis? |
Increases capillary density + tissue perfusion Angiogenesis is the physiological process through which new blood vessels form from pre-existing vessels, formed in the earlier stage of vasculogenesis. Angiogenesis continues the growth of the vasculature by processes of sprouting and splitting. |
|
|
|
What are the acute adverse effects to hypoxia? |
Headache Irritability Insomnia Dyspnoea Dizziness Nausea |
|
|
|
Chronic adverse effects to Hypoxia? |
Bronchoconstriction stresses right side of the heart - causing heart failure and Pulmonary oedema |
|
|
|
What are the categories of physiological changes that take place in diving? |
Effects of depth Gas toxicity Nitrogen narcosis Oxygen poisoning Decompression sickness |
|
|
|
Explain the effects of depth when diving, in terms of pressure |
When underwater, there is external hydrostatic pressure which increases with depth |
|
|
|
What does the increased external hydrostatic pressure do? |
Compresses gas within the alveoli, which increases partial pressure of all gases and decreases the Alveolar volume |
|
|
|
What can the impact of increased partial pressure and decreased Alveolar volume be? |
-Since depth increases partial pressures of all gasses, all gases dissolve into blood. Where as at sea level only O2/ CO2 can dissolve. This can be lethal -pressuring a gas decreases it's volume, so when a diver resurfaces this can cause severe damage to the tissues that contain the gas |
|
|
|
Gas toxicity underwater |
Air is principally made up of N2 and O2, both of which are toxic when inhaled under pressure |
|
|
|
What do divers who work at depth breath in instead? To avoid gas toxicity? |
A helium/ oxygen mix. Helium replaces N2 because it dissolves in the body tissues less readily |
|
|
|
What is nitrogen narcosis? |
At depths of 40m or more, the pressure of N2 rises to the point where it dissolves in cell membranes in amounts sufficient to disrupt ion channel function. Has effects similar to those of ethanol - is a narcotic |
|
|
|
What is oxygen poisoning? |
Breathing in O2 at high pressures cause it to dissolve in blood in amounts that exceed the buffering capacity of Hb. This causes a variety of neurological effects. |
|
|
|
What kind of neurological effects can oxygen poisoning cause? |
Visual disturbances Seizures Coma |
|
|
|
Why is O2 toxic? |
Naturally yes, because it has a tendency to form free radicals |
|
|
|
What causes decompression sickness (The Bends)? |
-A diver breathing air at pressure can accumulate significant amounts of N2 within their tissues. So when the diver ascends to surface, pure N2 bubbles are formed. -these bubbles block blood vessels as smaller bubbles join together causing dependent tissues to become ischaemic |
|
|
|
What is ischaemia? |
Restriction of blood supply to tissues, causing a shortage of oxygen.
Leads to pain in joints and limb muscles |
|
|
|
What are more severe symptoms of decompression sickness? |
Neurological deficits Dyspnoea (laboured breathing) Death |
|
|
|
How to treat a patient with decompression sickness? |
Must be given hyperbaric treatment in a decompression chamber. Pumping O2 back into their blood and relieving their symptoms |
|
|
|
How does the metabolic rate effect respiration? |
Increasing metabolic rate = Increasing rate of aerobic respiration.
So increased amounts of O2 taken in and CO2 removed causes metabolic rate to increase as well as the rate and depth of breathing.
Oxygen debt causes anaerobic respiration to be utilised and hence there's a build up of Lactic acid |
|
|
|
How does the foetus get oxygen? |
From the placenta. Carbon dioxide is also removed via the placenta |
|
|
|
When are attempts at respiratory movements made during development? What are they caused by? |
By the end of the 1st trimester
Caused by tactile and foetal asphyxia |
|
|
|
In which months of pregnancy, are breathing movements inhibited and the lungs almost completely deflated? |
3rd and 4th month |
|
|
|
What does this help prevent during the 3rd and 4th month of pregnancy? |
Meconium aspiration |
|
|
|
Why is small amounts of fluid secreted into the lungs until birth? By what? |
To keep clean fluid in the lungs Secreted by the alveolar epithelium |
|
|
|
Initiation of breathing in the neonate |
-compression of fluid from foetal lung during Vaginal delivery establishes lung volume -cutting off placenta removes oxygen supply causing asphyxia (suffocation) - which increases CO2 and decreases O2 - causing acidosis hence stimulates respiratory centres in the medulla/ chemoreceptors in the carotid arteries to initiate breathing |
|
|
|
What role does temperature play in the stimulation of breathing? |
Decrease in temperature, cause the stimulation of nerve endings in the skin in the new extrauterine environment to stimulate breathing |
|
|
|
Describe lung development in infants |
-Elastic fibre development occurs postnatally -development of alveoli from saccules occurs postnatally too |
|
|
|
Respiratory system in old age |
-Decreased elastic recoil of lung tissues and chest wall complaince -decreased strength in the respiratory muscles -increased residual volume, decreased vital capacity and decreased FEV1 |
|
|
|
Respiratory system and obesity |
-Upper Airways restriction and lung volume reduction -increases risk of atelectasis |
|
|
|
What is atelectasis? |
Collapsed lung |
|
|
|
What is the response of the respiratory system to fear? Describe the mechanism |
-the hypothalamus sends signals once stress is perceived -sympathetic NS stimulates Adrenal medulla to secrete adrenaline/ noradrenaline -stimulation of corticotrophs (by CRH) causes release of ACTH which stimulates release of cortisol |
|
|
|
What does adrenaline / noradrenaline do? |
Increases alertness Blood flow to muscles Respiration rate Cardiac output |
|
|
|
What does cortisol do? |
Increases glucose metabolism Supresses the immune system |
|
|
|
Adrenaline receptors in the heart, blood vessels, lungs, uterus? |
Heart = B1 Blood vessels responsible for vasoconstriction = a1 Blood vessels responsible for vasodilation = B2 Lungs and uterus = B2 |
|
|
|
Describe the role of lungs in maintaining acid/ base balance: EQUATION |
H2O + CO2 ↔️ H+ + HCO3- |
|
|
|
What does an increase in CO2 cause? |
Causes equilibrium to shift right (more H+ is produced) |
|
|
|
What do central chemoreceptors detect? |
Change in H+ in CSF (from pH and CO2) |
|
|
|
What do carotid chemoreceptors detect? |
Detects change in PCO2, PO2 and pH |
|
|
|
What do aortic chemoreceptors detect? |
Change in PCO2 and PO2 |
|
|
|
How do the kidneys aid homeostasis by working with the lungs? Where are these ions reabsorbed? |
They reabsorb bicarbonate ions (mostly in the PCT)
H+ is excreted in the urine
Helps shift the equilibrium curve to the right |
|
|
|
What is the normal range of arterial blood gases for pH, pCO2, HCO3 |
pH = 7.35- 7.45 pCO2 = 35-45 mmHg HCO3 = 22-26 mEQ/L |
|
|
|
What are mucociliary escalator cells? |
Ciliated airway epithelial cells that line the surface of the large airways |
|
|
|
Mucociliary escalator cells function? |
Cilia beat in a coordinated manner waving foreign bodies out of the lungs |
|
|
|
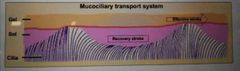
What are the three layers that make up the mucociliary transport system? These are found in the upper respiratory system |
Gel Solution Cilia |
|
|
|
What is the airway surface liquid made up of? |
An upper gel layer Periciliary solution layer |
|
|
|
What does the upper gel layer contain? |
Mucins (glycopeptides) which make up mucous |
|
|
|
What is the Peri-ciliary sol layer? |
A liquid layer which lubricates the cilia |
|
|
|
What is the process that takes place when the airway surface liquid contains too much fluid? What channels are used? |
-ENaC transports N+ into epithelial cell -Which causes water to move down its potential gradient into the epithelial cells -sodium is pumped into the blood via an Na+/K+ ATPase |
|
|
|
What happens when the airway surface liquid is too viscous? |
CFTR down regulated ENaC and also pumps Cl- into the airway surface liquid |
|
|
|
Cystic fibrosis and CFTR |
Cystic fibrosis is the result of a defect in the CFTR transmembrane receptor. This means that ENaC isn't down regulated. Therefore too much fluid is removed from the lungs and airway surface liquid is very viscous |
|
|
|
Done this already? |

|
|
|
|
What happens when allergens is inhaled? |
APC's activate naive T cells to become IL4 secreting TH2 helper cells. |
|
|
|
What does TH2 cells activate? |
Activate B cells and drive them to switch Ig isotype to IgE and become an IgE secreting plasma cell. |
|
|
|
What does IgE bind to? |
FC receptor on mast cells. This will then cause sensitized mast cells to degranulate when the pollen is next inhaled and binds to IgR |
|
|
|
Which pathogens cause tuberculosis? |
Microbacterium bovis Microbacterium tuberculosis |
|
|
|
What is TB transmitted by? |
Droplets |
|
|
|
What are the symptoms of TB? |
Persistent cough Fatigue Weight loss As the disease develops: Fever Coughing blood |
|
|
|
What does TB do to the body? |
Bacteria grow and divide in the upper region of the lungs. These get destroyed by the body's immune response.
But often some bacteria remain and re-emerge to cause a stronger post-primary TB.
The bacteria destroy lung tissue resulting in cavities and scar tissue. |
|
|
|
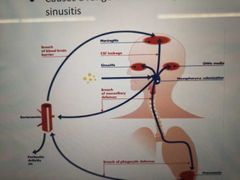
What does streptococcus pneumoniae cause? |
Pneumonia Meningitis Sepsis Otitis media (fluid between eardrum) Sinusitis |
|
|
|
What is the definition of a vaccination? |
The administration of antigenic material (a vaccine) to stimulate an individual's immune system to develop adaptive immunity to a pathogen |
|
|
|
Describe the vaccines response on the body |
-Dendritic cells are activated -Monocyte and neutrophils become APCs -APCs migrate towards germinal centre where T and B cells are activated -memory cells are produced |
|
|
|
What sort of pathogens do vaccines contain? |
Pattern-associated pathogens |
|
|
|
What is the immune response after a vaccine has being administered? |
A stronger, immediate secondary response is produced |
|
|
|
What is a long term active vaccine? |
Administration of an antigen (modified infectious agent or toxin) resulting in active production of immunity |
|
|
|
What is short term active vaccine? |
Administration of an antibody-containing serum or sensitised cells |
|
|
|
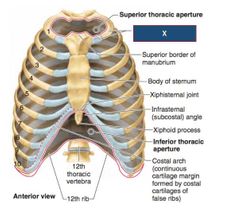
What is the bounderies of the Thoracic cavity? |
Body of T1, Medial margin of 1st rib and superior manubrium border |
|
|
|
What is the Thoracic aperture closed by? |
The diaphragm |
|
|
|
What is the Inferior Thoracic aperture bounded by? |
Bounded by the body of T12
Inferior margins of 11th and 12th ribs
The xiphoid process
|
|
|
|
What does the Thoracic cavity contain? |
Contains lateral pleura partitioned by the mediastinum |
|
|
|
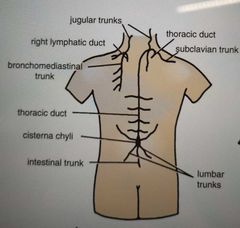
What does lymph pass through before returning to bloodstream? |
At least one lymph node |
|
|
|
The anterior Thoracic walls drain into which lymph nodes? |
Parasternal nodes Diaphragmatic nodes |

|
|
|
The posterior Thoracic wall drains into which nodes? |
Intercostal nodes (head and neck of ribs) |
|
|
|
Which nodes do the lungs drain into? |
Tracheobronchial nodes |
|
|
|
Where does the Thoracic duct begin? |
Cisterns chyli |
|
|
|
What does cisterna chyli drain into? |
Passes behind arch of aorta to enter the left brachiocephalic vein |
|
|
|
What are the anterior intercostals supplied by? |
Internal thoracic Coming off subclavian |
|
|
|
What are the posterior intercostals supplied by? |
Aorta |
|
|
|
What is the Venous drainage of the thoracic walls? |
Right side: The posterior intercostal veins drain into the azygous vein (4/5-12)
Left side: accessory hemiazygos (4-8) and hemiazygos vein (9-11)
The posterior intercostal vein of the first space drains into the left Brachiocephalic or azygous.
The left/ right superior intercostal vein is formed of 2nd, 3rd, sometimes 4th posterior intercostal veins which drains into the azygous vein on the right, and left Brachiocephalic on the left.
The hemiazygous and accessory hemiazygous vein drain into the azygous vein at the level T7-T8 |
|
|
|
What does the azygous vein receive? |
Receives lower 8 posterior intercostal veins, only on the right side of the body.
The right superior intercostal veins
First posterior intercostal vein
Hemiazygos and accessory hemiazygos veins |
|
|
|
What does the azygous veins drain into? |
Superior vena cava (T5-T6) |
|
|
|
What does the superior hemiazygous vein receive? |
Receives 4-8 left posterior intercostal veins |
|
|
|
What does the inferior accessory hemiazygous vein receive? |
Receives lowest (9-11) left posterior intercostal veins |
|
|
|
Is the ascending aorta anterior or posterior to the trachea? |
It's anterior |
|
|
|
What arteries does the ascending aorta give rise to? |
Coronary arteries |
|
|
|
The arch of aorta give rise to which arteries? |
Brachiocephalic Left common carotid Left subclavian |
|
|
|
The anatomical position of the descending aorta? |
Lies in the posterior mediastinum Runs downwards with oesophagus/ left lung and passes behind the diaphragm at T12 to become abdominal aorta |
|
|
|
What is an aortic aneurysm? |
Bulging / weakened area of the aorta resulting in ballooning to >50% more than vessels normal diameter and characterised by the location / shape / cause |

|
|
|
Once formed, what happens to an aneurysm? |
It will gradually increase in size and there will be a progressive weakening of the the aneurysm wall |
|
|
|
What is the treatment for an aortic aneurysm? |
Surgical repair or removal to prevent rupture |
|
|
|
What are some symptoms of aortic aneurysm? |
-Pain in chest /back -Wheezing -Shortness of breath (due to pressure on trachea) -Hoarseness due to pressure on vocal cords -Dysphagia due to pressure on oesophagus |
|
|
|
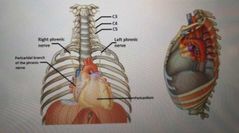
Where does the phrenic nerve originate from? |
From the cervical plexus |
|
|
|
What type nerve fibres does the phrenic nerve have? |
Motor / sensory / sympathetic |
|
|
|
What does the phrenic nerve supply? |
Motor supply to the diaphragm Sensation to the Tendon Mediastinal pleura Pericardium |
|
|
|
What vertebrates supply the diaphragm? |
C3/4/5 keep the diaphragm alive |
|
|
|
Anatomical pathway of the phrenic nerve? |
Enters superior mediastinum lateral to vagus nerve and behind brachiocephalic veins.
Passes anteriorly to the hilum of the lung and over the pericardium of the heart sending small pericardial branches to it |
|
|
|
What is the role of the Vagus Nerve (Cranial nerve 10)? |
Autonomic control of the heart and digestive tract |
|
|
|
What does the vagus nerve supply motor parasympathetic fibres to? |
To all organs except the suprarenal glands from the neck to the second segment of transverse colon Controls superior / middle / Inferior pharyngeal constructors and muscles of larynx |
|
|
|
Recurrent laryngeal nerve function? |
Sensory below vocal cords and motor to all except cricothyroid |
|
|
|
Superior laryngeal function? |
Gives off external and internal laryngeal |
|
|
|
Internal laryngeal nerve function? |
Sensory above vocal cords |
|
|
|
External laryngeal nerve function? |
Motor to cricothyroid |
|
|
|
What seperates Thoracic and abdominal aorta? |
The diaphragm |
|
|
|
What is the conducting zone vs respiratory zone? |
Conducting zone: Tip of nose to terminal bronchioles Respiratory zone: respiratory bronchioles to alveoli |
|
|
|
Pulmonary surfactant functions? |
-Prevents collapse of alveoli -Prevents small alveoli from joining with larger alveoli -increases lung compliance ANTI SURFACE TENSION |
|
|
|
What is respiratory rate? |
The respiratory rate is the rate at which breathing occurs. This is usually measured in breaths per minute and is set and controlled by the respiratory centre. |
|
|
|
What is minute ventilation? |
Minute ventilation is the volume of gas inhaled or exhaled from a person's lungs per minute. |
|
|
|
What happens to blood gases during hyperventilation and why? |
A decrease in PaCO2 of arterial blood |
During hyperventilation the rate of removal of carbon dioxide from the blood is increased. As the partial pressure of carbon dioxide in the blood decreases, respiratory alkalosis, characterized by decreased acidity or increased alkalinity of the blood, ensues. In turn, alkalosis causes constriction of the small blood vessels that supply the brain. |
|
|
How saturated is Haemaglobin at normal resting PO2 of mixed venous blood? |
Nearly 75% |
|
|
|
What is a component of internal respiration? |
Oxidative phosphorylation |
|
|
|
What is the optimum height of airway surface liquid for efficient clearance? |
7 micrometers |
|
|
|
What region containing olfactory epithelium containing bipolar sensory neurons? |
Sphenoethnoidal recess |
|
|
|
What region contains stratified squamous epithelial containing hair follicles? |
Nares (the nostrils) |
|
|
|
Where does the Sphenoid air sinus drain? |
Sphenoethmoidal recess |
|
|
|
Where does Maxillary sinus drain? |
Middle meatus |
|
|
|
Where does nasolacrimal duct drain? |
Inferior meatus |
|
|
|
Phrenic nerve summary: |
Origin: c3/4/5 cervical plexus Innervation: motor supply to diaphragm and sensory supply from the central tendon of diaphragm. Bilateral so there's a right and left phrenic nerve |
|
|
|
Laryngeal innervation summary: |
2 nerves, coming off the vagus nerve. First is the superior laryngeal: this splits into an internal and external branch. The internal branch provides sensory innervation to all muscles about the vocal cord. The external provides motor innervation to the cricothyroid muscle ONLY. The other nerve is the recurrent laryngeal. Supplies motor innervation to all of the muscles of the larynx apart rom the cricothyroid muscle. Supplies sensory to all the muscles below the level of the vocal cord. |
|
|
|
What does it mean if a person has high/ low HCO3- conc? |
Kidneys are trying to balance out H+ conc in the blood caused by too high it too low pCO2 |
|
|
|
What is ventilation? What is perfusion? What is diffusion? What is internal respiration? |
-Getting air into the lungs -Getting blood towards lungs -Gas exchange between blood and lungs -oxidative phosphorylation |
|
|
|
What is the upper vs lower respiratory tract? |
Upper: nose, mouth, pharynx, larynx Lower: tracheobronchial tree, alveoli |
|
|
|
What are the non obvious reasons for hypoxia? |
Cellular posioning: CO poisoning Cyanide poisoning |
|
|
|
Which arteries supply conducting zones vs respiratory zone? |
Conducting: bronchial arteries Respiratory: pulmonary artery (lungs totally dying is very unlikely since they have two blood supplies) |
|
|
|
Defensive functions of the conducting zone: |
Mucous Mucous escalator Macrophages |
|
|
|
Defensive role of the respiratory zone? |
Alveolar macrophages (dust cells) |
|
|
|
What is the pO2 in venous and arterial blood? |
Venous: 5 Arterial: 72 to 104? More like 20 maybe |
|
|
|
How to figure out where acidosis or alkalosis is compensated or uncompensated? |
Compensated when pH is normal levels despite pCO2 not being normal. Because additional HCO3- or H+ has dealt with it |
|
|
|
Which part of the brain allow voluntary control of breathing? |
Cerebral cortex |
|
|
|
During inspiration, is transpulmonary pressure greater or atmospheric? |
Atmospheric Things to remember: -intrapleural pressure is around - 3 -intrapulmomary pressure is same as atmospheric normally but with diaphragmic contraction it's - 1 |
|
|
|
What is solubility coefficient of a gas? |
I think how soluble the gas is in a particular liquid?
But at the Alveolar capillary interface, the rate of diffusion is directly proportional to the solubility coefficient of the gas. Remembers rate of diffusion and thickens are inversely proportional. |
|
|
|
What part of the lungs constricts in response to decreased pO2? |
Lung arteriole
Apparently in low oxygen states, pulmonary vessels constrict in an attempt to shunt blood away from poorly ventilated parts of the lungs to better ventilated parts |
|
|
|
What does decreased compliance of the lung mean? |
Lungs are stiff |
|
|
|
What other molecule is Haemaglobin capable of transporting? |
Carbon dioxide bound to globin |
|
|
|
Cells of the respiratory systen: |
Oral cavity: stratified squamous Conducting passageways: pseudostratified columnar (ciliated with goblet cells) Oropharynx and laryngopharynx: non-keratonised startifed squamous epithelium Bronchiole: simple cuboidal epithelium Type 2 Alveolar: cuboidal + granules |
|
|
|
What is the head of the rib? |
The part of the rib that connects with with the spinal cord posteriorly |
|

