![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
194 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are the bones function? |
Support body Protects organs Site for hematopoiesis Regulate mineral homeostasis |
|
|
|
What is hematopoiesis? |
Process of blood cell and platelet production in the bone marrow |
|
|
|
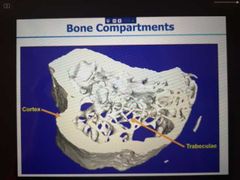
What are the different forms of bone? |
Trabecullar bone - spongy bone Cortical bone -compact |
|
|
|
Where is the cortical and trabecullae found? |
|
|
|
|
Why are the cortical and trabecullae bone ideal together? |
Together they allow bone to give support and mechanical strength whilst still being relatively lightweight |
|
|
|
What is found between the spaces in the trabecullae in the bone? |
Bone marrow
Yellow bone marrow: contains adipocytes
Red bone marrow: contains haematopoietic stem cells |
|
|
|
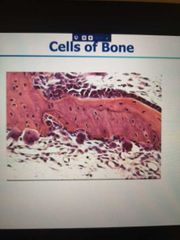
What is by far the most abundant bone cell? |
Osteocytes - will always see them in histology |
|
|
|
In histology, how do you spot osteoblasts? |
Osteoblasts can be spotted in histology sometimes, in clusters |
|
|
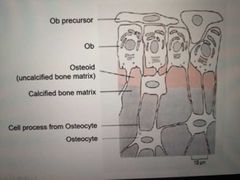
Label the 3 bone cells |
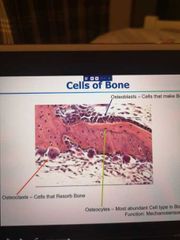
(normal bone does not look like this, this is a histological sample from an infected bone) |
|
|
|
What is osteoid? |
Unmineralised bone matrix |
|
|

Label this: |
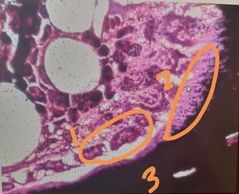
1) osteoblasts 2) osteoid 3) mineralised bone Dark speckles in the osteoid is where mineralisation has started to happen |
|
|
|
Osteoblasts: origin? What do they contain high levels of? Where are they almost always found? |
Mesenchymal origin High levels of enzyme alkaline phosphatase Secrete & respond to lots of growth factors and cytokines Active or inactive osteoblasts cover most bone surfaces |
|
|
|
Name some of the growth factors osteoblasts respond to? |
RANKL BMPS |
|
|
|
What are inactive osteoblasts? |
Flattened |
|
|
|
What happens when osteoblasts are incorporated into the bone matrix? (basically trapped) |
They become osteocytes |
|
|
|
How do osteocytes exist? |
As a big connected system of cells (their dendrites are in contact withe ach other and with the cells on the bone surface) |

|
|
|
What organelle is present in large amounts in osteoblasts and why? |
Rough ER Makes proteins - osteoids Large golgi complex to transport the proteins to outside the cell Secretory vessels |
|
|
|
What is required to differentiate mesenchymal progenitor into osteoblasts? |
Series of transcription factors |
|
|
|
Why is collagen type 1 a good component for bone? |
A key structural protein which gives bone strength and elasticity too (w/o it bone would be too brittle) |
|
|
|
What is the major organic component of bone? |
Type 1 collagen (90% of bone is this) |
|
|
|
Where else is type 1 collagen found? |
In tendons, ligaments, skin and scar tissues. Most prominent protein in the body. Found everywhere to provide structural support |
|
|
|
What is the remaining 10% of bone made up of? |
Mixture of:
Growth factors (TGfBeta) Osteocalcin Osteonectin Glycoproteins Osteopontin (involved in bone mineralisation) |
|
|
|
What is Osteocalcin? |
Bone formation marker- secreted by osteoblasts into blood during bone formation so is a good diagnostic component that can be measured to see how much bone formation is happening |
|
|
|
Bone is a major store for which growth factor? |
Tgfbeta |
|
|
|
What are the two types of bones formation? |
Lamellar Woven |
|
|
|
Which bone is stronger? |
Lamellar is stronger |
|
|
|
How to identify a histology of lamellar bone? |
Has straight lines called lamellae (sheets of bones) |

|
|
|
Histology of woven bone? |

|
|
|
|
How is woven bone produced? |
Osteoblasts rapidly produce unmineralised osteoid with the collagen fibres arranged randomly. This is a temporary structure and is soon replaces by lamellar bone |
|
|
|
When is woven bone formed? |
Embryonic development Fracture repair |
|
|
|
How is lamellar bone formed? |
Regular parallel alignment of collagen into sheets (made of mineralised osteoid) |
|
|
|
What gives lamellar bone its strength? |
Collagen fibres run parallel so increase strength In cross sections fibres run in opposite directions assisting the resistance of torsion forces |
|
|
|
What is bony substitution? |
When the woven bone is replaces by lamellar bone. Formation of lamellar bone is a much slower process (mineralisation of osteoid takes a few days at least) |
|
|
|
Lamellar bone can be divided into two different bones. What are they? |
Trabecullar Cortical |
|
|
|
The light, porous nature of trabecullar bone allows for what? |
Resistance against multi directional lines of forces
Also crucial for allowing the body to move |
|
|
|
Difference between strength provided by trabecullar and compact bone? |
Trabecullar - resists forces to a certain degree from all angles Compact- resists forces from one angle with a great degree |
|
|
|
What is bone deposition? |
A Crystallisation process in which calcium and phosphate ions (amongst others) are taken from the blood plasma and deposited in bone tissue as crystals of hydroxyapatite |
|
|
|
Describe the process of bone deposition |
1) Osteoblasts synthesise + secrete (osteoid, most of which is) collagen fibrils
2) these polymerise to form collagen strands
3) calcium and phosphate precipitate crystallises on collagen (which acts as a scaffold) to form hydroxyapatite 4) Ob secrete vesicles containing enzyme alkaline phosphatase which acts as the centre for calcium and phosphate deposition
5) the vesicles then rupture and act as centres for crystals to grow on
|
|
|
|
Function of compact bone? |
Protection + support to the bone Protects spongy bone |
|
|
|
Function of trabecullar bone? |
Protects red and yellow marrow Resist stress in all directions |
|
|
|
Function of trabecullar bone? |
Protects red and yellow marrow Resist stress in all directions |
|
|
|
Where is red bone marrow found? |
Hip bones Ribs Sternum Vertebrae Proximal end if humerus and femur This tehse are the sites for hematopoiesis |
|
|
|
What is collagen and where (molecular level) is it found? |
Structural protein in extracellular space of various connective tissues |
|
|
|
Is collagen rigid or compliant? |
Can be both, depending on the degree of mineralisation |
|
|
|
What is collagen secreted by? |
Fibroblast Osteoblast |
|
|
|
Why do bones get weaker as we grow older? |
Osteoblast activity lessens compared to osteoclasts activity - decreasing the density of bone |
|
|
|
What do osteocytes do? |
They can sense mechanical loading on the bone and then send signals to osteoblasts and osteoclasts which reshape bone density |
|
|
|
What is bone turnover? |
Total volume of bone resprbed and formed over a period of time |
|
|
|
What is bone remodelling? |
An active process which is essential for calcium homeostasis and preserving the skeleton through the use of osteoclasts and osteoblasts |
|
|
|
Describe the process of bone remodelling in 6 stages |
Activation, Resorption, Reversal, Formation, Mineralisation, quinesence |
|
|
|
What happens in activation |
Surface protein RANKL on osteoblasts binds to RANK surface protein on osteoclasts to cause the osteoclast precursors to differentiate into mature osteoclasts |
|
|
|
What happens in resorption |
Osteoclasts release acid and lysosomal enzymes on the bone surface to break down bone and release calcium into the blood stream |
|
|
|
What happens in reversal? |
Macrophage like cells found at the site of remodelling |
|
|
|
What happens during formation and mineralisation? |
Osteoprogenitor cells proliferate and differentiate unto osteoblasts - which secrete collagen and other organic matter to form a ECM. The matrix then mineralises and the osteoblasts become trapped - forming osteocytes |
|
|
|
What is the role of sex hormones on bone remodelling? |
-increase osteoblast activity -estrogen promotes widening if pelvis in females and other changes -shuts down growth at the epiphyseal plates so bone stops getting longer. Females have higher levels of oestrogen thus their growth of bones ends earlier |
|
|
|
What is osteoporosis? |
Bone weakness; increased risk of fractures due to decreased bone deposition or increased bone resorption |
|
|
|
What is osteopetrosis? |
Inherited bone disease which causes increased bone mass due to dysfunctional osteoclasts - hence matrix can't be degraded |
|
|
|
What is the functional unit of the bone? |
The osteaon |
|
|
|
What are the two canals present in the bone? |
Haversian's canal Volkmann's canal |
|
|
|
What does an osteon consist of? |
Concentric lamellae (circular, mineralised plates) around a Haversian canal |
|
|
|
What is a Haversian canal? |
Vertical canal in the middle of an osteon which has blood vessels, lymphatic vessels running through it |
|
|
|
What is present between the concentric lamellae? |
Lacunae which hold osteocytes (think of the lucanae as tunnels in the soil - a space which holds the osteocytes) |
|
|
|
What is the name of the small channels that radiate put from the lucunae and what do they contain? |
Canaliculi Filled with extracellular matrix |
|
|
|
What is the function of the canaliculi? |
Connects one lucanae to another. Though which dendrites of osteocytes pass through and connect to other osteocytes. Forming an interconnected system throughout the bone |
|
|
|
How do the osteocytes in the canaliculi communicate? |
Through gap junctions |
|
|
|
Why is the network of osteocytes important? |
Facilitates exchange of nutrients and metabolic waste through out the bone |
|
|
|
What are Volkmann's canals? |
Horizontal canals running through the bone which allow blood vessels and nerves from the periosteum to penetrate into the compact bone. They link with the Haversian canals to form a nerwork |
|
|
|
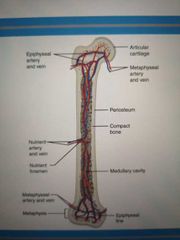
Where is the medullary cavity found? |
In the middle of a long bone |
|
|
|
What does the medullary cavity contain? |
Nutrient artery And 2 veins |
|
|
|
Where does the nutrient artery enter the bone? |
Through the nutrient foramen, the hole in the side of the bone and it branches to each end of the bone |

|
|
|
What does the nutrient artery do? |
Provides blood supply to inner section of the bone |
|
|
|
Define the structure of cartilage? How many zones does cartilage have? What are the names starting from superficial? |
4 zones
Zone 1: tangential zone Zone 2: transitional zone Zone 3: radial zone Zone 4: calcified cartilage |

|
|
|
In terms of size, Elastin fibres or collagen fibres? |
Elastin |
|
|
|
Where is cartilage found? |
In cartilage |
|
|
|
Name the 3 types of cartilage |
Hyaline cartilage Elastic cartilage Fibrocartilage |
|
|
|
Where is hyaline cartilage found? |
Synovial joint In movable joints like nose, ears |
|
|
|
What is Hyaline cartilage made up of? |
Widely dispersed fine collagen fibres (type II). Has Perichondrium present |
|
|
|
Which is the weakest type of cartilage? |
Hyaline |
|
|
|
What is Perichondrium? |
The connective tissue that envelops cartilage where it is not at a joint |
|
|
|
Describe the structure and function of elastic cartilage |
ECM is cross crossed with elastic fibres - gives flexibility + resilience to ECMOuter margins defined by a fibrous Perichondrium
Outer margins defined by a fibrous Perichondrium Outer margins defined by a fibrous Perichondrium Outer margins defined by a fibrous Perichondrium
|
|
|
|
What does the fibrous Perichondrium contain? |
Collagen fibres, fibroblasts and chomdroblasts |
|
|
|
Examples of where elastic cartilage can be found? |
Outer ear Larynx |
|
|
|
Fibrocartilage / fibrous cartilage structure and function |
No Perichondrium Strongest cartilage Prominently made up of collagen I |
|
|
|
Why is fibrocartilage so strong? |
Due to alternating layers of hyaline cartilage matrix and dense collagen fibres |
|
|
|
Where is fibrocartilage usually found? |
Forms a transitional layer between cartilage, ligament or Tendon. Places which require resistance against compressive forces. In the spine |
|
|
|
Examples of fibrocartilage |
Public symphysis Intervertable discs Temporomandibular joint |
|
|
|
What role of chondrocytes in growth? |
Produce and maintain the cartilaginous matrix
|

|
|
|
Through what pathway are chondrocytes made? |
Mesenchymal stem cell - chondrogenic cells - chomdroblasts - chondrocytes |
|
|
|
Functions of calcium, phosphorus, magnesium, fluoride, manganese in bone growth? |
Calcium - calcifies ECM Phosphorus - calcifies ECM Magnesium - helps form bone ECM Fluroide - helps strengthen bone ECM Manganese - activates enzymes involved in synthesis of bone ECM |
|
|
|
Role of the vitamins in controlling and modifying bine growth |
A :osteoblast stimulation C :collagen synthesis D :for uptake of Ca2+ from gut K and B12 :synthesis of bone protein |
|
|
|
What is the active form of Vitamin D and where is it produced? |
Calcitriol In the kidneys |
|
|
|
Role of hormones in bone growth: Growth hormone |
Promotes growth by stimulating IGF's |
|
|
|
Role of hormones in bone growth: insulin-like growth factors |
Secreted by the lover and bones on stimulation by GH - stimulated osteoblasts and increases synthesis of bone proteins |
|
|
|
Thyroid hormones (T3 and T4) function of bone growth |
Stimulate osteoblasts |
|
|
|
Insulin, effect on bone growth |
Promotes synthesis of bone proteins |
|
|
|
Why can damage to cartilage be serious? |
Non vascular tissue Mineral diffuse through tissue to provide nutrition - slow process So healing is v slow and likely to cause damage |
|
|
|
Describe what are the two types of ossification? |
Intramembranous ossification Endochondrial ossification processes |
|
|
|
What bones does intramembranous ossification occur for? Where does it take place? |
For flat bones of the skull Mandible Medial part of clavicle
Develops from fibrous connective tissues |
|
|
|
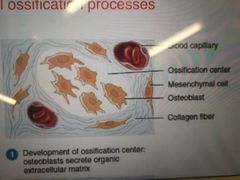
Briefly describe intramembranous ossification? |
Development of ossification Centre Calcification Formation of trabeculae Development of periosteum |
|
|
|
Describe the formation of the ossification Centre : intramembranous |
Mesenchyme cluster and differentiate into osteoprogenitor Which differentiate into osteoblasts Which secrete extracellular matrix (osteoid) till they're completely surrounded |
|
|
|
Describe Calcification : intramembranous ossification |
Osteoid is calcified. Calcium and other mineral salts are deposited and alkaline phosphatase catalyses Calcification |
|
|
|
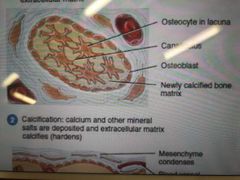
Describe the formation of trabeculae : intramembranous ossification |
ECM develops into trabeculae Which fuse to form spongy bone around a network of blood vessels
Red bone marrow forms in between the spaces |
|
|
|
Describe the development of periosteum :intramembranous ossification |
Mesenchyme at the periphery condenses to form periosteum
Thin layer of compact bone replaces surface spongy bone |
|
|
|
What are lacunae? |
Hollowed out spaced which osteocytes live in |
|
|
|
What is an ossification Centre? What is ossification? |
Where ossification takes place Process by which bone is produced |
|
|
|
What are chondrocytes? |
Cells that make up cartilage and produce a matrix consisting of collagen |
|
|
|
What are the 6 stages of Endochondrial ossification? |
Development of cartilage model Growth of cartilage model Primary ossification Centre forms Medullary cavity forms Secondary ossification centres form Articular cartilage + epiphyseal plate |
|
|
|
Step 1: Development of cartilage model |
Mesenchyme gather in the shape of bone, differentiate into chomdroblasts : these secrete cartilage ECM. Forming a cartilage model |
|
|
|
What does the cartilage model consist of? |
Hyaline cartilage and a Perichondrium which surrounds it |
|
|
|
Step 2: Growth of cartilage model |
Chondroblasts surrounded by cartilage ECM become chondrocytes. These divide and produce more cartilage ECM so cartilage model grows in length. The chondrocytes in the centre increase in size and the surrounding ECM calcifies. Chondrocytes within the calcifying cartilage die. Spaces left behind by dead form lacunae |
|
|
|
Why do chondrocytes die? |
Nutrient supply is blocked by calcified cartilage |
|
|
|
What type of growth is involved in endochondral ossification? What does it mean? |
Interstitial growth (growth from within. When chondroblasts in lacunae secure ECM and then divide, the cartilage expands) |
|
|
|
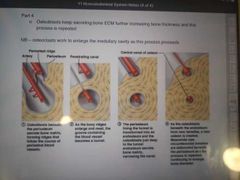
Step 3: development of primary ossification Centre |
Nutrient artery penetrates through Perichondrium and calcified cartilage model. Stimulated osteoprogenitor cells in Perichondrium to differentiate into osteoblasts. The periosteal capillaries grow into the cartilage and Stimulate formation of primary ossification Centre. Osteoblasts secrete osteoid over the remaining calcifies cartilage model to form spongy bone |
|
|
|
When osteoblasts are produced, what does the name of the Perichondrium change to? |
Periosteum |
|
|
|
Through what gap does the nutrient artery enter the cartilage emodel through? |
Nutrient foramen |
|
|
|
Step 4: development of medullary cavity |
Osteoclasts break down spongy bone leaving a medullary cavity in the diaphysis. The wall of the medullary cavity undergoes bone remodelling to form compact bone |
|
|
|
Step 5: development of secondary ossification centres |
When branches of epiphyseal artery reach epiphysis, secondary ossification centres develop Spongy bone remains at the centre of the epiphysis |
|
|
|
Which direction does secondary ossification proceed? |
Outwards, towards the outside surface of the bone from the epiphysis |
|
|
|
Step 6: formation of articular cartilage and epiphyseal plate |
Hyaline cartilage covering epiphysis becomes articular cartilage |
|
|
|
What remains between the epiphysis and the diaphysis until adulthood? |
The epiphyseal plate made of Hyaline cartilage as the expansion of this is responsible for the lengthening of bone |
|
|
|
How does growth of cartilage in step 2 occur in thickness? |
New chondroblasts developing from the perichondrium release ECM on surface of cartilage model (appositional growth) |
|
|
|
Endochondral ossification in one sentence? |
Replacement of cartilage with bone |
|
|
|
Where does appositional growth occur? |
Of course the surface of the cartilage. The surface of the diaphysis, growing from up |
|
|
|
What are the four zones of the epiphyseal plate? |
(epiphysis end) Zone of resting cartilage Zone of proliferating cartilage Zone of hypertrophic cartilage Zone of calcified cartilage (diaphysis end) |
|
|
|
Zone of resting cartilage |
Cells don't function in bone growth Anchor epiphysis to epiphyseal plate |
|
|
|
Zone of proliferating cartilage |
-Made up of larger chondrocytes arranged in columns -undergo interstitial growth and make more chondrocytes to replace ones calcified at the diaphysis end |
|
|
|
What hormones determine the length of the columns of the proliferative chondrocytes? |
PTHrP IHH |
|
|
|
Zone or hypertrophic cartilage |
Consists of large chondrocytes |
|
|
|
Zone of calcified cartilage |
Cartilage ECM surrounding chondrocytes is calcified Eventually calcified cartilage is replaced by bone through Endochondrial ossification |
|
|
|
How does a bone grow in width - describe appositional growth? |
-periosteal cells differentiate into osteoblasts which secrete osteoid -osteocytes develop, ridges form either side of the periosteal vessel -ridges fold together and create a tunnel enclosing the blood vessels -periosteum to endosteum -osteoblasts in endosteum secrete osteoid forming new concentric lamellae, narrowing the tunnel. -repeat |
|
|
|
What hormone is responsible for causing elongation of bone to cease? |
Oestrogen |
|
|
|
When does Perichondrium become known as periosteum? |
When the epiphyseal artery enters the bone, gaining blood supply |
|
|
|
Bone can only undergo one type of growth? |
Appositional NOT interstitial That's with cartilage |
|
|
|
Only type of cartilage to not have a Perichondrium? |
Fibrocartilage |
|
|
|
Muscles are excitable tissues.. What does 'excitable' mean? |
Electrical excitability - the ability to respond to certain stimuli by producing an action potential triggered by autorythmic electrical signals or chemical stimuli |
|
|
|
What are the different types of muscles? |
Voluntary Smooth Cardiac |
|
|
|
Discuss microscopic features for all three muscles |
Skeletal : unbranched, multi nucleated, striated Cardiac muscles : Branched, single nuclei, striated. Fibres joined to each other by intercalated discs Smooth muscles: thickest in the middle, tapered at the ends. Not striated. One nucleus |
|
|
|
Discuss location of the 3 muscles |
Skeletal : around bones
Cardiac : heart
Smooyh: walls of hollow organs/ parts. Blood vessels, Airways |
|
|
|
Discuss fibre diameter of the muscles |
Skeletal : very large (10-100 micro) Cardiac: large (10-20 micro) Smooth: small (3-8 micro) |
|
|
|
Connective tissue component in the three muscles |
Skeletal : endomysium, perimysium, epimysium Cardiac: endomysium and perimysium Smooth: endomysium |
|
|
|
Are all the proteins organised into sarcomeres? |
Smooth muscle isn't |
|
|
|
How much sarcoplasmic reticulum do the muscles have? |
Skeletal ; a lot Cardiac ; some Smooth ; very little |
|
|
|
What are the junctions between each fibre? |
Skeletal : none Cardiac : intercalated discs which contain gap junctions and demosomes
Smooth: gap junctions in visceral (single celled) smooth muscle - none in multiunit smooth muscle |
|
|
|
Source of Ca 2+ for contraction in the different muscles |
Skeletal : sarcoplasmic reticulum Cardiac : sarcoplasmic reticulum and interstitial fluid Smooth: sarcoplasmic reticulum and interstitial fluid |
|
|
|
Nervous control for the muscles |
Skeletal; voluntary (somatic nervous system) Cardiac ; involuntary (autonomic nervous system) Smooth : involuntary (autonomic nervous system) |
|
|
|
Contraction regulation |
Skeletal; acetylcholine released by somatic motor neurons Cardiac: acetylcholine and norepinephrine Smooth; acetylcholine and norepinephrine |
|
|
|
Speed of contractions for the 3 muscles |
Skeletal - fast Cardiac - moderate Smooth - slow |
|
|
|
What are the different types of skeletal muscles? |
Type 1 - slow oxidative fibre Type 2a - fast oxidative - glycolytic fibre (FOG) Type 2b - fast glycolytic fibre (FG) |
|
|
|
Structural characteristics of Slow oxidative fibres |
Many mitochondria Many capillaries Large myoglobin content Red in colour |
|
|
|
Fast oxidative - glycolytic fibres |
Many mitochondria Many capillaries Large amounts of myoglobin Red- pink in colour |
|
|
|
Fast glycolytic fibres structural characteristics |
Few mitochondria Few capillaries Small amounts of myoglobin content White in colour |
|
|
|
Where are slow oxidative fibres abundant? And their primary function |
Postural muscles such as those of the neck - maintain posture and aerobic endurance activity |
|
|
|
Where are fast oxidative glycolytic fibres abundant? Their primary function |
Lower limb muscles - walking and sprinting |
|
|
|
Fast glycolytic fibres location and primary function |
Upper limbs muscles - rapid, intense movements of short duration |
|
|
|
Capacity for generating ATP and method used in each of the 3 skeletal muscles |
Slow oxidative fibre - high and aerobic respiration Fast oxidative - glycolytic fibres - intermediate by both aerobic and anaerobic glycolysis Fast glycotic fibres - low by anaerobic glycolysis |
|
|
|
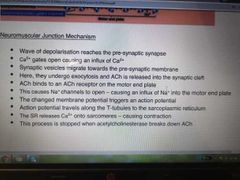
Describe neuromuscular Junction mechanism |
|
|
|
|
Where are the ACh receptors in a neuromuscular Junction? |
Motor end plate |
|
|
|
What does the action potential travel along to get to the sarcoplasmic reticulum? |
T-tubule |
|
|
|
When I muscle contractions stopped? |
When acetylcholinesterase breaks down ACh |
|
|
|
What is sarcoplasmic reticulum? |
Like endoplasmic reticulum. It sprees calcium ions |
|
|
|
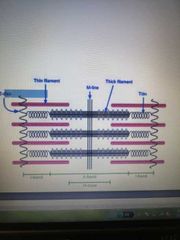
What is a sarcomere? |
Repeating unit between 2 Z lines |
|
|
|
What is the thin filament and the thick filament? |
Thin : actin Thick : myosin |
|
|
|
Sliding filament theory? |
Access A-level muscle set |
|
|
|
What are the intracellular functions of calcium? |
Signal transduction Muscle contraction Hormone secretion |
|
|
|
Calcium ectraceular functions |
Mineralises skeleton-hydroxyapatite Co-factor in clotting cascade Nerve conduction Neurotransmitter release |
|
|
|
Quantities calcium is present in intracellularly and extracellularly |
Intra : less than 100nmol/L Extra: 2.2 - 2.6 mmol/L |
|
|
|
How are calcium levels maintained? |
Controlling calcitonin secretion Controlling PTH secretion |
|
|
|
Calcium and calcitonin |
-parafollicular cells in the thyroid gland detect too much Ca2+ in the blood and secrete calcitonin -which Inhibits osteoclast activity thus decreasing blood Ca2+ levels |
|
|
|
Calcium and PTH |
-Parathyroid gland cells detect low Ca2+ in blood so secrete PTH -Promotes resorption if bone ECM (osteoclast) this releasing Ca2+ into blood, increasing Ca2+ levels -PTH decreases loss of Ca2+ through kidneys into urine -PTH stimulates kidneys to convert vitamin D into Calcitriol - which increases resorption of Ca2+ from the gut into the blood |
|
|
|
Where is phosphate found in the body? |
85% in the bone |
|
|
|
What affects phosphate levels in the body? |
Age Food intake Time of day |
|
|
|
Describe the functions of phosphate |
-Structural components : hydroxyapatite and cell membrane phospholipids -Energy production -intracellular signalling -acid/ base balance
|
|
|
|
Through what process are phosphate levels maintained? |
Secretion of PTH decreases phosphate levels Calcitriol increases FGF24 (fibroblast growth factor) decreases |
|
|
|
How does PTH decrease phosphate levels? |
Reduces the resorption of phosphate in kidneys so they're extreted |
|
|
|
How does Calcitriol raise phosphate levels? |
Promotes phosphate absorption in the intestines. (same with calcium) |
|
|
|
How does FGF23 decrease levels of phosphates? |
Reduces resorption of phosphates from urine in the kidneys |
|
|
|
What can occur of extracellular fluid concentration of calcium is too low? |
Hypocalcaemia |
|
|
|
What are some symptoms of hypocalcaemia? |
Paraesthesia (pins and needles) Seizure Handm feet spasm |
|
|
|
Hyper calcaemia symptoms? |
Lethargy Anorexia Constipation Hallucinations Bradycardia Heart block Kidney stones Renal failure |
|
|
|
What causes rickets? |
Vitamin D deficiency due to a lack of UVB exposure, covered skin, renal failure, malabsorption |
|
|
|
Rickets symptoms? |
Pain in bones Stunted growth Bone fractures Muscle cramps Bowlegs |
|
|
|
What are the 3 cells unique to bone? What is their general function? |
Osteoblasts - bone making cells Osteoclasts - cells that resorb bone Osteocytes--mechanosensor cells |
|
|
|
How to spot osteoclasts? |
Multinucleated |
|
|
|
What is the rarest type of bone cell? |
Osteoclasts - usually hint the person isn't very healthy |
|
|
|
Briefly describe the life cycle of an osteoblast |
1) The mesenchynal osteoblast precursor differentiate into ob in response to cytokines etc... 2) Ob produce osteoid (unmineralised) 3) Ob also regulates the mineralisation of the osteoid 4) some of the ob become trapped and form osteocytes |
|
|
|
How is lamellar bone formed? |
Regular parallel alignment of collagen into sheets aka lamellae (made of mineralised osteoid) |
|
|
|
What Inhibits osteoblasts? |
Sclerostin expressed in osteocytes/ some chondrocytes |
|
|
|
What is cartilage? |
Connective tissue that consists of chondrocytes surrounded by ECM |
|
|
|
What properties does cartilage have? |
Weight bearing |
|
|
|
What does ECM consist of? |
Collagen 2,4,9,11 Acan Elastin |
|
|
|
Cartilage is A and A... |
Avascular aneural |
|
|
|
The role of water in cartilage tissue? |
Maintains resilience of tissue Nutrition and lubrication aid |
|
|
|
Cardiac muscle properties |
Striated, shorter, branched, connected by intercalated discs and contain a centrally located nucleus. |
|
|
|
What allows cardiocytes to propagate electrical impulses? |
Branched cells and intercalated discs |
|

