![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
244 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Name the major endocrine glands |
Hypothalamus Pituitary Thyroid Parathyroid Pancreas Adrenal glands/ suprarenal |
|
|
|
What is a gland? |
Glands = collection of cells that makes and releases a substance for biological use |
|
|
|
What are EXOCRINE glands? Give 2 examples |
Secrete directly onto target via duct Salivary glands, sweat glands |
|
|
|
What is an ENDOCRINE gland? |
No duct Secrete into interstitial fluid and transported to target indirectly via bloodstream |
|
|
|
What gland is it likely to be if it is directly next to target organ? |
Exocrine |
|
|
|
If a hormone released by a gland effects multiple different parts of the body, what type of gland is it likely to have been released by? |
Endocrine |
|
|
|
What two other parts of the body composition are unexpectedly endocrine? |
Bone Fat |
|
|
|
What is the hypothalamus made of? |
Collection of nuclei (gray matter) at the base of the brain |
|
|
|
Describe the anatomical position of the hypothalamus |
Forms part of the wall and the 3rd ventricle |
|
|
|
What is the function of the hypothalamus? |
Link neurosensory system to endocrine system Coordinates ANS (unconscious) and ENDOCRINE |
|
|
|
Hypothalamus is also a site for many... |
Converging and diverging neural pathways. Hypothalamus has connections to lots of different parts of the brain and body |
|
|
|
Where does the hypothalamus receive info from? |
Neurons Blood CSF (cerebral spinal fluid) |
|
|
|
What is the ventricle in the brain full of? |
CSF |
|
|
|
What are the nuclei in the hypothalamus made of? |
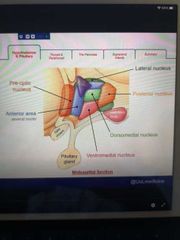
Small neurones arranged into functional groups. Each nuclei is responsible for different functions. (learn these seperate positions) |
|
|
|
What are some of the roles in the body that the hypothalamus is responsible for? |
Thermoregulation Osmoregulation Satiety ANS control |
|
|
|
Why is anatomical descriptions used for the different nuclei? |
Useful for imaging assessment |
|
|
|
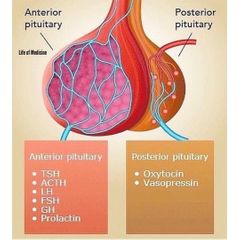
What is the pituitary gland made up of? |
Anterior part Posterior part |
|
|
|
How is the pituitary gland linked the the hypothalamus? |
The posterior part is an Extention of the hypothalamus |
|
|
|
Where physically does the pituitary gland sit? |
In the pituitary fossa of the skull - completely surrounded by bone |
|
|
|
How is the hypothalamus linked to the pituitary gland physiologically? |
Hypothalamus Coordinates the release of hormones from the pituitary gland. Does it differently for the anterior and posterior pituitary (since posterior is linked by neurones and anterior isn't) |
|
|
|
Key hormones of anterior pituitary gland - target organ - what is stimulates in target organ |
Prolactin - mammary glands - milk production Growth - MSK - growth, cell reproduction / regeneration Thyrotropin - thyroid gland - T3, T4 production Adrenocorticotropic - Adrenal Cortex- releases cortisol Gonadotropins (FSH/ LH) - ovaries/ testes |
|
|
|
How does the pituitary gland release hormones? |
In response to hormones releases by the Hypothalamus |
|
|
|
What are the two types of hormones the hypothalamus releases? |
Releasing hormones (RH) Inhibitory hormones (IH) |
|
|
|
Prolactin IH is also known as? |
Dopamine |
|
|
|
What is the function of the posterior pituitary gland? |
Stores and secretes the hormones produced by the Hypothalamus, doesn't synthesise any of its own hormones |
|
|
|
What are the 2 hormones secreted by the posterior pituitary gland? |
Vasopressin (Anti diuretic hormone) Oxytocin |
|
|
|
What connects the posterior pituitary gland to the hypothalamus? |
Infundibulum |
|
|
|
Hormones produced in the hypothalamus reach the pituitary by two way? In anterior and posterior? |
Anterior via portal blood vessels Posterior via neuroendocrine cells |
|
|
|
Which nuclei influence parasympathetic activity? (rest and digest) |
Pre-optic Anterior hypothalamic area |
|
|
|
Which nuclei influence sympathetic activity? (fight or flight) |
Posterior Lateral |
|
|
|
Which nucleus influences pituitary activity? (hormonal homeostasis) |
Anterior nuclei |
|
|
|
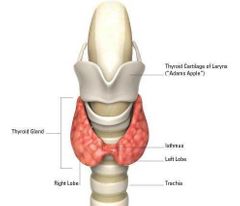
What is the scientific name for Adams apple? |
Laryngeal prominence |
|
|
|
What connects the two lobes of the thyroid? Over what tracheal rings are these? |
Isthmus 2-4 |
|
|
|
What is the top and bottoms of the thyroid gland called? |
Apex base |
|
|
|
What 3 main hormones does thyroid release |
Thyroxine (T4) Tri-idothronine (T3) Calcitonin (lowers blood calcium) (T tells you it's made in thyroid and number is number of iodine) |
|
|
|
Is T3 or T4 more active? Which does body produce more and what happens when that molecule enters cells? |
T3 Thus T4 is produced more, which is broken down into T3 when it gets to cells |
|
|
|
What do T3 and T4 do? |
Increase basal metabolic rate Increase body temp (calorigenic effect) Stimulates protein synthesis (growth and development) Inhances catecholamines |
|
|

Identify following on an ultrasound |
As seen in pic |
|
|
|
Thyroid development in an embryo |
At 4 weeks; Invagination of endoderm in pharynx floor - grows into "thyroid diverticulum". Then develops a thyroid gland at the end of it by week 5 |
|
|
|
How can thyroglossal cysts form? |
Thyroglossal duct may remain open and a gathering of mucus within it leads to infection |
|
|
|
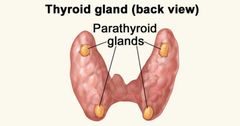
How many parathyroid glands are there? |
4, in each corner at the posterior of the thyroid glands |
|
|
|
What is the Parathyroid gland secretion controlled by? |
Calcium levels in blood |
|
|
|
What does the secretion of Parathyroid hormones cause? |
Increases calcium levels by releasing calcium from bones and increasing the amount of calcium absorbed at the small intestines. When Ca2+ levels are too high, less PTH is produced |
|
|
|
Is Pancreas an endocrine or exocrine gland? |
Both More than 95% is exocrine |
|
|
|
What organ is it intricately related to? |
Duodoneum |
|
|
|
What type of structural gland is the Pancreas? |
Lobulated |
|
|
|
What does the Pancreas consist of |
Head Neck Body Tail |
|
|
|
What is the endocrine part of the Pancreas called? |
Clusters of cells called islets of langerhans |
|
|
|
Key hormones produced by Pancreas |
Glucagon: increases bg Insulin Somatostatin : decreases release of pancreatic hormones and muscle contraction Vasoactive intestinal peptide (VIP) Pancreatic polypeptide (PP) |
|
|
|
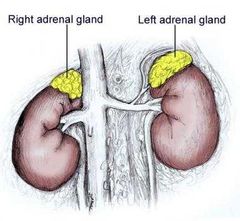
Where do you find suprarenal glands? Aka Adrenal glands |
Upper poles of kidneys |
|
|
|
What are the shapes or right and left suprarenal glands? |
Right is a pyramid Left is a crescent |
|
|
|
How many different layers of tissue do the Adrenal glands have? What are their names? |
3 Capsule Cortex Medulla |
|
|
|
How many zones does the Cortex have and what is produced in each zone? |
Zona glomerulus - aldosterone Zona fasciculata - cortisol Zona reticularis - sex hormones |
|
|
|
What does the medulla produce? |
Catecholamines (adrenaline/ noradrenaline) |
|
|
|
Is kidneys an endocrine organ? |
Yes |
|
|
|
Kidneys produce a hormone vital for Red blood cell production called? |
Erythropoetin (EPO) |
|
|
|
Describe the RAAS |
Pathway designed to increase blood pressure |
|
|
|
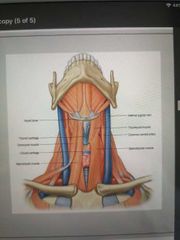
What does the thyroid gland wrap around? |
Cricoid cartilage |
|
|
|
Thyroid position anatomy |
In visceral compartment of the neck Between C5-T1 Below thyroid cartilage of larynx Anterior to the upper trachea and cricoid cartilage |
|
|
|
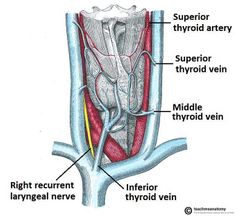
Arterial blood supply to the thyroid gland. 2 x pathways |
Common carotid External carotid Superior thyroid artery (feed tops of thyroid gland with blood)
Subclavian artery Thyrocervical trunk Inferior thyroid artery (feed bottoms of thyroid gland with blood) |

|
|
|
What 3 veins drain the thyroid gland of its blood? |
Superior thyroid vein Middle thyroid vein Inferior thyroid vein |
|
|
|
Where does the blood from the 3 thyroid veins go? |
Superior and middle thyroid veins drain into the internal jagular vein
The Inferior drain into brachiocephalic veins |
|
|
|
Describe the embryology of the thyroid gland. Where does it originally develop? What is the embryological remnant? |
Base of the tongue Foremen caecum |
|
|
|
Where does the thyroid go, through what? |
Descents from base of tongue to base of neck at the level of cricoid cartilage via thyroglossal duct |
|
|
|
What happens at the end of week 5? What has happened by the 6th weeks? |
Thyroglossal duct degenerates Then Throid has reached itrs destination |
|
|
|
What are the functional units of the thyroid? |
Follicular cells |
|
|
|
What are follicular hormones cells responsible for? |
Production and secretion of T3 and T4. They're also TSH (thyroid stimulating hormone) dependent |
|
|
|
What cells are found interlocking between follicular cells and what is their function? |
C-cells / parafollicular cells These produce calcitonin (calcium homeostasis) |
|
|
|
What are the target cells for T3 and T4? |
Cells in all tissue types |
|
|
|
Describe thyroid hormone action |
Binds directly to nuclear receptors THR receptors and results in transcription factors and alters gene expression |
|
|
|
Learn biosynthesis, storage and secretion of thyroid hormones |
Please |
|
|
|
Which form of thyroid hormones is active and inactive? |
Active; T3 Inactive; T4 |
|
|
|
What is the cavity inside follicular cells called? |
Lumen |
|
|
|
What is colloid? |
Colloid is the sticky fluid filling the thyroid follicular lumen. It contains Thyroglobulin (TGB) w/ attached to newly synthesised T3 and T4 for storge (iodine ions present) |
|
|
|
How are thyroid hormones synthesised? |
1) I- is actively up taken from blood into follicular cells via Na+/I- Symporters (both into the cell) . Then it diffuses into lumen by passive diffusion where it is oxidised (2I- ➡️ I2) 2) Thyroglobulin is synthesised by the follicular cell also and released into the lumen via exocytosis 3) Tyrosine molecules on the TGB undergo iodination to form MIT and DIT 4) MIT + DIT =T3 DIT + DIT = T4 5) colloid enters follicular cells via pinocytosis and merges with lysosomes. Digestive enzymes breakdown TGB leaving T3 and T4 |
|
|
|
What is MIT AND DIT |
Monoiodotyrosine Diioditryosine (tyrosine is the functional units of the TGB that the iodide binds to) |
|
|
|
Where is T4 broken down into T3? |
Liver and kidneys |
|
|
|
Where does TSH come into all this? |
Binds to TSH receptors on the follicular cell and causes endocytosis of droplets of colloid into the follicular cell where digestive enzymes in the lysosomes break down TGB and release T3 and T4 into the blood stream |
|
|
|
Describe the hypothalamic - pituitary - thyroid axis (negative feedback loop). How are levels of thyroid hormones in the blood increased? |
1) hypothalamus detects low circulating T3/T4/thyroid hormone
2) responds by releasing thyrotropin- releasing hormone (TRH) which stimulates the anterior pituitary gland to produce TSH 3) TSH stimulates thyroid gland to produce thyroid hormones and levels increase in blood |
|
|
|
How are levels of thyroid hormones decreased? |
TSH is an inhibitor for the hypothalamus producing TRH
Thyroid hormones are inhibitors for the anterior pituitary and hypothalamus |
|
|
|
What is hypothyroidism? |
TSH LEVELS ARE HIGH T3 / T4 LEVELS ARE LOW |
|
|
|
What is hyperthyroidism? |
TSH LEVELS ARE LOW T3 & T4 LEVELS ARE HIGH |
|
|
|
Effects of hyperthyroidism |
Increased basal metabolic rate Wight loss, good appetite Diarrohea Warm sweaty skin, heat intolerance Tachycardia |
|
|
|
Effects of hypothyroidism |
Decreased basal metabolic rate Weight gain, anorexia Dry skin Brady Constipation |
|
|
|
What does calcitonin do? |
Lowers release of calcium ions and phosphates by inhibiting bone resorption (opposite action of Parathyroid hormone) |
|
|
|
Name 3 sex steroids |
Testosterone Estrogen Progesterone |
|
|
|
What are these three sex hormones formed from? |
Cholesterol |
|
|
|
How is progesterone produced from cholesterol? |
Cholesterol to pregnenolone Pregnenolone to progesterone |
|
|
|
How is testosterone produced from cholesterol? |
Cholesterol to pregnenolone Pregnenolone to testosterone |
|
|
|
How is estrogen formed from cholesterol? |
Cholesterol to pregnenolone Pregnenolone to testosterone Testosterone to estrogen |
|
|
|
What enzyme converts testosterone to estrogen? |
Aromatase |
|
|
|
Where is testosterone produced? In men and in women (small amounts) |
Men: leydig cells Females: theca interna in ovaries |
|
|
|
When is the concentration of testosterone highest in the blood? What is this pattern called? |
In the morning Circadian rhythm |
|
|
|
What does testosterone do? |
Muscle growth Spermatogenesis Secondary male sexual characteristic |
|
|
|
What are the levels of testosterone and estrogen controlled by? |
LH & FSH |
|
|
|
What are the 3 types of estrogen? Which one is the main type? |
Estrone Estradiol - main Esteriol |
|
|
|
How is estrogen produced? In men too? |
Females :By granulosa cells of follicle Through conversion of testosterone via aromatization Placenta
Males: sertoli cells of testi |
|
|
|
What does estrogen do? |
Bone mass GnRH regulation Ovulation Cardiovascular Physiology Neuronal growth |
|
|
|
What is progesterone? |
A pregnancy hormone which initiates and maintains conditions for pregnancy |
|
|
|
What does progesterone do? |
Enhances endometrium secretion Inhibits uterine contractions Maintains pregnancy Increases body temperature Inhibits GnRH release |
|
|
|
Where is progesterone produced? Name 3 |
Corpus luteal cells Adrenal glands Placenta |
|
|
|
What is hypogonadism? |
Due to lack of estrogen and testosterone (hormones which help develop gonads) there is an underdevelopment of gonads |
|
|
|
Hypogonadism can be primary or secondary. When is it primary vs secondary? |
Defect at the level of gonad
Defect at pituitary or hypothalamus level causing reduced FSH/ LH levels or reduced GnRH secretion |
|
|
|
Where are the Parathyroid glands located? What do the Parathyroid glands consist of? |
Posterior of thyroid gland 4 small oval shaped glands |
|
|
|
What is the function of Parathyroid glands? |
They secrete Parathyroid hormone in response to low calcium serum level |
|
|
|
What cells are the Parathyroid glands made up of? |
Cheif cells Oxyphil cells |
|
|
|
What do the cheif cells secrete? |
Parathyroid hormones |
|
|
|
Which nerves supply the Parathyroid gland? |
Nerves derived from thyroid branches of the cervical ganglia |
|
|
|
Embryology of the Parathyroid gland? Superior and Inferior |
Superior Parathyroid glands originate from the 4th pharyngeal pouch Inferior Parathyroid glands a derived from the 3rd pharyngeal pouch |
|
|
|
What G protein does PTH use? |
Adenyl cyclase pathway |
|
|
|
How does the Parathyroid gland determine calcium levels? |
Receptors |
|
|
|
How is Parathyroid hormone activated? |
Pre prohormone to Pro hormone to Active hormone |
|
|
|
What does PTH do? Where does it do this? |
Activates 1 alpha hydroxylase in kidneys which converts CALCIDIOL into CALCITRIOL |
|
|
|
What is the active form of vitamin D? |
CALCITRIOL |
|
|
|
What does Vitamin D do? In the intestines? Kidneys? Bone? |
Maintains calcium serum levels in general:
Increases Ca2+ absorption in GI tract Increases bone resorption to release Ca2+ (vitamin D binds to the osteoblast which then release RANKL which causes Ca2+ reabsorption) Increases reabsorption of Ca2+ in kidneys |
|
|
|
What are the arteries that supply blood to the Parathyroid glands? |
Inferior thyroid arteries |
|
|
|
What are the veins that drain the Parathyroid gland? |
Parathyroid vein into thyroid venous plexus |
|
|
|
Where can you find VDR (Vitamin D receptor) and PTHR (Parathyroid hormone receptor)? Baso where does Vitamin D act? |
Intestines Kidneys Bone |
|
|
|
What else causes calcium serum levels to increase? |
Parathyroid horomes Binds to Parathyroid hormone receptors in kidneys and bone and increase calcium serum levels |
|
|
|
Describe the synthesis of Vitamin D |
7-Dehydrocholesterol Cholecalciferol Calcidiol CALCITRIOL |
|
|
|
How is 7-Dehydrocholesterol converted into Cholecalciferol? Where does this take place? |
UVB Skin |
|
|
|
How is Cholecalciferol converted into calcidiol? Where does this take place? |
Enzyme 25 hydroxylase Liver |
|
|
|
How is calcidiol converted into CALCITRIOL? Where does this happen? |
1 a-Hydroxylase enzyme Kidneys |
|
|
|
What activates 1 a-Hydroxylase? |
PTH activates it |
|
|
|
What is calcium used for? |
Neuronal excitability Muscle contraction Inc cardiac Blood clotting Cell devision / adhesion |
|
|
|
What is phosphate stored as? What is it used for? |
Stored as hydroxyapatite in bones - skeletal integrity ATP production |
|
|
|
What are the 3 hormones involved in calcium level management? |
Vitamin D Parathyroid Hormone Calcitonin |
|
|
|
What happens when ca2+ levels decrease? |
Increase in PTH Effects bone and kidneys to |
|
|
|
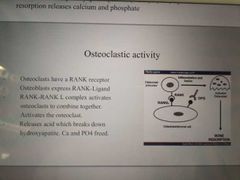
How does PTH and CALCITRIOL effect bone? |
Inhibits osteoblast Stimulate osteoclasts Bone is broken down releasing Ca2+ into the bloodstream |
|
|
|
How does PTH and Calcitriol effect the kidneys? |
PTH = an increase in PTH increases absorption of Ca2+ from kidneys and decreases phosphate reabsorption. Calcium serum levels increase but phosphate serum levels drop Calcitriol = an increase in Calcitriol increases absorption of Ca2+ and phosphate ion reabsorption from the kidneys |
|
|
|
What does Calcitriol do to the GI track? |
Increases number of calcium and phosphate channels in the GIT. So increases absorption of both ions |
|
|
|
What happens in response to increased Ca2+ levels? |
Parafollicular cells of the thyroid glands are stimulated by high conc of ca2+ and produce calcitonin. |
|
|
|
What is the effect of calcitonin on bone? |
Stimulates osteoblast Inhibits osteoclasts Calcium is removed from blood and used to build bone |
|
|
|
Overall effect of PTH on calcium and phosphate levels? |
Loss of phosphate from the kidneys is greater than phosphate absorbed from gut and bone - overall increase calcium and decreased phosphate |
|
|
|
Osteoblasts vs osteoclasts |
Osteoblasts - B - build bone Osteoclasts - C - crash bone |
|
|
|
What does this mean? |
|
Hydroxyapitate releases both Ca and PO4 |
|
|
What causes hypoparathyroidism? What things can cause this? |
Low PTH & low calcium serum levels
Surgical removal or auto immune disorders |
|
|
|
What causes pseudohypoparathyroidism? What things cause it? |
High PTH Target organ resistance to PTH - developmental disorder |
|
|
|
What are some clinical features of hypoparathyroidism? My Mum Can Never Tell Truth |
Muscle weakness Muscle cramps Chvosteks sign Nerve function Trousseau sign Tetany |
|
|
|
What is hyperparathyroidism? |
Increased secretion of PTH |
|
|
|
What are the two types of hyperparathyroidism? |
Primary - increased PTH due to a disorder to the gland (benign tumour) Secondary - compensatory oversecretion. Nothing is wrong with the gland but conditions like kidney failure and vit D deficiency decrease calcium levels which increases PTH |
|
|
|
Symptoms of hyperparathyroidism |
Often asymptomatic But can be ; Constipated Psychosis EVG changed - short QT interval |
|
|
|
What can be some complications of hyperparathyroidism? |
Osteoporosis Kidney stones Peptic ulcers Pancreatitis |
|
|
|
How is glucose transported into cells? |
Via 2 types of transporters: - sodium dependent glucose transporters (SDGTs) - facilitative glucose transporters (GLUT's) |
|
|
|
How do SGDTs work? Where are the present? |
These are sodium/ glucose co-transporters (secondary active transport). They uptake glucose from the intestines with sodium into epithelial cells |
|
|
|
What are GLUT's? |
Passive Glucose transporters via Facilitated diffusion |
|
|
|
How many GLUT's are there? |
5 |
|
|
|
Where is Glut 1 found? |
Brain Erythrocytes Placenta Fetal tissue |
|
|
|
What is special about Glut 1? |
Has a high affinity for glucose therefore uptake of glucose is constant |
|
|
|
Where is Glut 2 found? |
Tissues (liver, kidneys, intestine, pancreatic beta cells) |
|
|
|
What does insulin do to Glut 2? |
Increases up takes of glucose by Glut 2 but the liver itself does not need the insulin in order to uptake glucose |
|
|
|
Where is Glut 3 found? Why is Glut 3 special? |
Brain Allows preferential uptake of glucose in a hypoglycemic state |
|
|
|
Where is Glut 4 found? |
Muscle Adipose tissue (insulin stimulates a cascade reaction to store glucose) |
|
|
|
Where is Glut 5 found? |
Jejunum (part of small intestine) |
|
|
|
Describe the mechanism of insulin action in Glut 4 |
1) insulin binds to tyrosine kinase receptors 2) triggers protein kinase cascade 3) Glut 4 transporters travel to cell surface by exocytosis 4) glucose enters the cell |
|
|
|
What is glucose converted into in Adipose tissues? |
Fatty acids |
|
|
|
What is glucose converted into in the liver and skeletal muscle? |
Glycogen |
|
|
|
Anatomy of the Pancreas |
-Upper left quadrant -Posterior to stomach -Anterior to kidneys -Retroperitoneal except for tail which is intra peritoneal |
|
|
|
How many parts does the Pancreas have and what are they called? |
4 Head Neck Body Tail |
|
|
|
What are the functions of Pancreas? |
Digestion (exocrine) Hormone production (endocrine) |
|
|
|
What proportion of the Pancreas is endocrine function vs exocrine function? |
10% endocrine 90% exocrine |
|
|
|
What hormones do alpha cells release? What is the target organ? |
Glucagon Liver |
|
|
|
What hormones do beta cells release? |
Insulin |
|
|
|
What hormones do delta cells secrete? What is the action of this hormone? |
Somatostatin which Inhibits the secretion of insulin and glucagon (and GHRH) |
|
|
|
What do PPcells release? (diagram calls these F cells) what does this inhibit? |
Pancreatic polypeptide which Inhibits the secretion of Somatostatin |
|
|
|
Exocrine functions of the Pancreas? |
Secrete enzymes which neutralise and digest food in the intestines |
|
|
|
What can the exocrine portions of the Pancreas be divided into? |
Lobules |
|
|
|
What are lobules made up of? |
Acinar cells Ductal cells |
|
|
|
What do aciner cells do? |
Release digestive enzymes |
|
|
|
What do Ductal cells do? |
Secrete fluid and bicarbonate |
|
|
|
What 3 things are alpha cells stimulated by? |
Low blood glucose in fasting state
Sympathetic nervous system
Rise in blood amino acids |
|
|
|
What is the function of glucagon? |
Increase blood glucose levels Stimulate glycogenolysis Stimulates gluconeogenesis Inhibits glycogenesis |
|
|
|
What stimulates beta cells? |
High glucose in fed state Parasympathetic NS Gastric inhibitory polypeptide (GIP) and glucogon-like-peptide-1 |
|
|
|
What is the function of insulin? What does insulin suppress in the liver? |
Lowers blood glucose levels Increase uptake & storage of glucose, fatty acids, aa in liver & muscle tissue In liver suppresses gluconeogenesis |
|
|
|
How do beta cells work? |
1) glucose enters the cells via GLUT-2 2) glucose is converted into Glucose-6-phosphate via glucokinase 3)G6P stimulates glycolysis to produce ATP 4)ATP sensitive potassium channels close 5)potassium build up in the cell opens voltage gated calcium channels 6)increased ca2+ induces secretion of insulin |

|
|
|
What are the Incretins that also Stimulate insulin secretion after a carb rich meal? |
GIP GLP - 1 |
|
|
|
What are some causes of hypoglycemia? |
Excessive alcohol consumption Hormonal abnormalities Overdose of insulin |
|
|
|
Role of Adrenal glands in glucose regulation. What is released during fasting? |
Adrenaline is released during fasting
Cortisol is secreted in prolonged fasting (form of stress) |
|
|
|
What does Adrenaline do in a hypoglycemic state? |
Promotes glycogenolysis in liver and skeletal muscles |
|
|
|
What does cortisol do in a hypoglycemic state? |
Supports gluconeogenesis in the liver by mobilising aa from skeletal muscles |
|
|
|
What is type 1 diabetes? |
Insulin deficiency |
|
|
|
What is type 1 diabetes caused by? |
Autoimmune destruction of pancreatic beta cells At least 18 genes are involved + complex environmental interactions |
|
|
|
What age does type 1 diabetes develop? |
Any age but typically childhood |
|
|
|
What are the effects of having type 1 diabetes? |
Uncontrolled gluconeogenesis Use of alternative fuels Development of hyperglycaemia Ketoacidosis Eventual coma and death if untreated |
|
|
|
What is Ketoacidosis? |
Uncontrolled catabolism of lipids |
|
|
|
What is type 2 diabetes? |
Insulin resistance and insulin deficiency
Target tissues become unresponsive to insulin |
|
|
|
What happens when people develop. Type 2 diabetes? |
Target tissues are unresponsive to insulin. Pancreatic beta cells produce even more insulin to compensate so bg levels remain normal but eventually the cells function progressively declines and there's an insulin deficiency thus hyperglycemia |
|
|
|
What age does type 2 typically develop? |
Over 40 |
|
|
|
What is a major factor risk factor for type 2 diabetes? |
Obesity This is linked to the insulin resistance and beta cell dysfunction |
|
|
|
Describe the mechanism of insulin resistance |
Increased stress on cells since they're constantly metabolising incoming glucose Cells becomes overwhelmed with glucose and send signals to down regulates insulin receptors on its surface to stop glucose entering |
|
|
|
What is the neuroendocrine system? |
Nervous and endocrine systems work together |
|
|
|
What is the hypothalamus made up of? |
Groups of neurons called nuclei |
|
|
|
What is the name of the blood vessel network in the hypothalamus? |
Hypothalamo-hypophysial- portal system |
|
|
|
Where is the anterior pituitary derived from? |
Ectoderm of Rathke's pouch |
|
|
|
Where is the posterior pituitary derived from embryologically? |
Downward extension of neural ectoderm from the floor of the diencephalon |
|
|
|
What is the name of the bulb next to the pituitary gland but below hypothalamus? |
Optic chasm |
|
|
|
What is the name of the neck of the anterior pituitary? |
Pars tuberalis |
|
|
|
What is the name of the membrane in between the anterior and posterior pituitary? |
Pars intermedia |
|
|
|
What is the name of the body of the anterior pituitary? |
Pars distalis |
|
|
|
What is the neck of the posterior pituitary called? |
Infundibular stalk |
|
|
|
What is the body of the posterior pituitary called? |
Pars nervosa |
|
|
|
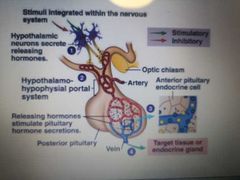
How does hormone action from the anterior pituitary work? |
1) hypothalamic neurons secrete releasing hormones 2) hypothalamo-hypophysial portal system 3) releasing hormones Stimulate pituitary hormone secretion 4) exit via vein to target tissue or endocrine gland
|
|
|
|
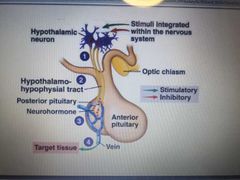
How does posterior pituitary hormone action work? |
1) hypothalamic neuron 2) hypothalamo-hypophysial tract 3) posterior pituitary 4) vein and into the blood stream |
|
|
|
What starts the GHRH-GH-IGF1 Axis? |
Stress and low blood glucose stimulates increased release of GHRH and decreases production of GHIH (inhibiting hormone)
GH produced then Inhibits the production of GHRH |
|
|
|
What mediated the effects of GH? |
IGF - 1 |
|
|
|
Where is IGF-1 produced? |
Liver in response to GH stimulation |
|
|
|
Main function of GH in children and adults? |
Children: linear growth Adults: protein synthesis Carbohydrate metabolism Lipolysis Calcium homeostasis |
|
|
|
Describe the CRH - ACTH - Adrenal axis |
Stress/ hypoglycemia Release of CRH Via hypothalamo-hypophysial portal system to anterior pituitary ACTH released Adrenal cortex releases cortisol |
|
|
|
What does cortisol inhibit? |
ACTH and CRH production |
|
|
|
What does cortisol do? |
Increases glucose production Increases protein breakdown Increases fat breakdown |
|
|
|
TRH-TSH- THYROID AXIS |
TRH from hypothalamus Causes TSH release from anterior Stimulates thyroid to make T3 & T4 T3 & T4 inhibit TSH & TRH release |
|
|
|
What action do T4 & T3 bring? |
-increased heart rate and Cardiac output -increased bone turnover and resorption -increased gut mobility -breaks down fats -increases catecholamines sensitivity in the sympathetic nervous system |
|
|
|
Prolactin axis? |
Anterior releases prolactin Hypothalamus releases dopamine to inhibit prolactin production |
|
|
|
Which nuclei is ADH produced in? |
Supraoptic nucleus |
|
|
|
Which nuclei is oxytocin produced in? |
Paraventricular nucleus |
|
|
|
What oxytocin do? |
-milk ejection (suckling is stimulus) -stimulates myoepithelial contractions (in uterus during childbirth and in mammary glands during lactaions) |
|
|
|
What does ADH do? |
-conserves body water -water deprivation increases osmolality of plasma which activates hypothalamic ossmoreceptors to stimulate ADH release |
|
|
|
What are some other functions of the hypothalamus? |
Thirst control Temperature Autonomic nervous system Appetite and hunger Sleep and circadian rhythm |
|
|
|
Which hormone can penetrates the plasma membrane? |
Estrogen |
|
|
|
G-protein coupled receptors are at the site of interaction for what? What are G proteins? |
Catecholamines (G-protein are proteins which bind signal molecules outside the cell, transduct the signal into the cell and cause a cellular response) |
|
|
|
Which hormone Inhibits release of growth hormone from the anterior pituitary? |
Somatostatin |
|
|
|
Leptin regulates food intake through interactions with what? |
The hypothalamus |
|
|
|
Where is calcium reabsorbed in the kidneys? |
60% PCT 15% thick ascending 10-15% DCT (this is where PTH and Calcitriol would act) |
|
|
|
What is acromegaly? |
When pituitary gland produces too much growth hormone during adulthood. This leads to swollen hands and feet, larger features, abnormal periods and erectile dysfunction. Tiredness/ sleep apnoe |
|
|
|
What is Addison's disease? |
Under production of cortisol and aldosterone due to autoimmune destruction of Adrenal gland. Can present at any age. Symptoms are: weight loss, dizzy spells, hyperpigmentation, frequent urination |
|
|
|
Which gland produces melatonin? |
Pineal gland Important in sleep cycle |
|
|
|
What is leptin? |
A hormone from fat that controls food intake |
|
|
|
What is conn's syndrome/ primary hyleraldosteronism? |
Too much aldosterone production Causes hypertension and metabolic alkalosis |
|
|
|
What is cushing's syndrome? |
Increase in ACTH release leading to the production of excess cortisol |
|
|
|
What is pgeochromocytoma (PCC)? |
A tumour in the Adrenal medulla of the Adrenal glands. Causes the Adrenal glands to make too much noradrenaline and adrenaline |
|
|
|
What is white adipose tissue? What is the function? |
-A single large membrane enclosed lipid droplet and few mitochondria -modest blood supply -function is lipid storage and hence insulation |
|
|
|
What does white adipose tissue secrete? |
Leptin Asprosin (during fasting to cause rapid release of glucose from the liver) |
|
|
|
What is brown adipose tissue? |
-Contains many small lipid droplets and lots of mitochondria (giving brown colour) -rich in blood supply |
|
|
|
What is the function of brown adipose tissue? |
Thermogenesis (process of heat production in body) |
|
|
|
What hormones are responsible for appetite regulation? |
Leptin Ghrelin Insulin |
|
|
|
When is leptin secreted? What does leptin inhibit? |
Released from adipose tissues. More fat = more leptin released
Decreases appetite and suppresses hunger
Leptin Inhibits insulin production and secretion. In contrast, insulin stimulates leptin secretion from adipose tissues |
|
|
|
What does ghrelin do? |
Released by G cells in response to empty stomach (walls not Stretched)
Acts on GHS-R on Arcuate nuclei
Increases appetite, decreases thermogenesis and increases insulin production (baso opposite to white and brown adipose tissue action) |
|
|
|
What protein converts cholesterol into pregnenolone? |
Steroidogenic Acute Regulatory Protein (StAR) |
|
|
|
What are the cells of anterior pituitary and what are they responsible for? |
Somatotrophs - GH Thyrotrophs - TSH Ginadotrophs - FSH and LH Lactotrophs - Prolactin Corticotrophs - ACTH and MSH |
|
|
|
GH can act in two ways: |
Direct Indirect |
|
|
|
How does GH act directly? |
GH binds to receptors on adipose tissues and target cells. Causes them to breakdown triglycerides and suppress their ability to take up lipids.
GH is released when theres hypoglycaemia, low fatty acids, high aa, in deep sleep, in the presence of the rest of the anterior pituitary hormones. GHRH acts in somatotrophs to produce GH |
|
|
|
What is the indirect action of GH? |
Mediated by insulin-like growth factor (IGF-1) a hormone that is released by the liver in response to GH
IGF-1 stimulates osteoblasts at the epiphyseal plate, increasing uptake of aa (for protein synthesis) and increasing blood glucose |
|
|
|
What Inhibits GH? |
GHIH/ SOMATOSTATIN is released in response to GHRH and Inhibits GHRH release |
|
|
|
What is gigantism? |
Caused by adenoma, a tumour of the pituitary gland. Excessive growth hormone in childhood |
|

