![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
403 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
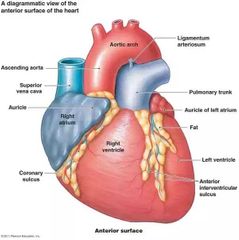
What is an auricle? |
Small area (shaped like an 'ear' present in the anterior side of each atria |
|
|
|
What does the Auricle do? |
Slightly increases the capacity of the atria (so greater potential blood volume) |
|
|
|
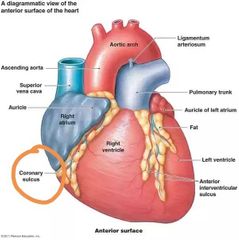
What's a sulci? |
A series of grooves in the surface of the heart that contain coronary blood vessels and fat |
|
|
|
What does each sulcus mark? |
The external boundary of each chamber of the heart |
|
|
|
What is the deep coronary sulcus mark? |
The external boundary between the superior atria and Inferior ventricles |
|
|
|
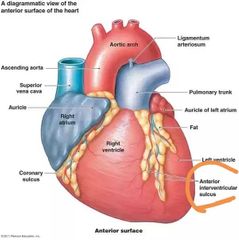
What does the anterior interventricular sulcus mark? |
Boundary between the left and right ventricles (shown as shallow grooves on the anterior surface) |
|
|
|
What is the posterior interventricular sulcus? |
The posterior interventricular artery of the heart is a branch of the right coronary artery |
|
|
|
What is a septa? |
The septa of the heart are the dividing walls present which seperate the four Chambers of the heart |
|
|
|
What are the three types of septa in the heart? |
Interarterial Interventricular Atrioventricular |
|
|
|
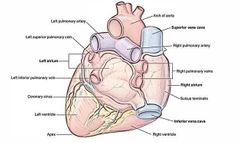
What are the 4 Chambers of the heart? |
Right atrium Right ventricle Left atrium Left ventricle |
|
|
|
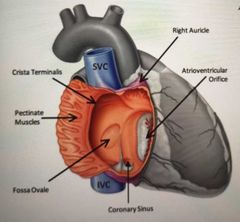
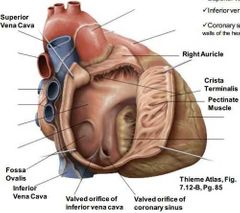
Where does the right atrium receive deoxygenated blood from? |
Superior Vena Cava Inferior Vena Cava Coronary sinus |
|
|
|
Why is the inside of the posterior wall of the atrium smooth and the anterior wall rough? |
Because of pectinate muscles |
|
|
|
What is crista terminalis? Where does it span from and to? |
The ridge on the inside of the right atrial wall between the atria and right Auricle, spanning from SVC to IVC |
|
|
|
What is Fossa ovale? |
An oval depression in the interarterial septum which is the remnant of the foramen ovale (which was an opening for the foetal heart in order to bypass the lungs) |
|
|
|
What is the valve between the right atrium and right ventricle called? |
Tricuspid valve |
|
|
|
What does the blood flow through to get from the right ventricle to the Pulmonary trunk? |
Conus arteriosus (smooth walled) / infundibulum |

|
|
|
What valve closes behind the blood entering the Pulmonary trunk? |
Pulmonary valve |
|
|
|
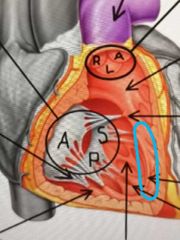
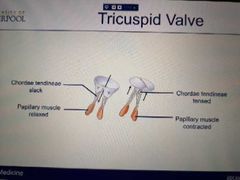
What is the tricuspid valve made up of? |
Fold of the endocardium & Connective tissues |
|
|
|
How many cusps does the tricuspid valve have? What are the named? |
Anterior Superior/ Septal Inferior |

|
|
|
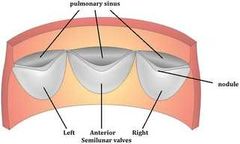
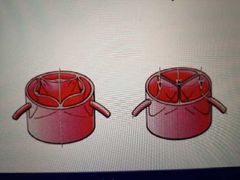
What types of cusps does the Pulmonary valve have? What are their names? |
Semilunar: -anterior -left -right |

|
|
|
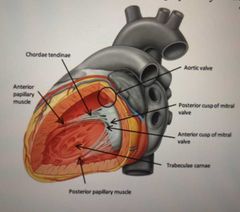
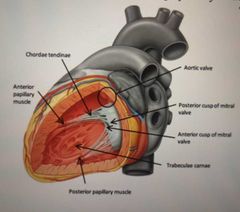
What is the series of ridges inside of right and left ventricle formed by raised bundles of Cardiac muscles called? |
Trabeculae carnae |

|
|
|
What are the tendons that attach the cusps of the tricuspid valve to the papillary muscles called? |
Chordae tendineae |

|
|
|
What is the function of the papillary muscles? |
When the ventricles contract, papillary muscles contract, preventing the cusps from turning inside out into the atrium as interventricular pressure rises |
|
|
|
What are the three types of papillary muscles? |
Anterior (largest) Posterior Septal Named based on anatomical position of the papillary muscles |

|
|
|
What is the septomarginal trabecula? |
Bridge between the interventricular septum and base of the anterior papillary muscle |
|
|
|
What is the function of the septomarginal trabecula? |
Carries a portion of the Cardiac conduction system to anterior wall of right ventricle |
|
|
|
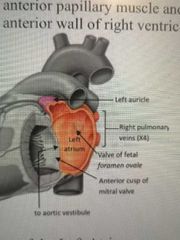
Which chamber of the heart forms most of the base of the heart? |
Left atrium |
|
|
|
Where does blood enter the left atrium from? |
Through 4 Pulmonary veins (2 from left lungs, and 2 from right) |
|
|
|
Are the walls of the left atrium smooth? Anterior and posterior |
Yes, both are smooth |
|
|
|
What is not present between the left atrium and the left Auricle in the anterior surface of the heart? |
No crista terminalis |
|
|
|
What is the depression in the interarterial septum? |
The valve of the foramen ovale |
|
|
|
Blood moves from the left atrium to left ventricle via which valve? |
Mitral valve |
|
|
|
What are the cusps of the mitral valve? |
Anterior Posterior |
|
|
|
What are the cusps attached to the ant/post papillary muscles by? |
Chordae tendinae |
|
|
|
Does the left ventricle have trabeculae carnae present? |
Yes |
|
|
|
What is the name of the valve between left ventricle and aorta? |
Aortic valve |
|
|
|
What are the 3 semilunar cusps of the aortic valve? |
Right Posterior Left |
|
|
|
What happens once blood passes through the aortic valve? |
The blood recoils in the aortic vestibule, filling up the aortic sinuses formed by the cusps and the blood in forced into the coronary arteries |
|
|

Label the Cardiac skeleton: |
1. Fibrous ring of Pulmonary valve 2. Fibrous ring of aortic valve 3. AV bundle 4. Right AV ring 5. Left AV ring |
|
|
|
What is the Cardiac skeleton |
A collection of fibrous tissue in the form of 4 rings which interconnect in a plane between atria and ventricles. The skeleton seperates muscular Wall of atria from ventricles and acts to electrically isolate the ventricles |
|
|
|
What is the name of the right and left fibrous rings of the heart around the AV and arterial orifices? |
Anuli fibrosi cordis |
|
|
|
What is the name of the right and left fibrous rings? |
Right- anulus fibrosus dexter cordis Left- anulus fibrosis sinister cordis |
|
|
|
What is Cardiac muscle also known as? |
Myocardium |
|
|
|
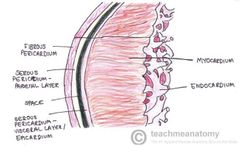
What is the internal lining of the heart consist of? |
Endocardium |
|
|
|
What cells is endocardium made up of? |
Endothelial cells |
|
|
|
What cells is myocardium made up of? |
Myocytes (specialised cells) |
|
|
|
What is epicardium made up of? |
Thin layer of mesothelial cells (slippery) and connective tissue |
|
|
|
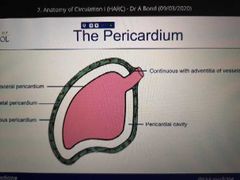
What is the pericardium? |
A fibrous sac that encloses the heart |
|
|
|
What is the function of the pericardium? |
-resist excessive movements of the heart as a whole -lubricates heart movement -prevents overfilling of heart |
|
|
|
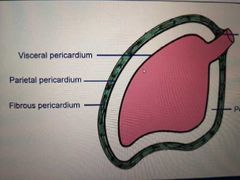
What are the 2 layers of the pericardium? |
Fibrous (outermost) Serous (inner) |
|
|
|
What is the serious layer spilt into? |
Parietal pericardium (outer) Visceral pericardium (inner) |
Note the continous black line |
|
|
How has the fibrous pericardium formed? |
Strong fibrous layer (acc just the external layer of the blood vessels that gave grown out around the heart forming the fibrous pericardium) |
|
|
|
What is the fibrous pericardium attached to? |
Diaphragm And Sternum |
|
|
|
What ligament attach the fibrous pericardium to the sternum? |
Sternopericardial |
|
|
|
What attaches the diaphragm to the fibrous pericardium? |
Pericardiophrenic ligament |
|
|
|
How does the fibrous pericardium interact with great blood vessels that pass through it? |
It fuses with their outer coats |
|
|
|
What does the parietal layer of the serous pericardium line? |
Fibrous pericardium |
|
|
|
What is the visceral layer of the serous pericardium also known as? |
Epicardium |
|
|
|
What is the cavity in between the parietal and visceral layer called? What does it contain? |
Pericardial cavity Pericardial fluid |
|
|
|
What is pericardial effusion? |
Pericardial effusion ("fluid around the heart") is an abnormal accumulation of fluid in the pericardial cavity. This causes the heart to become compressed and ineffective |
|
|
|
What causes pericardial effusion? |
Passage of fluid from capillaries to the pericardial cavity |
|
|
|
What is pericarditis? |
The inflammation of the pericardium usually causing sharp chest pain (commonly relieved by sitting forward) |
|
|
|
What does pericarditis do? How can it be clinically detected? |
Makes the serous pericardium rough. Creates the clinical sign of pericardial friction rub (which sounds like rustle of silk on auscultation over the left sternal border and upper ribs) |
|
|
|
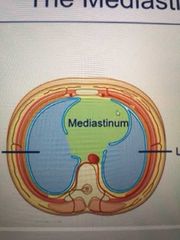
Where is the mediastinum? |
A space in the throax. It's the space between the right and left throacic cavity in which the right and left lungs sit. |
|
|
|
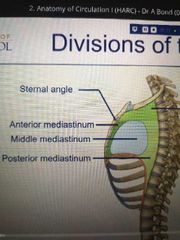
What is the mediastinum split into? |
Superior mediastinum (space above the sternal angle) Inferior mediastinum (space below the sternal angle) |
|
|
|
What is the inferior mediastinum split into? |
Anterior (front) Middle Posterior (back) |
|
|
|
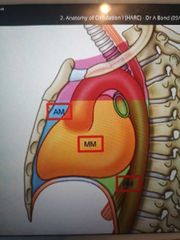
What is found in the anterior mediastinum? |
Thymus |
|
|
|
What is found in the middle mediastinum? |
Heart Pericardium |
|
|
|
What is found in the posterior mediastinum? |
Great vessels Oesophagus |
|
|
|
The pericardium is a serous membrane. What does this mean? |
It secretes fluid to lubricate the heart. Resist friction. |
|
|
|
How do the tricuspid and mitral valves stop back flow? |
Papillary muscle is relaxed so the chordae tendineae is slack. Allows blood to flow into the right ventricle. Before the contraction of the ventricle occurs, the papillary muscles contract and tense the chordae tendineae. The valves snap shut and stop backflow |
|
|
|
How do Pulmonary and aortic valves stop backflow? |
Blood flows through the space in the middle of the valve. When it tries to backflow, it ends up filling the semi-lunar pockets instead which shuts the valve. |
|
|
|
What is syncytium? |
A single giant multi nucleated cell. People argue electrically the heart is a syncytium |
|
|
|
Cardiac myocytes are joined to one another by what? |
An intercalated disc |
|
|
|
What is present in an intercalated disc? What does this crucially allow? |
Lots of gap junctions : these allow the flow of ions between cardiac myocytes. So if one cell depolarises and contracts, the whole heart will depolarise and contract. |
|
|
|
Compare Cardiac muscle to skeletal |
Cardiac muscles are: mononuclear shorter no stem cells present (thus cannot regenerate after damage) |
|
|
|
Cardiac vs smooth muscles |
-Smooth muscle isn't striated -Smooth muscles don't have gap junctions and intercalated discs |

|
|
|
Why is smooth muscles not striated? |
No actin and myosin |
|
|
|
What sit in the groves/sulcus of the heart? |
Blood vessels |
|
|
|
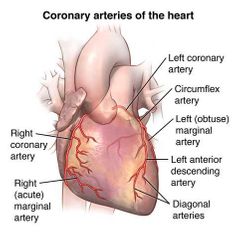
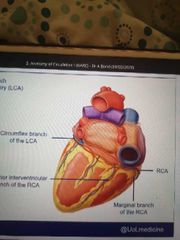
Where do the two coronary arteries arise from? |
Aortic sinuses of the ascending aorta |
|
|
|
In which connective tissue of the heart are the coronary arteries distributed? |
Epicardial connective tissue |
|
|
|
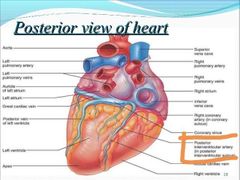
Right coronary artery: origin and pathway |
Aorta - Comes off aorta and sits in the coronary sulcus. Travels on the outer edge of the right Auricle and then continues posteriorly |
|
|
|
What branches may come off the right coronory artery |
Right Marginal branch (anterior branch) Posterior interventricular branch (branch on the posterior side) |
|
|
|
Left coronary artery: origin & pathway |
Arises from aorta and passes behind the pulmonary trunk and infront of left auricle. Here the LCA branches into the circumflex branch (which remains in the coronary sulcus and travels posteriorly) and the anterior interventricular branch which lays vertically below the left Auricle. |
|
|
|
What are the branches the come of the LCA? |
Circumflex branch Anterior interventricular branch |
|
|
|
Posterior view of the heart: |
|
|
|
|
What do the coronary arteries supply? |
The heart itself. The first thing the heart supplies is itself. |
|
|
|
What does the RCA supply? |
Right atrium Right ventricle (most) Left ventricle (diaphragmatic part) Interventricular septum SA node |
|
|
|
What does the LCA supply? |
Left atrium Left ventricle (most) Right ventricle (partially) Interventricular septum SA node AV node and bundle |
|
|
|
How much of the interventricular septum is supplied by the RCA vs LCA? |
RCA: Posterior 1/3 LCA: Anterior 2/3 |
|
|
|
What percentage of the SA node is supplied by the RCA vs LCA? |
RCA: 60% LCA: 40% |
|
|
|
What does the coronary sinus receive? |
Venous blood |
|
|
|
Where does the coronary sinus receive venous blood from? |
Great/middle/small/posterior/anterior cardiac veins |

|
|
|
Where does the mediastinum begin and end? |
Root of neck to diaphragm ↕️ Sternum to vertebral column ↔️ |
|
|
|
What is perfusion? |
The circulation of blood within an organ or tissue to meet the cells needs for oxygen, nutrients, and waste removal |
|
|
|
What are capillary walls (single cell thick) usually permeable to? |
O2 CO2 H2O Glucose Amino acids Fatty acids Vitamins Hormones |
|
|
|
What are capillary walls impermeable to? |
Proteins Blood cells |
|
|
|
What are some mechanisms of exchange in the blood vessels? |
Simple diffusion Pressure filtration |
|
|
|
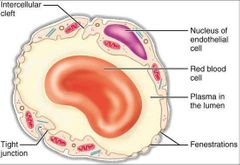
What are two routes of cross-wall movement? |
Intercellular cleft Fenestrations |
|
|
|
What are intercellular clefts? |
An intercellular cleft is a channel between two cells through which molecules may travel and gap junctions and tight junctions may be present. |
|
|
|
What are fenestrations? |
Small pores that go through endothelial cell to allow movement of molecules. They're necessary for free movement of substances |
|
|
|
Where are fenestrations common vs rare? |
Common in the liver Rare in the brain (so unwanted substances don't cross blood-brain barrier) |
|
|
|
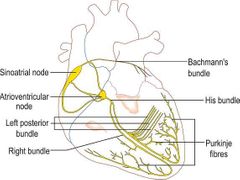
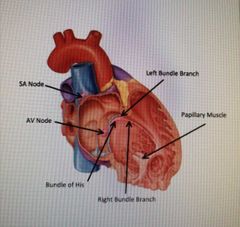
Briefly explain the conduction pathway of the heart. Which parts of the heart does it require? |
1. SA node creates action potential. This excites RA and LA and causes them to contract. 2. The impulse travels to AV node 3. Here it's travels through to the bundle of His 4. Then down the bundle branches 5. The bundle brunches terminate in purkinje fibres |
|
|
|
How does the impulses from SA node travel to the LA? |
They travel through the Bachmann's bundle and excited the LA |
|
|
|
What do the impulses travel through to get from the SA node to the AV node? |
Inter-node pathways in the right atrium |
|
|
|
What are bundle branches? |
Fibres specialised for rapid transmission of electrical impulses |
|
|
|
Where are bundle branches found? |
On either side of the interventricular spetum (right and left bundle branch) |
|
|
|
What does the RBB depolarise? |
Right ventricle |
|
|
|
What does the LBB depolarise? |
Left ventricle Interventricular septum |
|
|
|
Where are purkinje fibres found? |
Millions of small fibres projecting through the myocardium |
|
|
|
What prevents the backflow of blood through the AV valves? |
Impulses from the His-purkinje system travel in such a way that the papillary muscle contraction precedes that of the ventricles |
|
|
|
What two main forces drive ions across a cell membrane? |
Chemical potential Electrical potential |
|
|
|
What is chemical potential caused by? |
Caused by chemicals moving down their concentration gradient from an area of high concentration to an area of low concentration |
|
|
|
The difference in electrical potential (voltage) between the inside and outside of the cell is known as what? |
Transmembrane potential |
|
|
|
What happens to the transmembrane potential when there is a net movement if +ve ions into the cell? |
Transmembrane potential becomes more +ve and vice versa |
|
|
|
What are some properties of Cardiac ion channels? |
Selectively permeable to specific ions Voltage sensitive gating (only open at specific voltages) Time dependent (will only open for a fraction of a sec, then close and won't open until back to resting level TMP). |
|
|
|
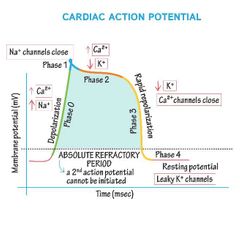
What are the 4 stages of a cardiomyocyte action potential? |
Phase 4- Resting phase Phase 0- Depolarisation Phase 1- Early repolarisation Phase 2- Plateau phase Phase 3- Repolarisation |
|
|
|
What is the resting potential of a cardiomyocyte and how is this maintained? |
-90V Na+/K+ pump is active (3Na+ out of the cell/ 2 K+ into the cell) Na+ and Ca2+ channels are closed Leaky K+ channels are open (NOT VOLTAGE GATED) |
|
|
|
Describe Depolarisation. At what voltage do Na+ ions open? |
1. Action potential from SA node/ neighbouring cardiomyocyte causes fast Na+ channels to open 2. Some Na+ enter the cell, raising the TMP 3. At -70mV threshold, lots more Na+ channels open causing influx of Na+ 4. TMP depolarises to over 0mV 5. Na+ channels close |
|
|
|
What is the period in which the TMP becomes positive called? |
Overshoot period |
|
|
|
What opens during Depolarisation when the TMP is around - 40mV? |
L-type Ca2+ channels, beginning the steady influx of Ca2+ into the cell down the concentration gradient |
|
|
|
Describe phase 1 -Early repolarisation |
TMP is slightly positive. Some K+ channels open and K+ leave out of the cell causing the TMP to be around 0mV |
|
|
|
Describe the phase 2 -Plateau phase |
-L-type Ca2+ channels still open and steady influx of Ca2+ into the cell continues -K+ continues to leave (via K+ leaky channels NOT VOLTAGE GATED) -this ion exchange is balanced maintain TMP at 0mV |
|
|
|
Describe phase 3 - Repolarisation |
-Ca2+ channels are inactivated -K+ VOLTAGE GATED channels open up and K+ continues to leave bringing TMP back to resting point - At -90V voltage gated K+ shut |
|
|
|
Is the refractory period of a skeletal muscle or Cardiac muscle longer? |
Cardiac |
|
|
|
Why do cardiac muscles have a longer refractory period? |
To prevent tetanus. Ensuring each contraction is followed by a big enough time to allow the heart chamber to refill before the next contraction |
|
|
|
What is a tetanic contraction? |
A sustained muscle contraction evoked when the motor nerve that innervated a skeletal muscle emits action potential at a very high rate |
|
|
|
What is excitation-contraction coupling? |
The mechanism by which an action potential causes a contraction |
|
|
|
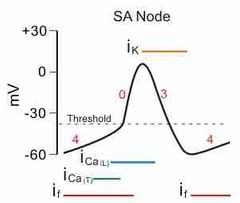
What are the properties of Cardiac pacemaker cells in the SA node? |
-Automaticity :don't require external stimulation for action potentials. Self-initiate depolarisation in a rhythmic pattern -Unstable membrane potential -No rapid Depolarisation stage |
|
|
|
Why do pacemaker cells not have a rapid depolarisation stage? |
Pacemaker cells have fewer Na+/K+ pumps than other cardiomyocyte so TMP is never lower than - 60mV. As fast Na+ channels need a TMP of - 90 mV to reconfigure into an active state, they are permanently inactivated in pacemaker cells so there's no rapid depolarisation phase |
|
|
|
What is the funny current/ pacemaker current? |
Spontaneous flow of ions mainly through slow Na+ channels slowly depolarises TMP above - 60mV |
|
|
|
Up to what voltage is the funny current active? |
TMPs of less than - 55 mV |
|
|
|
What happens at TMP - 55 mV? |
T-type Ca2+ channels open and continue slow depolarisation (Ca2+ move into the cell) |
|
|
|
What happens at - 40 mV? |
The threshold potential for pacemaker cells is reached. L-type Ca2+ channels open and depolarize cell to 0 mV, then overshoot to +40mV. NOTE THIS: the depolarisation is caused by a Ca2+ influx NOT Na+ |
|
|
|
What happens to repolarise the pacemaker cell? |
K+ channels open and counteract the L-type Ca2+ channels for a brief Plateau phase. Ca2+ channels close and then the TMP is returned back to - 60 mV because K+ channels remain open. |

|
|
|
What can increase heart rate and decrease heart rate? |
Sympathetic tone decreases time to reach threshold thus increases heart rate. (Increases Na+ influx)
Parasympathetic tone increases time to reach threshold thus decreases heart rate. (increases K+ efflux) |
|
|
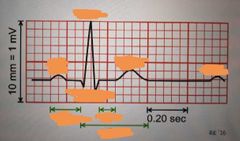
Label this ECG |
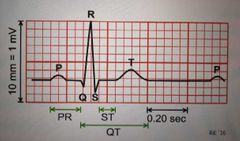
|
|
|
|
What does the P wave symbolise? |
Depolarisation of atria in response to SA node triggering |
|
|
|
What does the PR interval symbolise? |
Delay of AV node to allow filling of ventricles |
|
|
|
What does the QRS complex symbolise? |
Depolarisation of ventricles - triggering the main pumping contractions |
|
|
|
What does the ST segment symbolise? |
Beginning of ventricle repolarisation, should be flat |
|
|
|
What does the T wave symbolise? |
Ventricular repolarisation |
|
|
|
What is blood pressure? |
Measurement of the force against the walls of the arteries as the heart pumps blood throughout the body measured in millimetres of mercury (mmHg) |
|
|
|
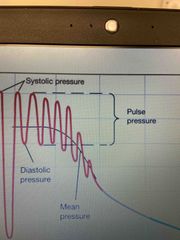
What is systolic pressure? |
Maximum arterial pressure during contraction of the ventricle of the heart |
|
|
|
What is diastolic pressure? |
The force exerted by blood in arterial walls during ventricular relaxation. The lowest pressure can be measured in the large arteries |
|
|
|
What is pulse pressure? |
Pulse pressure is the difference between systolic and diastolic blood pressure. So literally systolic - diastolic. Thus average is 120/80 |
|
|
|
What is the mean arterial pressure determined by? (MAP) |
Cardiac output (CO) Systemic vascular resistance (SVR) Central venous pressure (CVP)
|
|
|
|
What formula can be used to determine MAP? Mean arterial pressure |
(CO x SVR) + CVP Or Diastolic - 1/3 Pulse Pressure |
|
|
|
What is CVP usually taken as in order to measure MAP? |
0 mmHg |
|
|
|
What bp is hypotension? |
90/60 and below |
|
|
|
What is the normal bp range? |
90/60 to 120/80 |
|
|
|
What is the range for pre-hypertension? |
120/80 to 140/90 |
|
|
|
Bp above what is considered hypertension? |
140/90 and above |
|
|
|
What centre in the brain regulates blood pressure (stroke volume) and heart rate? |
Cardiovascular centre |
|
|
|
Where is the cardiovascular centre found? |
Medulla oblongata |
|
|
|
How does the cardiovascular centre decrease heart rate? -via which nerve -sympathetic or parasympathetic |
Via vagus nerve (parasympathetic nervous system) |
|
|
|
How does the cardiovascular centre increase heart rate? -via which nerve -sympathetic or parasympathetic |
Via cardiac accelerator nerves Sympathetic nervous system |
|
|
|
How does the cardiovascular centre cause vasoconstriction of blood vessels? -via which nerves -parasympathetic or sympathetic |
-vasomotor nerves -sympathetic |
|
|
|
Where are sensory receptors responsible for monitoring the chemical composition of blood found? |
Carotid sinus Arch of aorta |
|
|
|
Where are chemoreceptors responsible for maintaining arterial blood gasses found? |
PNS: Carotid sinus Arch of aorta CNS: Brain |
|
|
|
What do these sensory receptors detect in blood? |
Decrease in O2 (hypoxia) Increase in H+ (acidosis) Increase in CO2 (hypercapnia) |
|
|
|
What happens during a chemical reflex in response to the impulses sent by sensory receptors? |
Cardiac centre sends sympathetic impulses to cause systemic vasoconstriction -increasing BP |
|
|
|
What receptors normally (not chemical reflex) detect low BP? How? |
Baroreceptors These receptors stretch less with lower Bp thus sending slower rate of impulses to CV centre |
|
|
|
Which nerve are impulses from the carotid sinus sent? |
Glossopharyngeal nerve |
|
|
|
Which nerve are impulses from the aortic sinus sent? |
Vagus nerve |
|
|
|
What does the CV centre do when bp is high? |
Decreases/ Inhibits sympathetic stimulation of heart via cardiac accelerator nerves And Increases the parasympathetic stimulation via the vagus nerve Thus Bp lowers
|
|
|
|
What does the CV centre do when bp is too low? |
Decrease in parasympathetic stimulation via vagus nerve And Increase in sympathetic stimulation of the heart via cardiac accelerator nerves Thus bp increases |
|
|
|
What is systole and dystole? |
Systole - Contraction (normally of the ventricles) Diastole - Relaxation (normally of ventricles) |
|
|
|
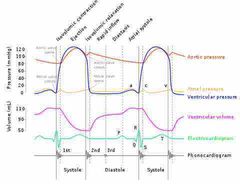
What are the 5 stages of the cardiac cycle? |
Late diastole Atrial systole Isovolumic ventricular contraction Ventricular ejection Isovolumic ventricular relaxation |
|
|
|
What happens in the late diastole? |
Both sets of chambers are relaxed and the ventricles fill passively |
|
|
|
What happens during atrial systole? |
Depolarisation of the SA node causes atrial depolarisation (p wave). Atria contracts, increasing the pressure within and causing the AV valves to open and blood to move down the pressure gradient into the ventricles. (This is acc a very small amount of blood that is pushed into the ventricles since they’re already pretty full passively) |
|
|
|
What happens during the isovolumic ventricular contraction? |
First phase of ventricular contraction during which the pressure inside the ventricles increases enough to close the AV valves but not enough to push open the semilunar valves |
|
|
|
What is the ventricular ejection? |
Ventricular pressures keeps rising with depolarisation and ventricular contraction, to the point where the pressure is greater inside the ventricles than the arteries. The semilunar valves open and the blood is ejected into the arteries |
|
|
|
What is the isovolumic ventricular relaxation? |
As ventricles relax, the pressure in the ventricles falls, blood flows back into cups of semilunar valves and snaps them close |
|
|
Do you understand this: |
Back (Definition) |
|
|
|
What is jugular venous pulse/ pressure? |
The jugular venous pressure (JVP, sometimes referred to as jugular venous pulse) is the indirectly observed pressure over the venous system via visualization of the right internal jugular vein |
|
|
|
Why is the internal jugular vein used for measuring jugular venous pressure? |
Because it doesn’t have valves |
|
|
|
Why is the right internal jugular vein used instead of the left internal jugular vein? |
As the right one travels almost directly above the superior vena cava and drains into the right atrium. Thus is an accurate representation of central venous pressure whereas the left drains in the superior vena cava via the left innominate vein |
|
|
|
Understand this: |
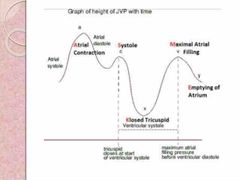
Back (Definition) |
|
|
|
What does perfusion of tissues mean? |
The flow of blood through blood vessels supplying oxygen to tissues |
|
|
|
What is Dalton’s law of partial pressure? |
The total pressure exerted by a mixture of gases is the sum of the pressures exerted independently by each has (it’s partial pressure) in the mixture |
|
|
|
Why are erythrocytes anucleate cells? |
To make more room for oxygen |
|
|
|
How many Haem (iron) molecules thus haemoglobin in one red blood cell? |
4 |
|
|
|
How many molecules of O2 Can one Hb molecule carry? |
4 |
|
|
|
How many Hb in each erythrocyte? |
270 Million |
|
|
|
What are some properties of alveoli? |
-Large SA / good blood supply / think exchange surface - low surface tension |
|
|
|
How do alveoli have low surface tension? What cells produce the fluid? |
Type 2 Alveolar cells produce pulmonary surfactant which have both hydrophobic and hydrophilic regions. This reduces Surface tension |
|
|
|
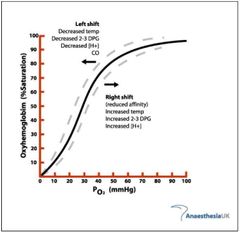
Explain the oxyhaemoglobin dissociation curve |
At low concentrations of oxygen, Hb has a low affinity for oxygen as the four polypeptide chains are tightly packed together.
Once the first oxygen molecule is loaded, Hb structure changes to allow more oxygen to bind easier |
|
|
|
When does the oxyhaemoglobin dissociation curve shift right? Hoe does temperature affect this? |
Decrease in pH Increase in CO2 Increase in temperature Increase in 2,3 bi/ Di sphosphoglyceric acid |
|
|
|
When does the oxyhaemoglobin dissociation curve shift left? (A left shift indicates increased oxygen affinity of haemoglobin allowing less oxygen to be available to the tissues.) |
Increase in PH Decrease in CO2 Decrease in Temp Decrease in 2,3 bi/ Di sphosphoglyceric acid |
|
|
|
Anatomy of the conducting system. Where is the SA node found? |
Superior to the crista terminalis |
|
|
|
Anatomy of the conducting system: where is the AV node found? |
Near the opening of the coronary sinus within the AV septum |
|
|
|
Where is the bundle of His anatomically found? |
Continous with the AV node and passes through the AV septum - then splits into the right and left bundle branch |
|
|
|
Anatomy of the right bundle branch |
Continues to the apex of the RV, entering the septomarginal trabecula, reeaching the base of the papillary muscle and forms the purkinje fibres |
|
|
|
Anatomy of the left bundle branch |
Passes to left side if the IV spetum, descending to the apex of LV and ends in purkinje fibres |
|
|
Fill in the labels: |
|
|
|
|
What is ventricular fibrillation? |
When ventricles contract rapidly and in an unsynchronised way, pumping little or no blood |
|
|
|
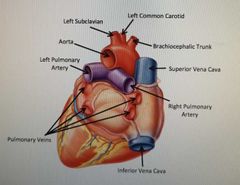
What are the great vessels of the heart and do they carry oxygenated or deoxygenated blood? |
|
|
|
|
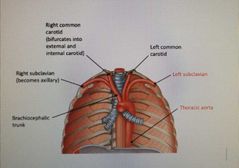
Posteriorly from right to left, order the three arteries coming off the aortic arch |
Left subclavian Left common carotid Brachiocephalic trunk |
|
|
|
What does the Brachiocephalic trunk bifurcate into? |
Right subclavian Right common carotid |
|
|
|
What does the right common carotid go on to split into? |
External and internal carotid |
|
|
|
What does the right subclavian artery go on to become? |
Axillary |
|
|
|
|
|
|
|
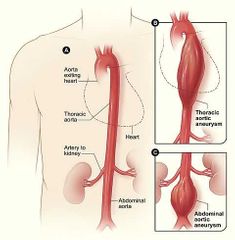
Relationship between Thoracic and abdominal aorta? |
|
|
|
|
At what level does the abdominal aorta bifurcate? |
L4 |
|
|
|
What does the abdominal aorta bifurcate into? |
Right common iliac Left common iliac |
|
|
|
The right/ left common iliac artery split into two. What is the internal of the two split up arteries called? |
Right / left internal iliac (these enter the pelvis) |
|
|
|
The remaining artery is called what? |
External iliac |
|
|
|
What does the external iliac supply? |
Blood to the lower limb |
|
|
Think about the venous drainage and the corresponding arterial system. Fill in the labels: |
|
|
|
|
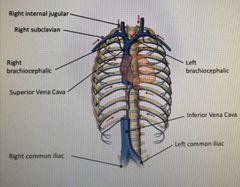
What does the superior Vena Cava split into? |
Right and left Brachiocephalic veins |
|
|
|
What does the right/left Brachiocephalic vein split into? |
Right/left subclavian vein (lateral) and Right/ left internal jugular (Medial) |
|
|
|
What are the 6 pulse point in the body? |
Neck Wrist Groin Posterior to the knee Near the ankle joint Foot |
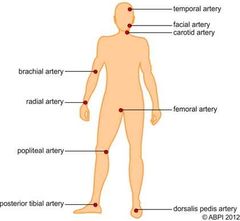
|
|
|
Neck pulse point is from which artery? |
Carotid artery |
|
|
|
Wrist pulse point is from which artery? |
Radial artery |
|
|
|
Groin pulse point is from which artery? |
Femoral artery |
|
|
|
The pulse point posterior to the knee is from which artery? |
Popliteal artery |
|
|
|
Pulse point near the ankle joint is caused by which artery? |
Posterior tibial artery |
|
|
|
Pulse point in the foot is caused by which artery? |
Dorsalis pedis artery |
|
|
|
Artery vs vein structure |
Arteries: much thicker muscular Wall and holds shape
Veins: much thinner muscular walls and lose shape. Have valves. |
|
|
|
What are the three layers present in arteries and veins called? |
Tunica intima Tunica media Tunica adventita |
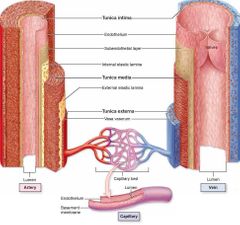
|
|
|
What is the tunica intima? What is it made up of? |
Inner lining of endothelial cells |
|
|
|
What is the tunica media? What is it made up of? |
The middle fibro muscular layer consisting of muscle cells and elastic fibres |
|
|
|
What is tunica adventita? What is it made up of? |
The outermost later made up of elastic tissue and collagen fibres |
|
|
|
Histology of artery vs vein |
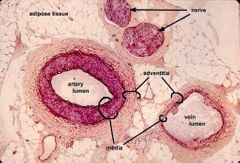
|
|
|
|
What are the three different artery classifications? |
Conducting (elastic) arteries Distribution (muscular) arteries Resistance arteries |
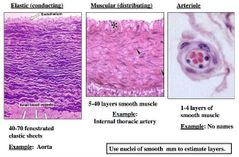
|
|
|
1) What are the properties of conducting (elastic) arteries and what does that allow it to do? |
The tunica media of these arteries has a high elastic fibre content allowing the vessel to cope with large pressure changes |
|
|
|
What are some examples of conducting (elastic) arteries? |
Aorta and its branches The Pulmonary arteries |
|
|
|
2) What are the properties of distribution (muscular) arteries? |
They have a higher content of smooth muscle in tunica media than conducting vessels
These arteries branch and distribute blood to resistance vessels |
|
|
|
What are some examples of distribution (muscular) arteries? |
Radial artery Splenic artery |
|
|
|
3) What are resistance arteries? |
End point or arterioles |
|
|
|
What are the properties of resistance arteries? |
Poorly defined tunica adventita and one/ two layers of smooth muscle
Its diameter can change in response to stimuli such as nervous innervation affecting resistance of blood flow |
|
|
|
4) What are exchange vessels? |
Capillaries or sinusoids |
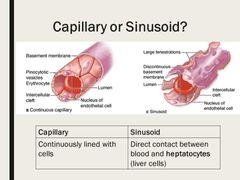
|
|
|
What are the properties of exchange vessels? |
Permits exchange between the blood and interstitial fluid Consists of an endothelial tube (no tunica media or adventita) |
|
|
|
What are sinusoids? |
Capillaries with pores allowing larger plasma proteins to move into interstitial fluid |
|
|
|
After leaving exchange vessels, where does the blood go next? |
Reservoir (capacitance) vessels |
Histology is the same as the one of vein |
|
|
What are reservoir (capacitance) vessels? |
Veins which contain around 70% of blood volume |
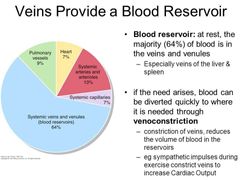
|
|
|
What are the properties of reservoir vessels? How does it respond to changing volume? |
Relatively large tunica adventitia
More complaint than arteries and expand to accommodate changing volume |
|
|
|
Where does the blood go following reservoir vessels? |
Returns back to the heart through veins |
|
|
|
How do veins return blood back to the heart? Name 4 |
Vasoconstrictor tone Pressure from surrounding structure Gravity Respiratory pump |
|
|
|
What is vasoconstrictor tone? |
Refers to the degree the diameter of a vein can be altered to allow changes in blood pressure. This helps increase BP and bring blood back to the heart |
|
|
|
How does pressure from surrounding structures help blood travel through the veins? |
Muscle contraction, artery pulsation and pressure from capillary bed |
|
|
|
How does gravity help bring blood back to the heart? |
Helps return blood from the head and neck |
|
|
|
How does the respiratory pump help bring blood back to the heart? |
During inspiration, intrathoracic pressure is negative and abdominal pressure is positive - pulling blood towards right atrium |
|
|
|
What allows cardiomyocytes to propagate electrical impulses? |
Their branched cells and intercalated discs |
|
|
|
What is a myocyte composed of? |
Bundles of myofibrils that contain myofilaments |

|
|
|
What is a sarcomere? |
The region of myofilament structures between the z-lines |
|
|
|
Muscle contraction mechanism? |
Refer to A Level set |
|
|
|
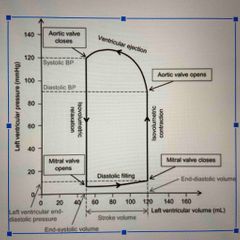
What is preload? |
Degree of stretch in the heart before contraction. The greater the preload (stretch) on the heart, greater the force of contraction (think of it like a rubber band) |
|
|
|
When is the preload increased? |
Hypervolemia (too much fluid in the blood) Heart failure Regurgitation of cardiac valves |
|
|
|
What is contractility? |
Strength of contraction at any preload |
|
|
|
What is afterload? |
Afterload is the pressure against which the heart must work to eject blood during systole (systolic pressure). The lower the afterload, the more blood the heart will eject (increased SV) with each contraction. Eg. Narrowing of blood vessels due to atherosclerosis can increase afterload |
|
|
|
What is Starling law? |
The more the heart fills up with blood, the greater the force of contraction |
|
|
|
Thus what does Starling law demonstrate the relationship between? |
Preload and myocardial contractility |
|
|
|
What is the equation for cardiac output? |
Cardiac output= Heart rate x stroke volume |
|
|
|
The equation for stroke volume? |
End diastolic volume (edv) - End systolic volume (esv) |
|
|
|
Define the basic autonomic control of the heart. How is heart rate increased/ decreased? |
Afferent receptors (chemoreceptors) send information to the CNS where it’s processed. Information is then sent down the sympathetic or parasympathetic pathways (to increase or decrease HR) |
|
|
|
What are 5 sympathetic responses to increase HR? |
Na+ absorption Renin Vasoconstriction increases: Renal vascular resistance, Peripheral vascular resistance Direct contraction of heart |
|
|
|
What is Ischaemia? |
An inadequate blood supply to an organ or part of the body |
|
|
|
What is atherosclerosis? |
A disease characterised by the formation of atherosclerotic plaques in the intima of large (eg. Aorta) and medium sized arteries (eg. Coronary arteries). It is always a generalised disease affecting arteries which supply blood not only to the heart but also organs. |
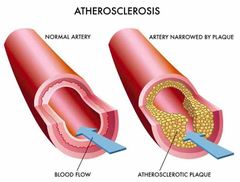
|
|
|
When may ischaemic damage to vital organs may occur? |
When an occlusive thrombus forms on a spontaneously disruptive plaque (atherothrombosis) |
|
|
|
What is occlusion? |
The blockage or closing of a blood vessel or hollow organ |
|
|
|
The formation of atherosclerosis begins at what stage in our lives? |
In young children |
|
|
|
What is the earliest significant lesion called? |
A fatty streak |
|
|
|
What does a fatty streak consist of? |
Lipid containing foam cells in the artery just under the endothelium |
|
|
|
What happens to fatty streaks over time? |
They evolve into atherosclerotic plaques, which remain stable or regress |
|
|
|
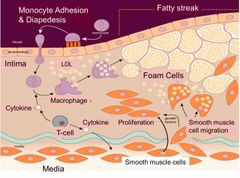
In simple terms, explain the biology of atherosclerosis |
1) Monocytes migrate beneath endothelium 2) They differentiate into macrophages 3) LDL’s enter into the intima of artery where they’re phagocytosis by macrophages |
|
|
|
What is LDL? |
Low density lipoprotein (bad cholesterol) |
|
|
|
What is the name of a macrophage which has engulfed LDLs? |
Foam cell |
|
|
|
Once foam cells form, what do T-cells do? |
They secrete cytokines that induces smooth muscle cells to migrate from the media into the intima. Overtime an accumulation of lipid/ smooth muscle in the intima forms. The growing lesion raises the endothelium into the artery, forming an atherosclerotic plaque |
|
|
|
What are the two categories of plaque? |
Stable and unstable plaques |
|
|
|
What is the difference between stable and unstable plaque in terms of growth? |
Stable plaque grows slowly and unstable grows more rapidly |
|
|
|
Why do stable plaque grow slowly? |
Gradual growth due to the accumulation of lipid in foam cells and migration and proliferation of smooth muscle cells |
|
|
|
What is the difference between stable and unstable plaque in terms of growth? |
Stable plaque grows slowly and unstable grows more rapidly |
|
|
|
Why does unstable plaque grow rapidly? |
As a result of more rapid lipid deposition |
|
|
|
What do both plaques have to stop rupture? What is the major difference? |
Fibrin caps -this matures in stable plaques -this thins out making it prone to rupture |
|
|
|
What happens when a plaque ruptures? |
It can trigger an acute thrombosis (clot) by activating platelets and the clotting cascade |
|
|
|
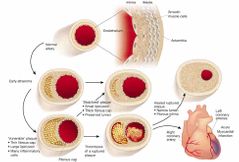
What is stenosis? |
Abnormal narrowing of a body channel |
|
|
|
What causes angina pectoris (coronary artery disease) |
Atherosclerotic narrowing that reduces the lumen of a coronary artery more than 75% causes anyone pectoris |
|
|
|
What symptoms does angina pectoris cause? |
Chest pain that results when pain producing substances accumulate in the myocardium |
|
|
|
In angina pectoris when does the pain come and go? |
Comes on during exertion and disappears with rest, as the substances are washed out by the blood |
|
|
|
What causes angina/ subendothelial myocardial infarction (CAD)? |
When a mural thrombus forms on top of a ruptured plaque |
|
|
|
What is a mural thrombus? |
Where the thrombus (a blood clot that remains in blood vessel) is in contact with the endocardial lining of a large blood vessel such as an artery but isn’t occlusive. |
|
|
|
Variable obstruction of the coronary artery leading to pain at rest or minimal exertion is known as what? |
Unstable angina |
|
|
|
Death of cardiac muscle under the endothelium caused by a mural thrombus is known as what? |
Subendothelial myocardial infarction |
|
|
|
What is acute transmural myocardial infarction? |
A thrombus forms on top of a ruptured plaque and occluded the lumen of the coronary artery. This leads to the death of the full thickness of cardiac muscle supplied by that artery |

|
|
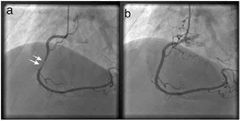
What is it pointing to? |
Severe stenosis |
|
|
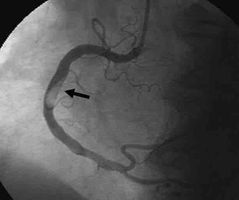
What is it point to? |
Thrombus |
|
|
|
What is peripheral arterial disease? |
When atherosclerosis of arteries of the lower legs causes symptoms of ischaemia and/ or infarction (tissue death due to lack of blood supply) to occur |
|
|
|
What is peripheral arterial disease also known as? |
Peripheral vascular disease |
|
|
|
What are the most common presenting symptoms of Peripheral arterial disease? |
Intermittent clarification (pain in the legs on walking that is relieved by rest. If circulation is severely compromised, the skin can ulcerate, producing lesions that are slow to heal Gangrene of the extremities may occur as a result |

|
|
|
How many L of water in an average person? how much of it is intracellular, interstitial, and intravascular? |
42 L on average Intracellular 28L Interstitial 10.5L Intravascular 3.5L |
|
|
|
What other ions and molecules are in the body? |

Back (Definition) |
|
|
|
What is inciting pressure? |
A form of osmotic pressure exerted by proteins, notably albumin, in a blood vessels plasma and in the opposing force to hydrostatic pressure |
|
|
|
What is hydrostatic pressure? |
The pressure of blood against the wall |
|
|
|
What is acute myocardial infarction? |
Heart attack |
|
|
|
What is oedema? |
An increased volume of interstitial fluid in a tissue or organ |
|
|
|
What causes oedema? |
Raised hydrostatic pressure (eg.cardiac failure) Low oncotic pressure (eg.hepatic disease) Endothelial damage or Impaired lymphatic drainage (tumours) |
Oncotic pressure is a form of osmotic pressure exerted by proteins either in the blood plasma or interstitial fluid. Hydrostatic pressure is a force generated by the pressure of fluid on the capillary walls either by the blood plasma or interstitial fluid. |
|
|
What is haemostasis? |
A process that stops bleeding. It does this by establishing a framework for tissue repair which prevents the loss of blood through damaged blood vessels |
|
|
|
What phases does haemostasis consist of? |
Vascular phase Platelet phase Coagulation phase |
|
|
|
Vascular phase |
Consists of a vascular spasm/ vasoconstriction of the injured vessel (vasodilation of all other vessels). Thus preventing blood loss and bringing. |
|
|
|
Platelet phase |
Platelets adhere to sticky endothelial surfaces, basement membrane and to exposed collagen fibres beneath endothelium. They aggregate (stick together) to form a platelet plug to close the break in vessel. |
|
|
|
Activated platelets release what? |
ADP Thromboxane A2 Serotonin Clotting factors PDGF (platelet derives growth factor) Calcium ions |
|
|
|
What does prostacyclin inhibit? |
Platelet aggregation |
|
|
|
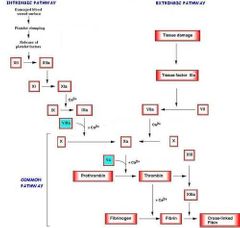
What three pathways does the coagulation phase consist of? |
Extrinsic Intrinsic Common pathways |
|
|
|
During the vascular phase, what do the endothelial cells release? |
ADP Tissue factor Prostacyclin Endothelins |
|
|
|
What does endothelins do? |
Stimulate smooth muscle contraction Vascular spasm Proliferate endothelial cell, muscle fibres, and fibroblasts Endothelial cells become sticky for platelets to adhere to |
|
|
|
Both the extrinsic and intrinsic pathways lead to the formation of what? |
Prothrombin |
|
|
|
What does prothrombinase do? |
Converts prothrombin into thrombin (enzyme) |
|
|
|
What does thrombin do? |
Converts soluble fibrinogen into insoluble fibrin forming the thread of clot |
|
|
|
Deficiency of what vitamin affects coagulation? |
Vitamin K |
|
|
|
What is vitamin K required for? |
Thrombin Factor VII Factor IX Factor X Fibrin clot |
|
|
|
What is vitamin K obtained by? |
Green vegetables Bacteria in the gut |
|
|
|
What triggers the extrinsic pathway? |
TF (tissue factor) CFIII leaks into blood from cells extrinsic to blood vessels. It is released from surface of damaged cells |
|
|
|
In the presence of what ion does TF activate what CF? |
Ca2+ Clotting factor X (CFX) |
|
|
|
How is the intrinsic pathway activated? |
The intrinsic pathway is activated through exposed endothelial collagen inside the vessel. Activated platelets are released |
|
|
|
What do activated platelets release in the intrinsic pathway? |
Platelet phospholipids |
|
|
|
What is activated CFXII converted into? In the presence of what? (intrinsic pathway) |
CFX in the presence of platelet phospholipids and Ca2+ |
|
|
|
Activated CFX combines with what to form what? (common pathway) |
Ca2+ and CFV to form active prothrombinase |
|
|
|
Which of the two pathways is faster? |
Extrinsic is the faster pathway |
|
|
|
What pathway follows the intrinsic/ Extrinsic pathways? |
Common pathway |
|
|
|
What is stage 2 of the common pathway? (Stage one being intrinsic/ extrinsic pathway) |
Prothrombinase and Ca2+ catalyse the conversation of prothrombin to thrombin |
|
|
|
Where is prothrombin produced? |
A plasma protein produced by the liver |
|
|
|
What happens in the stage 3 of the common pathway? |
A sturdy clot is formed |
|
|
|
How is the sturdy clot formed? |
Thrombin and Ca2+ Convert soluble fibrinogen into insoluble loose fibrin threads |
|
|
|
What does thrombin activate during stage 3 of the common pathway? |
CFXIII (released by platelets trapped in the clot) which strengthens the fibrin into a sturdy clot |

|
|
|
There’s two thrombin positive feedback loops in the common pathway. What does the 1at thrombin positive feedback loop involve? |
CFV and accelerates the formation of prothrombinase (so more thrombin is produced) |
|
|
|
What does the 2nd thrombin positive feedback consist of? |
Thrombin activates platelets (PF3) reinforcing aggregation and increasing release of platelet phospholipids |
|
|
|
Describe clot retraction |
The clot pulls torn edges of vessel closer together reducing residual bleeding and stabilising the injury site. This reduces the size of the damaged area making it easier for site to be repaired |
|
|
|
What cells repair the site of a clot? |
Fibrocytes Smooth muscle cells Endothelial cells |
|
|
|
What are CF I, II, III |
Fibrinogen Prothrombin Tissue factor |
|
|
|
What are CF IV, V, VII? |
Calcium ions Proaccelerin Proconvertin |
|
|
|
What are CF VIII, IX, X? |
Antihemophilic Plasma thromboplastin Stuart proper factor |
|
|
|
What are CF XI, XII, XIII? |
Plasma thromboplastin Hageman factor Fibrin stabilising |
|
|
|
Negative feedback on coagulation? What does plasmin do? What releases plasmin? |
Plasmin acts directly on the fibrin mesh and breaks it down. Anti thrombin decreases the production of thrombin from prothrombin and decreases the amount of activated factor X. Protein C and S also act to prevent coagulation, mainly by inactivating factors V and VIII. |
Plasminogen circulates in blood as a zymogen and can be activated to the protease plasmin by two activators named tissue-type plasminogen activator (t-PA) and urokinase-type plasminogen activator (u-PA). |
|
|
What is fibrinolysis? |
Slow process of dissolving the clot |
|
|
|
What substances are required for fibrinolysis? |
Thrombin Protein C Tissue plasminogen (t-PA) (cleaves protein bonds) |
|
|
|
What does plasminogen do in fibrinolysis? |
Produces plasmin which digests fibrin strands |
|
|
|
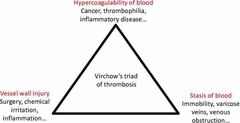
What is the virchow’s triangle? |
Three broad categories of factors that influence the occurrence of thrombosis |
|
|
|
What are the three categories of Virchow’a triangle? |
Hypercoagulability (blood) Vascular damage (vessel) Circulatory stasis (flow) |
|
|
|
State Ohms law |
The idea that the longer and narrower the vessel, the greater the resistance for blood to pass through |
|
|
|
What are short term pressure changes regulated by? Eg. Adjusting quickly from sitting to standing? |
Baroreceptors |
|
|
|
How do aortic arch baroreceptors respond to change in bp? |
Transmits signals to cardiovascular centre via vagus nerve -which regulates SYSTEMIC blood pressure |
|
|
|
Where are carotid sinus baroreceptors found? |
Internal carotid artery |
|
|
|
Describe the pathways of carotid sinus baroreceptors |
Internal carotid artery Glossopharyngeal nerve Monitoring of bp in head and neck |
|
|
|
Where are high pressure baroreceptors locates compared to low pressure detecting ones? |
High- aortic arch, carotid sinus Low- cardiopulmonary receptors |
|
|
|
What do cardiopulmonary receptors send to the brain? |
Information about the fullness of the vascular system |
|
|
|
Where are cardiopulmonary receptors found? |
Vena cava Pulmonary trunk Vein and atrium of right ventricle (All major deoxygenated sites) |
|
|
|
Where are chemoreceptors found? |
Arch of aorta In each common carotid artery |
|
|
|
When do chemoreceptors activate? |
Low pH Low O2 CO2 levels are high Lactate (Detect bp through molecules in blood) |
|
|
|
What is the bainbridge reflex? |
Positive feedback mechanism in which there is a compensatory increase in heart rate, due to a rise in right arterial pressure The Bainbridge reflex, also called the atrial reflex, is an increase in heart rate due to an increase in central venous pressure. |
|
|
|
What increases contractility? |
Positive intropic agents increase contractility: Epinephrine and norephrine which increase Ca2+ inflow (even angiotensin 2) |
|
|
|
What decreases contractility? |
Negative inotropic agents: eg. Ca2+ blockers |
|
|
|
What three factors affect stroke volume? |
Preload Afterload Contractility |
|
|
|
What does warfarin inhibit? |
II VII IX X |
Warfarin decreases blood clotting by blocking an enzyme called vitamin K epoxide reductase that reactivates vitamin K1. Without sufficient active vitamin K1, clotting factors II, VII, IX, and X have decreased clotting ability. The anticlotting protein C and protein S are also inhibited, but to a lesser degree. |
|
|
What happens if cardiac output rises due to an increase in stroke volume or heart rate, but resistance stays the same? |
Blood pressure increases |
|
|
|
What prevents excessive rise in bp during intense exercise? |
Activation of (carotid) baroreceptors |
|
|
|
Sympathetic nerves arise from what vertebral levels to increase the rate of heart contraction? |
T1 - T4 |
|
|
|
What part of the heart is also known as the moderator band and why? |
Septomarginal trabecula; carries part of the right bundle branch to the anterior papillary muscle of the right ventricle. Acts as an electrical shortcut across the chamber and allows the tricuspid valve to close shut before ventricular contraction |

|
|
|
What is something that happens to the left bundle branch but not the right bundle branch? |
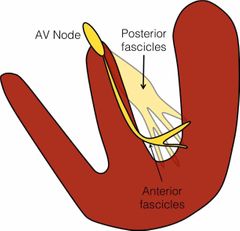
Splits into two. An anterior and posterior fascicles |
|
|
|
What does the rate at which the SA generates electrical impulses relied on? |
Autonomic nervous system |
|
|
|
Where does SA lie? |
Junction of superior vena cava and right atrium |
|
|
|
What happens in the refractory period following a contraction? |
Ca2+ are allowed to return to intracellular stores and the Na+/K+ to reset extracellular ion levels |
|
|
|
What are some channels only present in pacemaker cells? What do the do? |
HCN-gated channels These support K+ efflux and Na+ influx but Na+ influx dominates |
|
|
|
Pacemaker cells phases |
No phase 1 and 2 |
|
|
|
What cells link atrial myocytes together through gap junctions? |
Nodal cells |
|
|
|
Why can the atrial wave of depolarisation not reach ventricles? |
Due to cartilage and fibrous material and AV junction. Acts like an electrical insulator. Signals have to go through the AV node |
|
|
|
What substance does the sympathetic nervous system release to increase heart rate? |
Norepinephrine onto nodal cells |
|
|
|
What does norepinephrine do? |
Binds to B-1 adrenergic receptors which are G-protein couple receptors. This produces cAMP. Eventually increases probability of HCN channels opening causing faster influx of Na+ causing threshold potential to be reached quicker |
|
|
|
What do parasympathetic fibres release via vagus nerve to slow heart rate? |
ACh on nodal cells |
|
|
|
Which cells does ACh bind to to bring what action? |
M2 receptors (also G-protein coupled) Less camp produced, less HCN opening etc... |
|
|
|
What channels are responsible for the funny current? |
HCN channels (the more they open, the greater the influx of Na+, the faster the threshold is reached, increased heart rate) |
|
|
|
Note: |
If a question asks about receptors and bp, not mentioning pH, O2 etc. The answer is baroreceptors |
|
|
|
What two mechanisms regulate contractility? |
Autonomic nervous system Frank starling law |
|
|
|
According to frank starling law, increasing the resting length of a muscle leads to... |
More optimum overlap of action and myosin - contractility increases |
|
|
|
Where does majority of the ca2+ in cardiac muscles come from? |
I-type ca2+ channels in the t-tubules (contrasting to skeletal where majority is stored in sarcoplasmic reticulum). This results in cardiac contraction being dependent on the extra cellular levels of Ca2+ |
|
|
|
Which channel/ pump is open during the plateau phase of the action potential in cardiac myocytes? |
Voltage gated calcium channels |
|
|
|
Which pump/channel removed calcium to the extra cellular space? |
Sodium/ calcium exchanger |
|
|
|
Which channels/ pump plays the most important role in depolarising cardiac myocytes? |
Voltage gated potassium channel |
|
|
|
Which pump/ channel causes rapid upstroke of the action potential in cardiac myocytes? |
Voltage gated sodium channel |
|
|
|
Which channel/ pump is blocked by local anaesthetics? |
Voltage gated sodium channel |
|
|
|
What is the ejection fraction calculated by? |
Dividing stroke volume by end-diastolic volume |
|
|
|
What happens to heart rate when a person moves from sitting to standing? |
As a result of the reduction in cardiac output and stimulation of a branch of the autonomic nervous system, heart rate increases |
|
|
|
What is the mechanism most associated with local control of increased muscle blood supply? |
Accumulation of adenosine |
|
|
|
What is the physiological mechanism most associated with global increase in cardiac output due to increased lactate levels? |
Activation of aortic arch chemoreceptors |
|
|
|
What is the physiological mechanism most associated with the prevention of excessive rises in blood pressure during very intense exercise? |
Activation of carotid baroreceptors |
|
|
|
What is the mechanism responsible for increase in cardiac output in anticipation of the need to exercise? |
Activation of brain stem control centres via cortical flow |
|
|
|
Embryology of the heart. What is the depression on the interatrial wall? |
Fossa ovalis |
|
|
|
What receives the umbilical, vitelline and cardinal veins? |
Sinus venous |
|
|
|
What is a membrane tissue that grows in a crescenteric shape to fuse with the endocardial cushions? |
Septum primum |
|
|
|
What shunts blood from the left umbilical vein into the inferior vena cava? |
Ductus venous |
|
|
|
What is closed by increased blood flow in the left atrium? |
Foramen ovale |
|
|
|
What is the antagonist of Vitamin K? |
Warfarin |
|
|
|
What is a mixture of mucopolysaccharides derived from mast cells, and activates antithrombin? |
Heparin |
|
|
|
What innervates the heart? |
The heart is innervated by vagal and sympathetic fibers. The right vagus nerve primarily innervates the SA node, whereas the left vagus innervates the AV node; however, there can be significant overlap in the anatomical distribution |
|
|
|
Which vessel commences at the level of the right sternoclavicular joint and then passes laterally posterior to the clavicle? |
Right subclavian |
|
|
|
Remember: |
Right common and subclavian arteries come off the BRACHIOCEPHALIC |
|
|
|
Semilunar valves are composed of connective tissues covered in? |
Endocardium |
|
|
|
This attaches to the cusps of the mitral and tricuspid valves |
Fibrous skeleton |
|
|
|
What is the innermost surface of the heart? |
Endocardium |
|
|
|
Which layer is the Cardiac musle found in? |
Myocardium |
|
|
|
What is the parietal pericardium composed of? |
Mesothelium |
|
|
|
Name two layers continous with each other? |
Epicardium and parietal pericardium |
|

