![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
118 Cards in this Set
- Front
- Back

What is the term for non-infectious ulcers of the oral mucosa?
|
Aphthous ulcer (canker sore)
|
|
What is the cause of Canker Sores / Aphthous ulcers?
|
Unknown etiology
|
|
How common are Canker Sores / Aphthous ulcers? When?
|
- Extremely common: up to 35-40% of population
- More common in first two decades of life - Prevalent within some families |
|
How long do Canker Sores / Aphthous ulcers last?
|
Usually resolve in 7-10 days or persistent for weeks
|
|

What causes "cold sores"?
|

Herpes Stomatitis (HSV type 1)
- Person-to-person transmission |
|
|
What are the symptoms of Herpes Stomatitis / cold sores?
|

- Asymptomatic: virus can persist in dormant state
- Reactivates to form vesicles ("cold sores") |
|
|
What happens when Herpes Stomatitis reactivates?
|
- Intraepithelial edema → clear fluid → rupture → ulcer
- Multinucleated cells w/ intra-cellular viral inclusions |
|

How do you test for / diagnose Herpes Stomatitis?
|
Tzanck test - swab ulcer and smear on slide
Look for 3 M's: - Multinucleated cells - Molding (stick together) - Margination (chromatin pushed to side, dark purple) |
|
|
What is the most common fungal infection of the oral cavity?
|
Candidiasis or "Thrush"
|
|
|
What are the causes of Candidiasis?
|
- Dentures
- Diabetes Mellitus - Steroids / prolonged antibiotic therapy - Widespread cancer - Immunosuppression: transplant, AIDS, etc |
|
|
What is the appearance of Candidiasis?
|
- White plaque like pseudomembrane
- You can scrape it off, which exposes an erythematous base |
|
What does it mean if the white plaque in the oral cavity can be pealed off? What if it can't be pealed off?
|
- Removable: Candidiasis
- Non-removable: Leukoplakia |
|
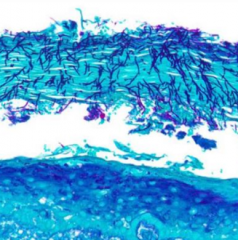
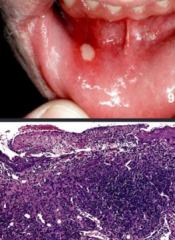
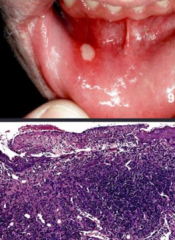
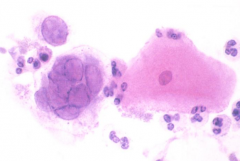
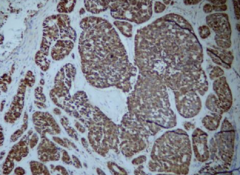
What does this microscopic image show?
|
- Fungal hyphae superficially attached to underlying mucosa = Candididasis
- Special stain = GMS (silver) |
|
|
What kind of lesion in the mouth is associated with HPV? What does it look like?
|

Squamous Papilloma = benign epithelial hyperplasia
- Soft, finger like projections |
|
|
What virus is associated with Squamous Papilloma?
|

Low risk sub-types HPV 6 and 11
|
|
|
When is it most common to get Squamous Papilloma? Is it contagious?
|
Usually from 30-50; not contagious
|
|
|
Where do you get Squamous Papilloma lesions?
|

- Lingual (tongue)
- Labial (lips) - Buccal (cheek) - Larynx |
|
|
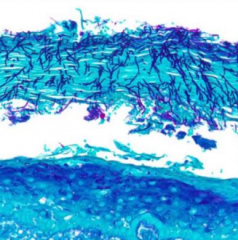
What is the microscopic appearance of Squamous Papilloma?
|
Papillary (finger-like) hyperplasia of squamous mucosa w/ fibrovascular cores
|
|
|
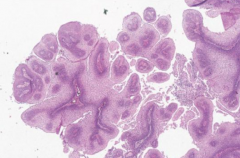
What benign lesions can form on the vocal cords d/t smoking or vocal abuse?
|
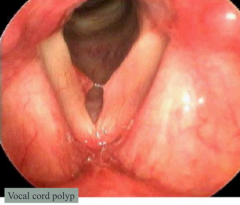
Vocal Cord Nodules and Polyps
|
|
|
How do vocal cord nodules and polyps compare?
|

- Nodules are BILATERAL on opposing surfaces of the middle third of vocal cord
- Polyps are SINGLE in the ventricle or Reinke's space - Both smooth and rounded - No cancer risk |
|
|
What increases the risk for Vocal Cord Nodules and Polyps? Who is more likely to get it?
|
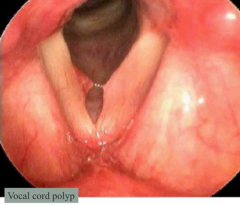
- Smoking
- Vocal abuse - M > F |
|
|
What are the precancerous lesions of the oral cavity?
|
- Leukoplakia
- Erythroplakia |
|
|
How does Leukoplakia compare to Erythroplakia in appearance?
|
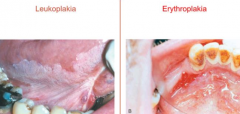
- Leukoplakia: white patch caused by epidermal thickening of hyperkeratosis
- Erythroplakia: red granular area that may or may not be elevated w/ poorly defined boundaries |
|
|
How does Leukoplakia compare to Erythroplakia in epithelial changes?
|
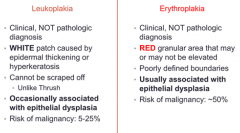
- Leukoplakia: OCCASIONALLY associated with epithelial dysplasia
- Erythroplakia: USUALLY associated with epithelial dysplasia |
|
|
How does Leukoplakia compare to Erythroplakia in risk for malignancy?
|
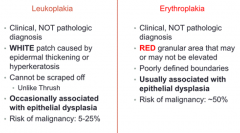
- Leukoplakia: 5-25%
- Erythroplakia: ~50% |
|
|
How do you diagnose Leukoplakia and Erythroplakia?
|
Both clinical, not pathologic diagnoses
|
|
|
Which lesion causes white patches in the oral cavity that cannot be scraped off? Can be?
|
- Can't scrape off: Leukoplakia
- Can scrape off: Erythroplakia |
|
|
What is the sequence of events for development of squamous cell carcinoma?
|

1. Hyperplasia
2. Dysplasia 3. Carcinoma |
|
|
What is the first event in development of squamous cell carcinoma?
|
Hyperplasia: increased number of cells
|
|
|
What is the second event in development of squamous cell carcinoma?
|
Dysplasia: progressively increasing degrees of pleomorphism, hyperchromasia, increased nuclear size, and nuclear/cytoplasmic ratio
|
|
|
What is the third event in development of squamous cell carcinoma?
|
Squamous Cell Carcinoma
- Can lead to invasion / infiltration of submucosa |
|
|
How does the amount of dysplasia correlate to the risk of developing squamous cell carcinoma?
|
- Mild dysplasia: 1-2% over 5-10 years
- Severe dysplasia: 5-10% over 5-10 years - Dysplastic changes often regress after smoking stops |
|
|
What are the features of Epithelial Dysplasia (second event in development of squamous cell carcinoma)?
|
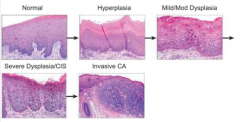
- Proliferation of immature (basal) cells
- Loss of cell polarity - Increased number of mitotic figures - Variation in nuclear size and shape - Hyperchromasia |
|
|
What characterizes 95% of oral and laryngeal cancers? When are they more likely?
|
Squamous Cell Carcinoma
- Age: 50-70 years - M > F |
|
|
Why has the survival rate not improved for oral and laryngeal cancers?
|
There is a lack of earlier detection
|
|
|
What is Squamous Cell Carcinoma in the oral cavity and larynx associated with?
|
- Tobacco: cigarettes, chewing tobacco, snuff
- Alcohol (synergistic effect with tobacco) - Family history - HPV infection (16 and 18) - Leukoplakia (occasionally) - Erythroplakia (commonly) |
|
|
Which HPV serotypes are associated with upper respiratory tract cancer vs benign squamous papilloma?
|
- Cancer: 16 & 18
- Papilloma: 6 & 11 |
|
|
Where in the mouth are Squamous Cell Carcinoma lesions?
|
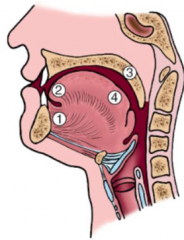
- Most: tongue (2) and floor of mouth (1)
- Also: gingiva, hard/soft palates (3), dorsal tongue (4), mucosa |
|

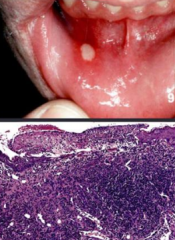
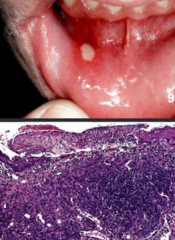
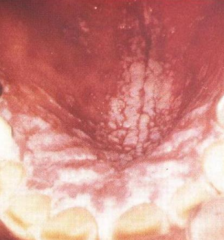
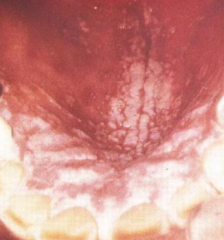
What does this image show?
|

Squamous Cell Carcinoma on the tongue
|
|
|
What is the prognosis of oral Squamous Cell Carcinoma?
|
5-year survival:
- Early stage oral SCC: 80% - Late stage oral SCC: 19% |
|
|
Where does oral Squamous Cell Carcinoma metastasize to?
|
- Regional lymph nodes: submental and cervical
- Distant: lung, liver, bone, mediastinal lymph nodes |
|
|
What is the most common location of laryngeal carcinoma?
|
Glottis (true vocal cords)
|
|
|
What are the symptoms of squamous cell carcinoma on the glottis (true vocal cords)?
|

Hoarseness: makes it diagnosed at earlier stage
|
|
|
What are the symptoms of carcinoma on the supraglottis or infraglottis?
|
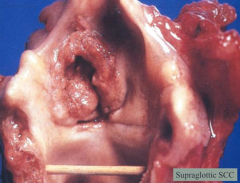
- Usually asymptomatic early in course
- Diagnosed at later stages (not until symptoms secondary to mass size such as breathing or voice problems) |
|
|
What are the symptoms of laryngeal carcinoma that spreads to adjacent structures?
|
- Hemoptysis
- Dysphagia |
|
|
How do you treat laryngeal squamous cell carcinoma? Prognosis?
|
- Surgery: laryngectomy
- Radiation 5 year survival: - Stage 1 = 70% - Stage 40 = 30% |
|
|
What happens if someone is infected with HPV serotypes 16 and/or 18?
|
- HPV proteins E6 and E7 inactivate p53 and Rb
- Leads to Squamous Cell Carcinoma (keratinizing and non-keratinizing) |
|
|
Where does Non-Keratinizing Squamous Cell Carcinoma occur?
|
Waldeyer's Ring:
- Base of tongue - Tonsils (palatine, adenoids) |
|
|
What kind of cells are in the nasal vestibule? Posterior nasal cavity and sinuses? Nasal septum?
|
- Nasal Vestibule: Squamous
- Posterior Nasal Cavity and Sinuses: Respiratory (Ciliated Pseudostratified Columnar) - Nasal Septum: Cartilage and Lamellar bone |
|
|
What are the causes of Rhinosinusitis?
|
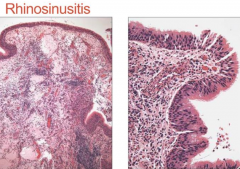
- Viral (common cold)
- Allergic - Obstructive process (eg, deviated septum) |
|
|
What are the histological features of Rhinosinusitis?
|
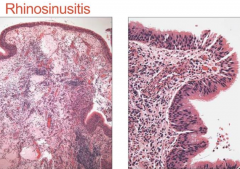
- Mixed inflammatory infiltrate
- Edema - Thickened basement membrane |
|
|
What are the complications of Rhinosinusitis?
|
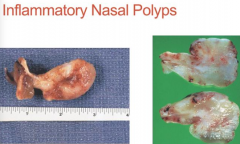
Nasal Polyps
|
|
|
What are the types of nasal cavity and paranasal sinus tumors?
|
Benign:
- Schneiderian Papilloma Malignant: - Olfactory Neuroblastoma (Esthesio-neuroblastoma) - Nasopharyngeal Carcinoma |
|
|
What benign neoplasm can form from the nasal mucosa? What kind of epithelium?
|
- Schneiderian Papillomas
- Arise from ciliated columnar epithelium |
|
|
What are the clinical symptoms of Schneiderian Papillomas?
|
Non-specific:
- Nasal obstruction - Headaches - Epistaxis - Rhinorrhea - Facial pressure |
|
|
What are the types of Schneiderian Papillomas?
|
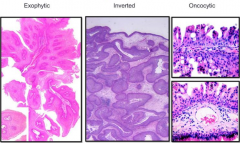
- Exophytic
- Endophytic (inverted) - Cylindrical |
|
|
What is Schneiderian Papillomas associated with?
|
HPV (mostly 6 and 11)
|
|
|
Which type of Schneiderian Papillomas has the highest recurrence rate? Prognosis?
|
- Endophytic (inverted) ~60% recurrence
- Excellent prognosis if no malignant transformation |
|
|
What type of neoplasm forms from neuroendocrine cells
|
Olfactory Neuroblastoma (Esthesio-neuroblastoma)
|
|
|
Where does Olfactory Neuroblastoma (Esthesio-neuroblastoma) occur?
|
Superior and lateral mucosa of nose (olfactory mucosa)
|
|
|
What are the symptoms of Olfactory Neuroblastoma (Esthesio-neuroblastoma)? Median age of occurrence?
|
- Epistaxis
- Nasal obstruction - Headache - Median age: 50 years |
|
|
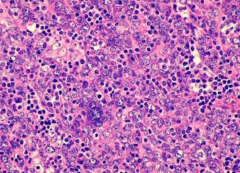
What is the microscopic appearance of Olfactory Neuroblastoma (Esthesio-neuroblastoma)?
|
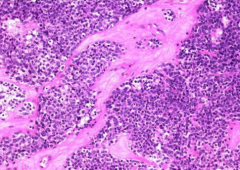
- Uniform cells with round nuclei
- Scant cytoplasm - "Salt and pepper" chromatin - Neurosecretory granules |
|
|
What is immunochemistry marker of Olfactory Neuroblastoma (Esthesio-neuroblastoma)?
|
Neuroendocrine markers: synaptophysin and chromogranin
|
|
|
What is the prognosis for Olfactory Neuroblastoma (Esthesio-neuroblastoma)?
|
- Locally invasive
- Metastasizes widely: local lymph nodes and lungs - 5-year survival 50-70% |
|
|
Where is Nasopharyngeal Carcinoma more common?
|
- Africa
- China (Hong Kong most frequently) |
|
|
What are some causes of Nasopharyngeal Carcinoma?
|
** EBV infection
- Diet (salted fish) - Smoking - Hereditary |
|
|
What are the types of Nasopharyngeal Carcinoma?
|
- Keratinizing Squamous Cell Carcinoma
- Non-Keratinizing Squamous Cell Carcinoma |
|
|
What are the features of Non-Keratinizing Squamous Cell Carcinoma Nasopharyngeal Carcinoma?
|
- Undifferentiated
- Lymphoepithelial carcinoma (numerous lymphocytes between tumor cells obscuring the epithelial (cohesive) derivation) |
|
|
What is the prognosis for Nasopharyngeal Carcinoma?
|
- Grows silently until they become unresectable
- Local regional lymph nodes (cervical) and distant metastasis - 50-70% 3-year survival rate |
|
|
How do you treat Nasopharyngeal Carcinoma?
|
Radiotherapy
|
|
|
What are the major salivary glands? What kinds are they?
|
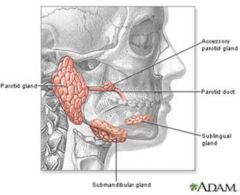
- Parotid gland: serous
- Submandibular gland: mixed, mainly serous - Sublingual gland: mixed, mainly mucinous |
|
|
Where are the minor salivary glands?
|
Innumerable distributed throughout the mucosa of the oral cavity (lips, gingiva, floor of mouth, cheek, hard and soft palates, tongue, tonsillar areas, oropharynx)
|
|
|
What is the function of salivary glands?
|
- Mastication
- Digestion - Protection of teeth |
|
|
Where does saliva come from?
|
Acinar-Ductal unit
|
|
|
Parotid Gland:
- Size - Type of cells - Lymph nodes - Duct |
- 14-30 grams
- Almost exclusively serous cells - Abundant adipose tissue - Intraparenchymal lymph nodes w/ epithelial inclusions - Parotid duct - Accessory gland |
|
|
Submandibular Gland:
- Size - Type of cells - Lymph nodes - Duct |
- 7-8 grams
- 90% serous cells, 10% mucous cells - No lymph nodes - Wharton's duct |
|
|
Sublingual Gland:
- Size - Type of cells - Organization - Duct |
- 2-3 grams
- Predominantly mucous cells - Serous cell demilunes - Poorly encapsulated - Multiple Bartholin's ducts |
|
|
Minor Salivary Glands:
- Organization - Location - Type of cells |
- Unencapsulated
- Throughout oral cavity - Variable cell types: mixed seromucinous, mucous only, or serous only |
|
|
What is the autoimmune disease that affects the salivary and lacrimal glands?
|
Sjogren Syndrome
|
|
|
What are the symptoms of Sjogren Syndrome?
|
- Xerostomia (dry mouth)
- Keratoconjunctivitis (dry eyes) - Often associated with other autoimmune diseases (RA, lupus, etc) |
|
|
What are the serological features of Sjogren Syndrome?
|
* Anti-SS-B
- Anti-SS-A |
|
|
What happens in Sjogren Syndrome?
|
Lymphocytic (autoimmune) infiltration of salivary and lacrimal glands w/ eventual gland destruction
|
|
|
What is Mikulicz disease?
|
- Benign lymphoepithelial lesion
- Type of benign enlargement of the parotid and/or lacrimal glands - This pathologic state is sometimes, but not always, associated with Sjögren's syndrome |
|
|
How common are neoplasms of the salivary glands? Who gets them?
|
< 2% of all human tumors
- Most occur in adults (benign from 40s-60s, malignant slightly older) - 5% occur in children younger than 16 years - Slight F > M |
|
|
Which salivary glands are more likely to get neoplasms?
|
- 65-80% in parotid gland
- 10% in submandibular gland - Remainder in minor salivary glands |
|
|
What affects the likelihood of a neoplasm of the salivary glands becoming malignant?
|
Likelihood of it becoming malignant is inversely proportional to size of gland (eg, bigger glands are more likely to be benign)
- 15% of parotid gland tumors are malignant - 40% of submandibular gland tumors are malignant - 50% of minor salivary gland tumors are malignant - 70-90% of sublingual gland tumors are malignant |
|
|
Which kind of salivary gland is most likely to have malignant neoplasms? Least likely?
|
- Most likely: Sublingual (70-90%)
- Least likely: Parotid (15%) bigger glands are more likely to be benign and vice versa |
|
|
What are the benign neoplasms of the salivary glands?
|
* Pleomorphic Adenoma (60%)
* Warthin tumor (5-10%) |
|
|
What are the malignant neoplasms of the salivary glands?
|
* Mucoepidermoid Carcinoma (15%)
* Adenoid Cystic Carcinoma (5%) |
|
|
What is the most common salivary gland tumor? Benign/Malignant?
|
Pleomorphic Adenoma - benign salivary gland neoplasm (50-60% of all salivary gland tumors)
|
|
|
Where do Pleomorphic Adenomas most commonly occur?
|
75-85% occur in parotid
|
|
|
What are the characteristics of a Pleomorphic Adenoma?
|
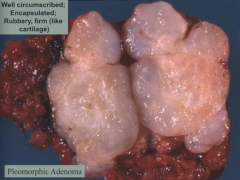
- Most common salivary gland tumor
- Well circumscribed and encapsulated - Rubbery, firm (like cartilage) Benign Mixed Tumor: - Epithelial cells (ductal) - Myoepithelial cells - Mesenchymal components: myxoid, hyaline, chondroid Pleomorphic: - Variability (cell types and composition) Adenoma: - Proliferation of cells (epithelial and myoepithelial) |
|
|
What is the clinical course of Pleomorphic Adenoma?
|
- Painless, slow-growing
- Local recurrence of 4% - Malignant transformation is uncommon (2% for tumors present for <5y; 10% for tumors present for >10y) |
|
|
What is the second most common salivary gland tumor? Benign/Malignant?
|
Warthin Tumor - benign (5-10%)
|
|
|
Where do the first and second most common neoplasms of the salivary glands most commonly affect?
|
- Pleomorphic Adenoma - most occur in parotid gland
- Warthin Tumor - restricted to parotid gland (bilateral) |
|
|
Who is most likely to get a Warthin Tumor?
|
- M > F
- Associated w/ smoking |
|
|
What is the most common bilateral salivary gland tumor?
|
Warthin Tumor (benign)
|
|
|
What does a Warthin tumor look like?
|
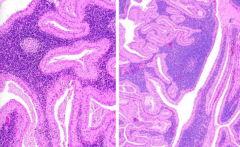
- Papillary cystic change
- Bilayered oncocytic (pink) epithelial cells (= oncocytes) and lymphocytes |
|
|
What is the most common malignant tumor of the salivary glands?
|
Mucoepidermoid Carcinoma
|
|
|
Where does Mucoepidermoid Carcinoma most commonly occur? In whom?
|
- 50% in parotid gland
- 40% in minor salivary glands - Occurs in both adults and children |
|
|
What kind of cells are present in Mucoepidermoid Carcinoma?
|
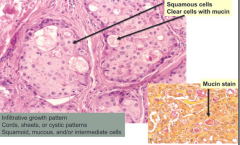
Mixture of squamous, mucous, and intermediate cells
- Infiltrative growth pattern - Cords, sheets, or cystic growth patterns |
|
|
What is the prognosis for Mucoepidermoid Carcinoma?
|
- Low grade tumors invade locally, rarely metastasize, 5 year survival is >90%
- Intermediate/High grade tumors recur more frequently, metastasize in 30%, 5 year survival is ~50% |
|
|
How do you treat Mucoepidermoid Carcinoma?
|
Surgical resection followed by radiation
|
|
|
What is the least common salivary gland tumor we need to know? Benign/Malignant?
|
Adenoid Cystic Carcinoma
- 10% of all salivary gland carcinomas |
|
|
Where do Adenoid Cystic Carcinoma most commonly occur?
|
* Minor salivary glands more commonly
- Can also occur in major salivary glands |
|
|
What are the microscopic features of Adenoid Cystic Carcinoma?
|
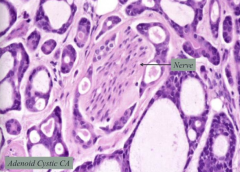
- Perineural invasion
- Cribriform architecture |
|
|
What is the prognosis for Adenoid Cystic Carcinoma? Treatment
|
- Local recurrence
- Wide to radical surgical resection |
|
|
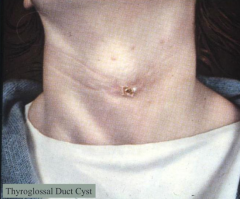
What midline developmental cyst is always connected to the hyoid bone?
|
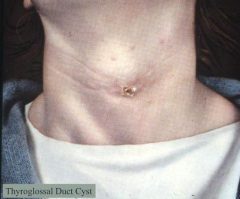
Thyroglossal Duct Cyst
|
|
|
When and where do Thyroglossal Duct Cysts occur?
|
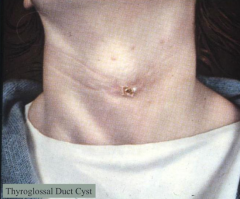
- Occurs prior to 4th decade
- Midline, connected to hyoid bone |
|
What kind of cells are in a Thyroglossal Duct Cyst?
|
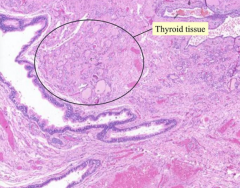
- Lined by respiratory or squamous epithelium
- Thyroid tissue in wall of cyst |
|
|
What are the implications of a Thyroglossal Duct Cyst being attached to the hyoid bone?
|
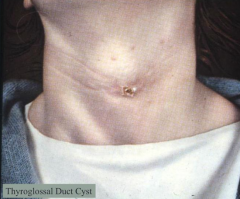
Moves with swallowing
|
|
|
What abnormality in the soft tissue of the neck arises from the 2nd branchial pouch?
|
Branchial Cleft Cyst (Cervical Lymphoepithelial Cyst)
|
|
|
Which branchial pouch does the Branchial Cleft Cyst arise from? How old are people when they get these?
|
- 2nd branchial pouch
- 75% of patients are between 20-40 years |
|
|
What is the location of Branchial Cleft Cysts?
|
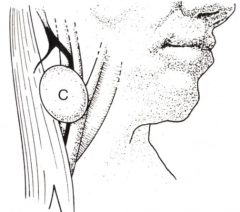
Laterally placed in neck along anterior border of SCM
|
|
|
What can happen to a Branchial Cleft Cyst
|
May become infected
|
|
|
What does a Branchial Cleft Cyst look like grossly?
|
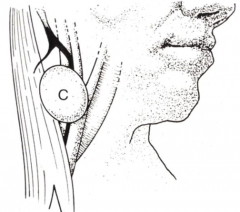
- Thin-walled
- Filled with cheesy, mucoid material |
|
|
What does a Branchial Cleft Cyst look like microscopically?
|
Squamous lining, filled w/ lymphoid tissue
|
|
|
What do you need to distinguish a Branchial Cleft Cyst from on your differential?
|
Metastatic Squamous Cell Carcinoma
|

