![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
What are the characteristics of the R bronchus?
|
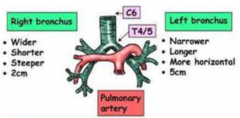
- Wider
- Shorter - Steeper - 2 cm |
|
|
What are the characteristics of the L bronchus?
|
- Narrower
- Longer - More horizontal - 5 cm |
|
|
Which bronchi is an inhaled foreign body more likely to enter? Why?
|
Right Bronchus:
- Wider - Shorter - Steeper - 2 cm |
|
|
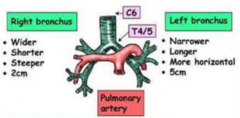
Which part of the respiratory system is lined w/ respiratory epithelium? What kind of epithelium?
|
- Lines airways proximal to the respiratory bronchioles
- Pseudostratified ciliated columnar epithelium |
|
|
What is the acinus?
|
Airway structures distal to the terminal bronchiole:
- Respiratory Bronchiole - Alveolar Duct - Alveolus |
|
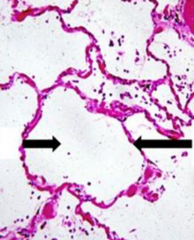
What are the L & R arrows pointing at?
|
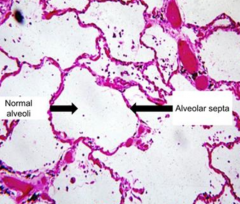
L: Normal Alveoli
R: Alveolar Septa |
|
|
What kind of cells cover 95% of the alveolar surface
|
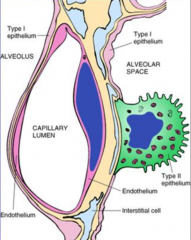
Type 1 Pneumocytes
|
|
|
What is the function of Type 2 Pneumocytes?
|
- Produce surfactant
- Repair alveolar epithelium |
|
|
Describe the continuity of the alveolar septum?
|
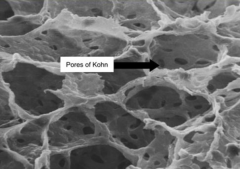
- Fenestrated
- Pores of Kohn - Important for exchange of substances |
|
|
What is Atelectasis?
|
State in which the lung, in whole or in part, is COLLAPSED or without air; loss of lung volume d/t inadequate expansion of air-spaces
|
|
|
What are the types of Atelectasis?
|
1. Resorptive
2. Compressive 3. Loss of Surfactant (neonatal) 4. Contraction |
|
|
What are the acquired forms of Atelectasis?
|
- Resorptive
- Compressive - Contraction |
|
|
What kind of Atelectasis is the consequence of COMPLETE airway obstruction?
|
Resorption Atelectasis
|
|
|
What causes Resorption Atelectasis?
|
Complete Airway Obstruction:
- Mucus/mucopurulent plug following surgery - Aspiration of foreign materials - Bronchial asthma, bronchitis, bronchiectasis - Bronchial neoplasms (caveat - total obstruction) |
|
|
Where does the obstruction occur in Resorption Atelectasis?
|
Complete Airway Obstruction occurs in bronchi, subsegmental bronchi, or bronchioles
|
|
|
What are the consequences of Resorption Atelectasis?
|
- Prevents air from reaching the alveoli
- Resorption of air trapped in distal airspaces through the pores of Kohn - Lack of air in distal airspaces - Collapse |
|
|
What are the clinical findings of Resorption Atelectasis?
|
* Fever and dyspnea w/in 24-36 hours of collapse
- Ipsilateral deviation of trachea - Ipsilateral diaphragmatic elevation - Absent breath sounds and absent vocal vibratory sensation (tactile fremitus) - Collapsed lung does not expand on inspiration |
|
|
What is the most common cause of fever 24-36 hours after surgery?
|
Resorption Atelectasis
|
|
|
What kind of Atelectasis is caused by air or fluid accumulation in the pleural cavity, causing collapse of the underlying lung?
|
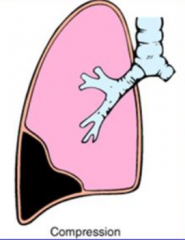
Compression Atelectasis
|
|
|
What causes Compression Atelectasis?
|
Air or fluid accumulation in pleural cavity, increases pressure and collapses underlying lung
|
|
|
What are some examples of Compression Atelectasis?
|
- Tension Pneumothorax
- Pleural Effusion |
|
|
What are the clinical findings of Compression Atelectasis?
|
- Trachea and mediastinum shift AWAY from atelectatic lung (contralateral side)
|
|

What is happening in these lungs?
|

Compression Atelectasis d/t Pneumothorax:
- Note that R lung has a darker / lucent appearance because of presence of air occupying almost entire pleural space - R lung is next to mediastinum - Deviation of trachea to contralateral side |
|
What is happening in these lungs?
|
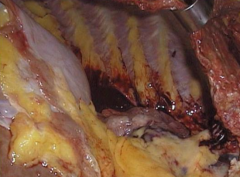
Compression Atelectasis d/t Pleural Effusion
- Lung should be taking up entire space - Pleural Effusion filled entire space, but was drained before doing autopsy |
|
|
What happens to the alveoli during Compression Atelectasis?
|
Alveoli collapse into slit-like spaces
|
|
|
What is the cause of Neonatal Atelectasis?
|
Loss of Surfactant
|
|
|
What are the components of Surfactant?
|
Lipids:
- Phosphatidylcholine (Lecithin) - Phosphatidylglycerol Proteins: - Surfactant proteins A and D - Surfactant proteins B and C |
|
|
What is the function of the proteins in Surfactant?
|
- A and D: innate immunity
- B and C: reduces surface tension at air liquid barrier in alveoli |
|
|
Where is Surfactant stored?
|
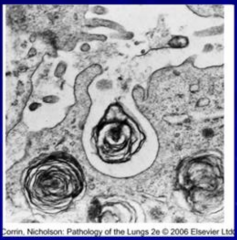
Lamellar bodies
|
|
|
What is the function of Surfactant?
|
- Reduces surface tension in small airways
- Prevents collapse of airways on expiration |
|
|
What modulates the synthesis of surfactant?
|
- ↑ by cortisol and thyroxine
- ↓ by insulin |
|
|
What can cause Neonatal Atelectasis?
|
Decreased surfactant in fetal lungs:
- Prematurity - Maternal diabetes (fetal hyperglycemia stimulates insulin release) - C-section (labor and vaginal delivery ↑ stress related cortisol secretion which ↑ surfactant production) |
|
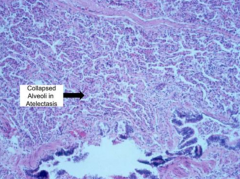
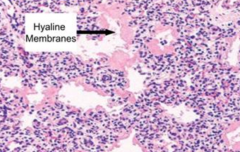
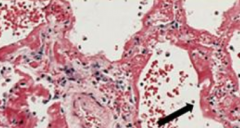
What is happening in this image?
|
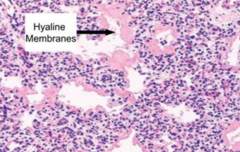
Neonatal Atelectasis: collapsed alveoli are lined by hyaline membranes
|
|
|
What happens to the alveoli during Neonatal Atelectasis?
|
Collapsed alveoli are lined by hyaline membranes
|
|
|
What are the clinical findings of Neonatal Atelectasis?
|
- Respiratory distress w/in a few hours after birth
- Hypoxemia → Respiratory Acidosis - Ground glass appearance (opacified and pale) on chest x-ray |
|
|
What are the complications of Neonatal Atelectasis?
|
- Intraventricular hemorrhage
- PDA (persistent hypoxemia) - Necrotizing enterocolitis (intestinal ischemia) - Hypoglycemia (excessive insulin release) - O2 therapy damages lungs (bronchopulmonary dysplasia) and may cause cataracts (blindness) |
|
|
What are the complications of O2 therapy in Neonatal Atelectasis?
|
- Damages lungs (bronchopulmonary dysplasia)
- Cataracts (blindness) |
|
|
Why does Neonatal Atelectasis cause Hyaline Membranes to form on the alveoli?
|
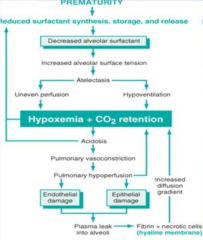
- Prematurity leads to reduced surfactant synthesis, storage, and release
- Causes increased alveolar surface tension - Leads to atelectasis: uneven perfusion and hypoventilation - Causes hypoxemia and CO2 retention - Leads to acidosis, pulmonary vasoconstriction, and pulmonary hypoperfusion - Leads to endothelial and epithelial damage which causes plasma to leak into alveoli - Causes fibrin and necrotic cells to accumulate within alveoli forming a Hyaline Membrane |
|
|
What type of Atelectasis is caused by fibrotic changes in lung or pleura, which prevents full expansion?
|
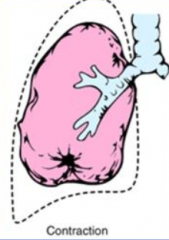
Contraction Atelectasis
|
|
|
What happens in Contraction Atelectasis?
|
- Fibrotic changes in lung parenchyma or pleura
- Prevents full expansion - Not reversible |
|
|
What part of the lung is damaged in Acute Lung injury?
|
Endothelium or Epithelium
|
|
|
Is there a genetic predisposition to Acute Lung injury?
|
- There are both non-heritable and heritable forms
- The response and survival of heritable forms depends on multiple loci on different chromosomes |
|
|
What are the chemical mediators of Acute Lung injury?
|
- Cytokines, oxidants, growth factors
- TNF; IL-1, -6, -10; TGF-β |
|
|
What are the manifestations of Acute Lung injury?
|
- Mild form: pulmonary edema
- Severe form: diffuse alveolar damage (acute respiratory distress syndrome) |
|
|
What are the features of the mild form of Acute Lung Injury?
|
* Pulmonary Edema
- Microvascular or alveolar injury → increase in capillary permeability |
|
|
What causes pulmonary edema in acute lung injury?
|
Alterations in Starling forces:
- ↑ Hydrostatic P in pulmonary capillaries - ↓ Oncotic P |
|
|
What can cause increased hydrostatic pressure in pulmonary capillaries? Outcome?
|
- L sided heart failure
- Volume overload - Mitral stenosis - Hemodynamic disturbances - cardiogenic pulmonary edema Leads to pulmonary edema |
|
|
What can cause decreased oncotic pressure in pulmonary capillaries? Outcome?
|
- Nephrotic syndrome
- Liver cirrhosis Leads to pulmonary edema |
|
|
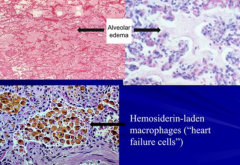
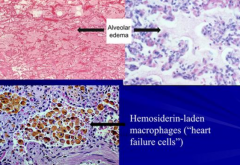
What are the features of pulmonary edema in acute lung injury?
|
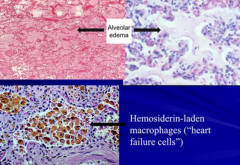
- Transudate (low in proteins)
- Edema fluid accumulation in alveoli w/ heart failure cells and brown induration |
|
|
What can cause increased capillary permeability / pulmonary edema in acute lung injury?
|
Microvascular or Alveolar Injury:
- Infections - Aspiration - Drugs, shock, trauma - High altitude |
|
|
What causes Acute Respiratory Distress Syndrome?
|
Non-cardiogenic pulmonary edema resulting from acute alveolar-capillary damage:
- Direct lung injury - Indirect lung injury (systemic diseases) |
|
|
What are the risks for Acute Respiratory Distress Syndrome?
|
* Gram negative sepsis (40%)
* Gastric Aspiration (30%) * Severe trauma (10%) * Pulmonary infections (diffuse) (these account for >50% of causes) - Heroin - Smoke inhalation |
|
|
What are the clinical findings of Acute Respiratory Distress Syndrome?
|
- Dyspnea
- Severe hypoxemia NOT responsive to O2 therapy - Respiratory acidosis |
|

What does this x-ray show?
|

- White-out appearance (like a snow storm)
- Represents severe and advanced Acute Respiratory Distress Syndrome (ARDS) |
|
|
What is the pathogenesis of Acute Respiratory Distress Syndrome?
|
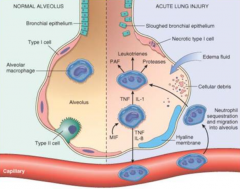
- Acute injury to alveolar epithelium or endothelium
- Alveolar macrophages and other cells release cytokines → neutrophil chemotaxis → transmigration of neutrophils into alveoli → leakage of protein (fibrin) rich exudate → form hyaline membrane - Damage to pneumocytes causes surfactant deficiency leading to atelectasis - Progressive interstitial fibrosis |
|
|
What tries to repair damage in Acute Respiratory Distress Syndrome?
|
Type 2 Pneumocytes
|
|
|
What is the prognosis for Acute Respiratory Distress Syndrome?
|
Poor ~60% mortality rate
|
|
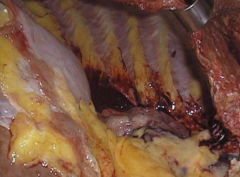
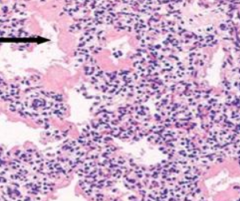
What is seen in this image?
|
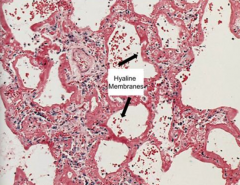
Hyaline Membrane in Acute Respiratory Distress Syndrome
|
|
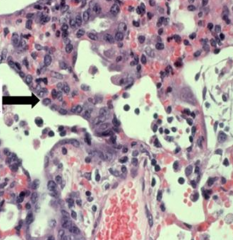
What is seen in this image?
|
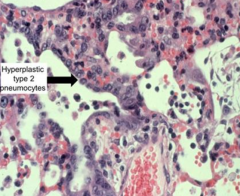
Hyperplastic Type 2 Pneumocytes, trying to repair damage
|
|
|
What are the stages of Acute Respiratory Distress Syndrome? What happens in each stage? Timeline?
|
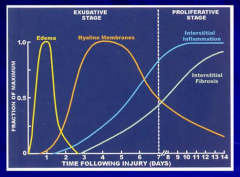
Exudative Stage (days 0-7)
- Edema (peaks day 1) - Hyaline Membrane formation (peaks day 4) Proliferative Stage (days 7-14) - Interstitial Inflammation (peaks day 11) - Interstitial Fibrosis (peaks day 14) - Interstitial inflammation and fibrosis begin during exudative stage |
|
|
Case: 60 yo woman develops pneumonia complicated by septicemia. 3 wks later develops multiple organ failure. Abx led to sputum and blood cultures lacking growth of organisms. Requires intubation w/ mechanical ventilation and becomes more difficult to maintain SaO2. Chest x-ray shows increasing opacifications of all lung fields.
What is the pathologic process most likely to be present in her lungs? |
Diffuse hyaline membrane formation
|

