![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
What is a normal arterial blood gas value for pH?
|
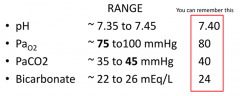
7.4
|
|
|
What is a normal arterial blood gas value for PaO2?
|
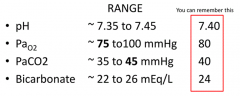
80 mmHg
|
|
|
What is a normal arterial blood gas value for PaCO2
|
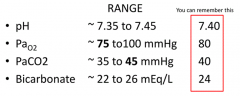
40 mmHg
|
|
|
What is a normal arterial blood gas value for Bicarbonate?
|
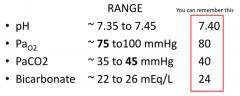
24 mEq/L
|
|
|
What does the term FiO2 stand for? What does this mean clinically?
|
Fraction of Inspired Oxygen
Room air: - 20% of air is O2 → FiO2 = 0.2 Oxygen via nasal cannula: - Increases flow by 1 L/min increments → increases 4% - 1 LPM: FiO2 = 0.24 - 2LPM: FiO2 = 0.28 - Etc. but increase in FiO2 stops at 10 LPM, so FiO2 limit is 50-60% w/ nasal cannula Oxygen via face mask w/ high flow: - FiO2 = 0.8-0.9 Oxygen via face mask + reservoir w/ high flow: - FiO2 = 1.0 |
|
|
How can you give a patient 100% Oxygen (FiO2 = 1.0)?
|
Deliver O2 via face mask + reservoir w/ high flow
|
|
|
What receptors respond to a decrease in PaO2 (<80 mmHg)?
|
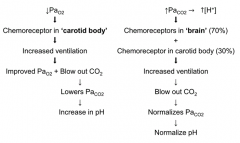
Chemoreceptors in CAROTID BODY
|
|
|
What receptors respond to an increase in PaCO2 (>40 mmHg)?
|
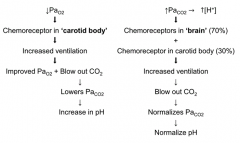
- Chemoreceptors in BRAIN (70%)
- Chemoreceptors in carotid body (30%) |
|
|
What happens when a low PaO2 (<80 mmHg) is detected in the carotid body?
|
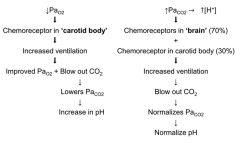
↑ Ventilation
→ Improves PaO2 + Blow out CO2 → Lowers PaCO2 → Increase in pH |
|
|
What happens when a high PaCO2 (>40 mmHg) is detected in the brain and carotid body?
|
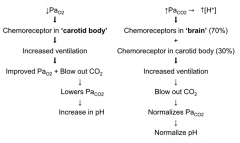
↑ Ventilation
→ Blow out CO2 → Normalizes PaCO2 → Normalizes pH (previously decreased d/t excess CO2) |
|
|
What is the relationship between SaO2 and PO2?
|
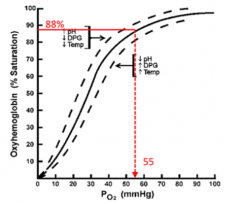
- SaO2 = O2 saturation of Hemoglobin
- PO2 = O2 pressure in mmHg - Sigmoidal curve - At 88% saturation, PO2 is 55 mmHg (normal is 80 mmHg) |
|
|
What are the signs and symptoms of hypercapnia (>40 mmHg)?
|
- Morning headaches
- Confusion - Lethargy / drowsiness / sleepiness - Flushed skin - Rapid breathing - Tremors (flapping) |
|
|
What is the role of the Carotid Body chemoreceptors?
|
* Sense dissolved O2 in blood (PaO2)
* Respond to PaO2 < 75 mmHg - Sense ↑ [H+] / elevated PaCO2 (30% of response) |
|
|
What is Oxygen Content?
|
O2 bound to Hb + O2 dissolved in plasma (PaO2)
|
|
|
What are Carotid Body chemoreceptors UNABLE to detect?
|
- Not sensitive to changes in Hemoglobin levels or if Hemoglobin has lost its capacity to carry O2
- Therefore, not sensitive to anemia or CO poisoning *Only detects ↓PaO2 <75 mmHg (and contribute to resposnse to hypercapnia/↑[H+] |
|
|
What is the role of the Central chemoreceptors?
|
- Respond to ↑[H+] / ↑PaCO2
- Responsible for ~70% of increased ventilation in response to hypercapnia |
|
|
What is increased PaCO2 (hypercapnia) responsible for?
|
Main cause of increased Tidal Volume and increased respiratory rate under normal conditions
|
|
|
What can cause PaCO2 to rise?
|
- Increasing oxygenation decreases CO2 carrying capacity of Hemoglobin
- Removal of hypoxemic vasconstriction in lungs, shunts blood to areas where CO2 exchange cannot take place - Removal of hypoxemic respiratory drive |
|
|
What happens if you have bilateral carotid artery resection?
|
* Almost complete loss of ventilatory response to hypoxia (↓PaO2) (may be some chemoreceptors in aortic bodies?)
- Partial loss (30%) of ventilatory response to hypercapnia (↑PaCO2) (causes PaCO2 to rise 2-4 mmHg (or more in COPD) |
|
|
What happens in COPD with CO2 retention?
|
- Theoretically, w/ CO2 retention, the respiratory drive from hypercapnia is diminished
- They must rely on hypoxemic respiratory drive to breathe faster |
|
|
What should you do for a patient w/ COPD and hypoxia?
|
- Correct hypoxia to a level that supplies enough O2 to the brain (O2 sats >88% sufficient = PaO2 of 55mmHg)
- Do not hold O2 just because CO2 will go up, O2 is essential for life - DO NOT GIVE EXTRA O2 just to make saturations increase to 100%; this does not improve O2 content of blood |
|
|
What causes the rise in PaCO2 in COPD?
|
- Loss of hypoxemic drive (responsible for 10-20% of level of PaCO2)
- Increasing O2 flow to these patients causes O2 to displace sites on Hb, preventing CO2 from leaving blood (30-40%) - Ventilation perfusion mismatch (40-50%) |
|
|
What O2 pressure and saturation should you target?
|
PaO2: 55 mmHg
O2 Sat: 88% If you try to go higher than this you can increase PaCO2; 88% saturation is high enough because this corresponds to the horizontal part of the hemoglobin dissociation curve |
|
|
How do O2 and CO2 affect partial pressures?
|
O2 and CO2 bound to hemoglobin do not contribute to partial pressures, only the free O2 and CO2 contribute to PaO2 and PaCO2
|
|
|
Where are the pulmonary receptors?
|
- In lung parenchyma (via vagus)
- In chest wall |
|
|
What kind of receptors are found in the lung parenchyma?
|
- Slowly adapting receptors
- Rapidly adapting receptors - Juxtacapillary receptors |
|
|
What are the features of the slowly adapting receptors?
|
- Found in lung parenchyma (airway smooth muscle)
- Detects increases in lung volume --> sends signal via vagus to inhibit further inspiration = Hering-Breuer Reflex - Ultimately, prevents over-inflation of lungs |
|
|
What are the features of the rapidly adapting receptors?
|
- Found in lung parenchyma (carina)
- Irritant receptors - very sensitive to chemical stimuli - Communicate via vagus nerve |
|
|
What are the features of the juxtacapillary receptors?
|
- Found in lung parenchyma (next to capillaries)
- Innervated by vagus |
|
|
What kind of pulmonary receptors are found in the chest wall?
|
- Muscle Spindles
- Tendon Organs |
|
|
What happens in Pickwickian Syndrome?
|
- Obesity Hyperventilation Syndrome
- Depressed hypercapnic and hypoxic drive - They have lower tidal volume when compared to person of same height and weight who does not have elevated PO2 |
|
|
Case: 24 yo female w/ chronic iron deficiency anemia is admitted for a blood transfusion. Her hemoglobin is 4.0 g/dL. She has no respiratory distress. The resident orders an ABG.
What is the expected pH? paO2? paCO2? |
All should be normal:
- pH: 7.4 - PaO2: 100 mmHg - PaCO2: 40 mmHg |
|
|
How can neuromuscular disease affect respiration?
|
Can cause respiratory failure d/t muscle weakness (of the inspiratory and expiratory muscles)
|
|
|
What change in vital capacity and maximum inspiratory force indicates the start of respiratory failure?
|
- Vital capacity falls to <55% of predicted value
- Maximum inspiratory force falls to <30% of predicted value |
|
|
What are the different patterns of breathing?
|
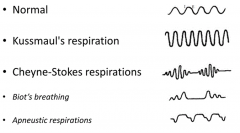
- Normal
- Kussmaul's respirations - Cheyne-Stokes respirations - Biot's breathing - Apneustic respirations |
|
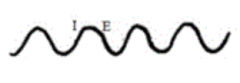
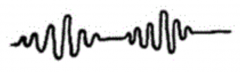
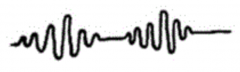
What kind of breathing is this?
|
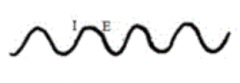
Normal
|
|
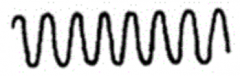
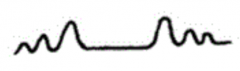
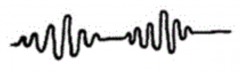
What kind of breathing is this? Characteristics?
|
Kussmaul's Respirations:
- Consistently deep and rapid respirations - Severe metabolic acidosis (eg, diabetic ketoacidosis) |
|
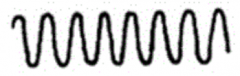
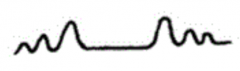
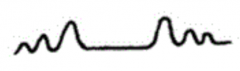
What kind of breathing is this? Characteristics?
|
Cheyne-Stokes Respirations:
- Tidal volume starts shallow - Gets progressively deeper (crescendo) - Then gets progressively shallower (decrescendo) - Caused by heart failure, strokes, traumatic brain injuries, brain tumors, or first-time high altitude sickness |
|
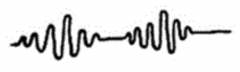
What kind of breathing is this?
|
Biot's Breathing:
- Periods or clusters of rapid respirations of near equal depth or VT - Followed by regular periods of apnea - Caused by damage to medulla oblongata (stroke (CVA), trauma, uncal or tentorial herniation) |
|

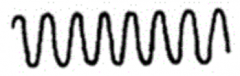
What kind of breathing is this? Characteristics?
|

Apneustic Respirations:
- Prolonged inspiratory phase - Followed by a prolonged expiratory phase - Caused by damage to upper part of pons |
|
|
Which kind of respirations are associated with severe metabolic acidosis?
|
Kussmaul's Respirations:
- Consistently deep and rapid respirations |
|
|
Which kind of respirations are caused by heart failure, strokes, traumatic brain injuries, brain tumors, and first-time high altitude sickness?
|
Cheyne-Stokes Respirations:
- Tidal volume starts shallow - Gets progressively deeper (crescendo) - Then gets progressively shallower (decrescendo) |
|
|
What are the pre-requisites for Cheyne-Stokes Respirations?
|
- Increased gain
- Increased circulation time - Changing state of alertness |
|
|
Which kind of respirations are caused by damage to the upper part of the pons?
|

Apneustic Respirations
- Prolonged inspiratory phase - Followed by a prolonged expiratory phase - Caused by damage to upper part of pons |
|
|
Which kind of respirations are caused by damage to medulla oblongata such as a stroke (CVA), trauma, or an uncal or tentorial herniation)?
|
Biot's Breathing:
- Periods or clusters of rapid respirations of near equal depth or VT - Followed by regular periods of apnea |
|
|
What are chemoreceptor neurons?
|
- Neurons whose discharge rate is altered by changes in PO2 or PCO2 in their environment
- Respiratory chemoreceptors are neurons that alter breathing |
|
|
What is the location of O2 chemoreceptors?
|
Carotid Body (also slightly activated by hypercapnia)
|
|
|
What innervates the carotid body?
|
- Sensory fibers originating from the petrosal ganglion
- Fibers travel through the carotid sinus nerve (a branch of CN IX) |
|
|
Where is carotid body activity processed?
|
- Initially processed in the Nucleus Tractus Solitarius (NTS) which projects to multiple sites in brainstem
- Carotid sensory mechanism is within glomus cells |
|
|
What happens in the carotid sensory mechanism?
|
- Occurs in glomus cells
- Changes in conductance of K+ channels - Changes in intracellular Ca2+ → liberates hormones like serotonin and/or ACh → diffuse to nerve endings → initiate changes in discharge frequency |
|
|
How do PaO2 and PaCO2 interact in the carotid chemoreceptors? What is their impact on impulse frequency in the carotid sinus nerve?
|

- As PaO2 ↓, impulse frequency ↑ (non-linear relationship)
- As PaCO2 ↑, impulse frequency ↑ (linear relationship) |
|
|
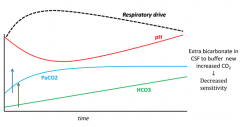
What is the effect of surgically denervating the carotid chemoreceptors on resting PaCO2 and CO2 sensitivity?
|
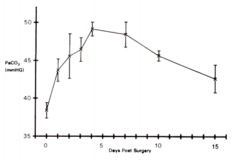
- Results in transient hypoventilation and attenuation of CO2 sensitivity
- After 5 days, recovery from initial effects begins - Graph: PaCO2 increases initially (carotid chemoreceptors responsible for 1/3 response to hypercapnia), and at 5 days starts to recover to return levels to normal |
|
|
What is the relationship between PaCO2 and ventilation rate? Effect of stimulation of carotid body?
|
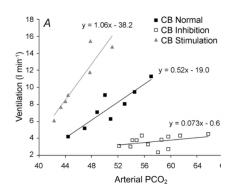
- As PaCO2 increases, so does ventilatory rate
- With CB stimulation, there was a greater increase in RR / change in PaCO2 - With CB inhibition, there was almost no change in RR / change in PaCO2 |
|
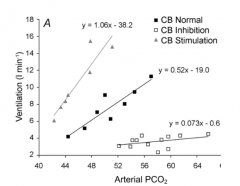
What does this graph tell us?
|
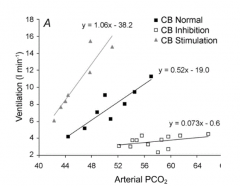
Ventilatory intracranial chemoreflex is directly related to the level of carotid chemoreceptor activity
- With CB stimulation, there was a greater increase in RR / change in PaCO2 - With CB inhibition, there was almost no change in RR / change in PaCO2 |
|
|
What are the sites of the respiratory chemoreceptors (affect breathing)?
|
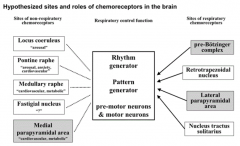
- Pre-Bötzinger Complex
- Retrotrapezoidal Nucleus - Lateral Parapyramidal Area - Nucleus Tractus Solitarius |
|
|
What are the respiratory control functions?
|
- Rhythm generator
- Pattern generator - Pre-motor neurons and motor neurons |
|
|
What are the sites of non-respiratory chemoreceptors (affect other physiologic functions)? Functions?
|
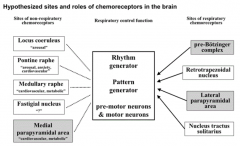
- Locus Ceruleus (arousal)
- Pontine Raphe (arousal, anxiety, CV) - Medullary Raphe (CV, metabolic) - Fastigial Nucleus (?) - Medial Parapyramidal Area (CV, metabolic) |
|
|
The dogma says that the primary drive for breathing is from what? Why?
|
CO2 chemoreceptors
- Small changes in PaCO2 have much larger effect on breathing than small changes in PaO2 |
|
|
What is the major fast-acting neurotransmitter? Function?
|
Glutamate - excitatory to post-synaptic neurons and leads to depolarization
|
|
|
What is the action of neuromodulators (as opposed to neurotransmitters)
|
- Bind to post-synaptic receptors to change the membrane potential to increase or decrease the possibility of eliciting discharge
- Some act as ionotropic receptors and others act as G-protein coupled receptors that initiate a cascade of events that change the excitability of the neurons |
|
|
What are the major excitatory neuromodulators?
|
- Serotonin
- ACh - Substance P - NE - Orexin |
|
|
What are the major inhibitory neuromodulators?
|
- GABA
- Glycine |

