![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
89 Cards in this Set
- Front
- Back
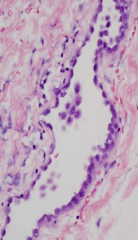
What does this image show?
|
Normal Pleura - flat/squamous to cuboidal epithelium "mesothelium" that covers the pleural surface
|
|
|
What are the layers of pleura surrounding the lungs?
|
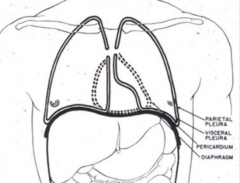
- Visceral pleura
- Parietal pleura - Separated by pleural space |
|
|
What is the definition of a pleural effusion?
|
Accumulation of fluid >15 ml in pleural space
|
|
|
What can cause a pleural effusion?
|
- ↑ Hydrostatic pressure
- ↓ Osmotic pressure - ↑ Vascular permeability |
|
|
What can cause ↑ hydrostatic pressure, leading to a pleural effusion?
|
- CHF
- Lymphatic blockage d/t tumor |
|
|
What can cause ↓ osmotic pressure, leading to a pleural effusion?
|
- Nephrotic syndrome
- Chronic liver disease (not making enough proteins) |
|
|
What can cause ↑ vascular permeability, leading to a pleural effusion?
|
Pneumonia
|
|
|
What are the clinical manifestations of a pleural effusion?
|
- Dyspnea
- Pleuritic pain - Cough - Respiratory distress d/t atelectasis |
|
|
What causes pleuritic pain?
|
Visceral and parietal pleural layers rubbing against each other causes pain on deep inspiration
|
|
|
What are the physical exam findings of pleural effusion?
|
Enlarged Hemithorax:
- Dullness on percussion that side - Decreased or absent breath sounds on that side |
|
|
What does compression of the lung in pleural effusion cause?
|
Atelectasis which leads to respiratory distress
|
|
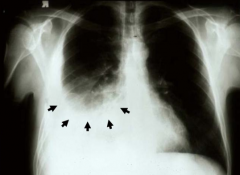
What does this image show?
|
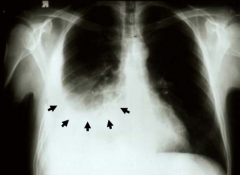
Pleural Effusion
- Fluid accumulates at bottom of lung - Looks opacified d/t fluid collection in pleural space - Blunting of costophrenic angle (where the diaphragm meets the ribs) |
|
|
How do you clinically manage a patient with Pleural Effusion?
|
- Chest x-ray to confirm diagnosis
- Thoracentesis to determine what kind of fluid is in there and therapeutic to remove fluid - Analyze pleural fluid (chemistry, culture, cytology) - Pleural biopsy (percutaneous or open) - Treat underlying cause |
|
|
How do you analyze the pleural fluid removed by thoracentesis?
|
- Chemistry
- Culture (look for infection) - Cytology (look for malignant cells, indicative of neoplasm) |
|
|
What do you need to do if the pleural fluid analysis removed by thoracentesis is not indicative of the cause of the Pleural Effusion?
|
Pleural Biopsy either percutaneously or by opening patient up to get a larger section of tissue (uncommon)
|
|
|
What are the common causes of Pleural Effusion?
|
- Infections
- PE - Malignant neoplasm - Trauma - Systemic condition |
|
|
What kinds of infections are more commonly associated with Pleural Effusion?
|
- Bacterial Pneumonia
- Viral disease - Tuberculosis |
|
|
What are the systemic conditions that can cause Pleural Effusion?
|
- CHF
- Cirrhosis - Nephrotic syndrome - Collagen vascular diseases (eg, lupus, RA) |
|
|
What are the types of Pleural Effusion?
|
- Inflammatory Pleural Effusions
- Non-inflammatory Pleural Effusions |
|
|
What are the Inflammatory types of Pleural Effusion?
|
- Serofibrinous (contains lots of fibrin)
- Suppurative (empyema, contains lots of pus) - Hemorrhagic (contains blood) |
|
|
What are the Non-Inflammatory types of Pleural Effusion?
|
- Hydrothorax (serous fluid)
- Hemothorax (blood) - Chylothorax (lymphatic fluid) |
|
What are the causes of Serofibrinous Pleural Effusion?
|
Inflammatory conditions such as:
- Pneumonia - TB - Lung infarcts - Abscesses |
|
|
What are the causes of Suppurative Pleural Effusion / Empyema?
|
Inflammatory conditions causing localized accumulation of pus d/t organisms:
- Pneumococci - Staphilococci - Streptococci |
|
|
What are the causes of Hemorrhagic Pleuritis?
|
- Coagulopathies
- Rickettsial disease - Malignant neoplasms |
|
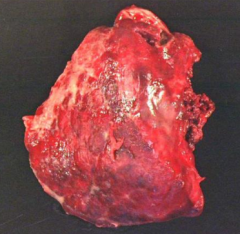
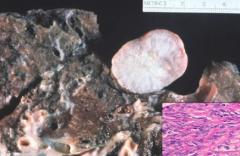
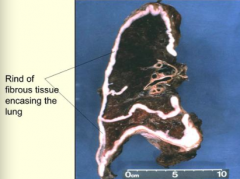
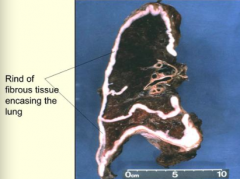
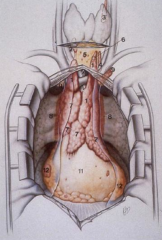
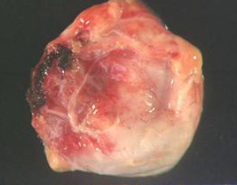
What does this image show?
|
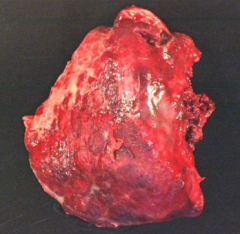
Fibrinous Pleuritis / Serofibrinous Inflammatory Pleural Effusion:
- Upper half is covered in thick, white exudative process described as "shagginess" - Pleural adhesion in middle would be responsible for lung sticking to chest wall |
|
|
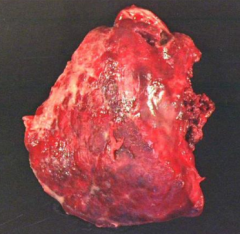
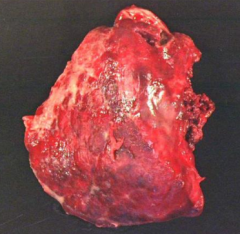
What does Empyema / Suppurative Pleural Effusion look like?
|
- Pleural surface is coated by shaggy thick fibrin layer admixed w/ greenish purulent exudate
- Produces adhesions and circumscribed pus which limits lung expansion causing atelectasis |
|
|
How do you treat Empyema / Suppurative Pleural Effusion?
|
Surgical decortication (open up chest and remove pus)
|
|

What kind of pleural fluid from a non-inflammatory Pleural Effusion would look like this? Cause?
|

Hydrothorax:
- Clear serous fluid - Caused by CHF, pulmonary congestion and edema, cirrhosis, uremia, renal failure |
|

What kind of pleural fluid from a non-inflammatory Pleural Effusion would look like this? Cause?
|

Hemothorax:
- Hemorrhagic fluid - Caused by ruptured aortic aneurysm, trauma, etc |
|

What kind of pleural fluid from a non-inflammatory Pleural Effusion would look like this? Cause?
|

Chylothorax:
- Milky fluid - Caused by thoracic duct trauma or lymphatic occlusion secondary to malignancy |
|
|
What happens in a Pneumothorax?
|
Presence of air or gas within the pleural cavity
|
|
|
What causes a Pneumothorax? What is it associated with?
|
- Spontaneous
- Traumatic - Therapeutic - Commonly associated w/ emphysema, asthma, and TB |
|
|
Who gets and what causes a Spontaneous Idiopathic Pneumothorax?
|
*Young individuals (usually males) secondary to rupture of small apical lung blebs (especially in apical region)
|
|
|
What happens in Spontaneous Idiopathic Pneumothorax?
|
Usually subsides spontaneously
|
|
|
What happens in Tension Pneumothorax?
|
- Defect acts as a flap/valve
- Permits entrance of air during inspiration - Does not allow escape of air during expiration - Leads to contralateral deviation of trachea |
|
|
What are the mechanisms that cause Pneumothorax?
|
- Perforation of visceral pleura and entry of air from lung into pleural space
- Penetration of air from chest wall, diaphragm, mediastinum, or esophagus into pleural space - Gas forming organism in empyema (inflammatory pleural effusion) |
|
|
What are the symptoms of Pneumothorax?
|
- Chest pain
- Dypsnea - Absent breath sounds on auscultation - Tympanitic percussion (hyper-resonance) - Contralateral deviation of trachea on CXR - Compression and collapse of lung parenchyma w/ atelectasis - Marked respiratory distress |
|
|
What can cause Spontaneous Pneumothorax?
|
- Idiopathic
- Secondary to rupture of pleural bleb or bulla - Bronchopleural fistula (between airway and pleural space) - Bullous emphysema |
|
|
What can cause Tension Pneumothorax?
|
Penetrating trauma to lungs
- Flap-like pleural defect acts like valve to let air in and not out |
|
|
What are the symptoms of Tension Pneumothorax?
|
- Increased pleural cavity pressure w/ compression and atelectasis of lung
- Sudden onset of respiratory distress (medical emergency) - Trachea deviates to contralateral side of pneumothorax |
|
|
What are the types of pleural neoplasms?
|
Benign:
- Solitary fibrous tumor (pleural fibroma) Malignant: - Metastases from other organs - Malignant mesothelioma |
|
|
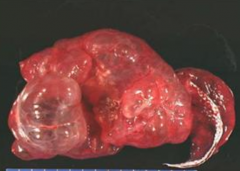
What is the benign neoplasm of the pleura? What does it look like?
|
Solitary Fibrous Tumor (Pleural Fibroma):
- Polypoid - Well-circumscribed - Pedunculated |
|
|
What does a Solitary Fibrous Tumor (Pleural Fibroma) consist of?
|
Fibroblasts w/ abundant collagenized stroma
|
|
|
How do you diagnose and treat Solitary Fibrous Tumor (Pleural Fibroma)?
|
- Usually discovered incidentally on chest x-ray
- Mostly asymptomatic - Cured by simple excision |
|
|
What symptoms is Solitary Fibrous Tumor (Pleural Fibroma) associated with?
|
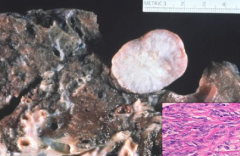
- Mostly asymptomatic
- Associated with hypoglycemia and clubbing of the fingers |
|
|
What is the name of the malignant pleural neoplasm (not a metastasis)?
|
Malignant Mesothelioma
- Proliferation of mesothelial cells lining serosal surfaces |
|
|
How common is Malignant Mesothelioma? When are you more likely to get it?
|
- Affects 15-20 people / million / year in general population
- More common in adults over 50 - More common in those w/ occupational exposure to Asbestos: millworkers, roofing materials, textiles, insulation, shipyard workers |
|
|
What are the most common causes of Malignant Mesothelioma?
|
** Asbestos exposure
- Radiation - Chronic inflammation - Viral infections (SV40 simian virus in old polio vaccines) - Up to 50% are idiopathic |
|
|
If you have a history of heavy exposure to Asbestos what are you at increased risk for?
|
Malignant Mesothelioma (up to 10% lifetime risk)
|
|
|
Why is Malignant Mesothelioma more common in adults > 50 yo?
|
Asbestos exposure has a long latency period (20-40 years)
|
|
|
What do Asbestos fibers look like?
|
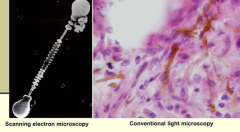
- LM: brown dumbbells
- EM: dumbbell shape with linear striations in middle |
|
|
What are the clinical symptoms of Malignant Mesothelioma?
|
- Insidious, slow growing neoplasm
- Recurrent pleural effusions - Chest pain and dyspnea in more advanced stages - 20% have pulmonary fibrosis (asbestosis) |
|
|
What is the prognosis of Malignant Mesothelioma once it is detected?
|
Fatal malignancy; median survival 18 months
|
|
|
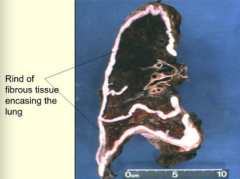
How does Malignant Mesothelioma spread?
|
Along mesothelial surfaces; it does not project into the lung
|
|
|
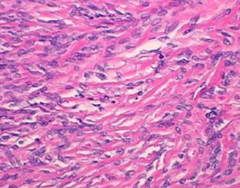
What is Malignant Mesothelioma composed of? How does this affect diagnosis?
|
- Composed of bland-appearing cuboidal cells that resemble normal mesothelial cells (well-differentiated neoplasm)
- Very difficult to distinguish Malignant Mesothelioma from metastatic carcinoma to pleura |
|
|
What other serosal surfaces can Malignant Mesothelioma affect?
|
- Peritoneum
- Tunica vaginalis - Pericardium |
|
|
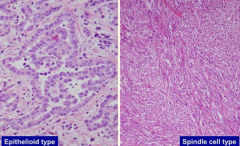
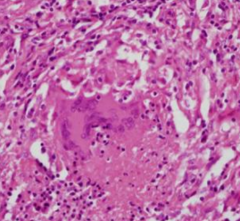
What are the types of Malignant Mesothelioma based on histology?
|
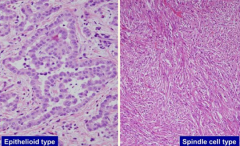
- Epithelioid type: cells resemble cuboidal epithelium but has nested appearance
- Spindle Cell type: doesn't resemble epithelium, has a sarcomatous appearance, much more malignant |
|
|
What are the most common tumors in the pleura?
|
Metastatic tumors most commonly from:
* Lung - Breast, ovarian, pancreas, kidney |
|
|
How do metastases get to the pleura?
|
Spread by blood, lymphatics, or direct extension
|
|
|
What do metastatic tumors to the pleura look like?
|

Multiple and bilateral (whereas Malignant Mesothelioma is usually unilateral)
|
|
|
If pleural tumors are bilateral what should you think of? Unilateral?
|
- Bilateral: metastatic tumors
- Unilateral: Malignant Mesothelioma |
|
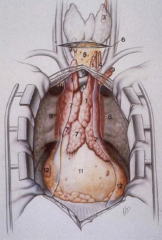
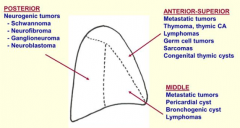
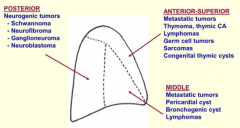
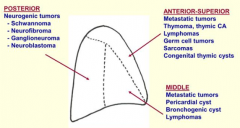
What are the compartments of the mediastinum?
|
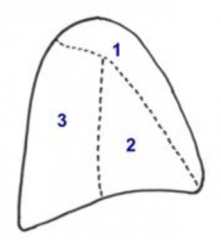
- Anterior / superior (1)
- Middle (2) - Posterior (3) |
|
What pathology affects the mediastinum?
|
- Inflammation
- Congenital / developmental malformations - Neoplasms |
|
|
What kind of inflammatory conditions can affect the mediastinum?
|
- Acute Mediastinitis
- Granulomatous Mediastinitis - Idiopathic Sclerosing Mediastinitis |
|
|
What causes Acute Mediastinitis?
|
Complication of conditions affecting neighboring organs (eg, esophageal perforation, perforation of lung abscess, sternal osteomyelitis, etc)
|
|
|
What causes Granulomatous Mediastinitis?
|
Chronic disorder secondary to fungal or mycobacterial infection:
- Histoplasmosis - Tuberculosis - Cryptococcosis - Atypical mycobacteria - Aspergillosis |
|
|
What causes Idiopathic Sclerosing Mediastinitis?
|
Unknown etiology
|
|
|
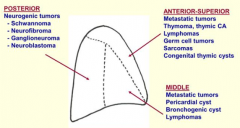
What tumors affect the anterior-superior mediastinum?
|
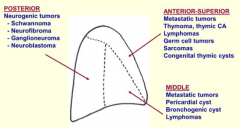
- Metastatic tumors
- Thymoma, thymic cancer - Lymphomas - Germ cell tumors - Sarcomas - Congenital thymic cysts |
|
|
What tumors affect the middle mediastinum?
|
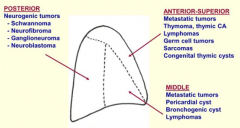
- Metastatic tumors
- Pericardial cysts - Bronchogenic cysts - Lymphomas |
|
|
What tumors affect the posterior mediastinum?
|
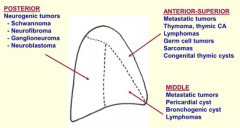
Neurogenic tumors:
- Schwannoma - Neurofibroma - Galnglioneuroma - Neuroblastoma |
|
|
Which part of the mediastinum is affected by:
- Metastatic tumors - Pericardial cysts - Bronchogenic cysts - Lymphomas |
Middle Mediastinum
|
|
|
Which part of the mediastinum is affected by:
Neurogenic tumors: - Schwannoma - Neurofibroma - Galnglioneuroma - Neuroblastoma |
Posterior Mediastinum
|
|
|
Which part of the mediastinum is affected by:
- Metastatic tumors - Thymoma, thymic cancer - Lymphomas - Germ cell tumors - Sarcomas - Congenital thymic cysts |
Anterior-Superior Mediastinum
|
|
|
What do congenital cysts look like? Where are they found?
|

- Usually unilocular
- Lined by simple cuboidal epithelium - May be filled w/ serous fluid - Found on anterior-superior mediastinum (that have spread from thymus) |
|
|
Who is most likely to get a congenital cyst?
|
Children aged 5-15 years
|
|
|
What is Thymic Hyperplasia associated with? What part of the mediastinum can be affected by it?
|
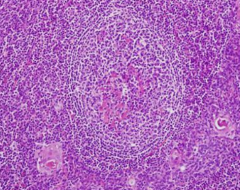
- Thymic lymphoid follicular hyperplasia (large middle structure)
- Anterior-Superior Mediastinum |
|
|
Who is most likely to get Thymic Hyperplasia?
|
Associated w/ Myasthenia Gravis and other Auto-Immune disorders
|
|
|
What is Myasthenia Gravis?
|
Autoimmune disease:
- Auto-antibodies form to ACh receptor in neuromuscular junction - Autosensitization to AChR is initiated in thymus d/t defective confrontation of ACh secreting thymic myoic cells w/ T-cells |
|
|
What are the symptoms of Myasthenia Gravis?
|
- Muscular weakness
- Fatigability - Ptosis - Diplopia |
|
|
What is Myasthenia Gravis associated with?
|
Thymic lesions:
- Thymic hyperplasia - Thymoma (30-40% of patients w/ thymoma develop MG) - Thymic carcinoma |
|
|
What the primary thymic epithelial neoplasms? Where can they spread?
|
- Thymoma
- Thymic carcinoma - Can metastasize to anterior-superior mediastinum |
|
|
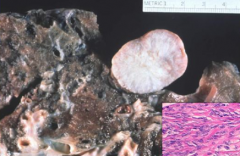
What is a thymoma?
|

- Primary thymic epithelial neoplasm
- Proliferation of thymic epithelial cells |
|
|
What does a thymoma contain?
|
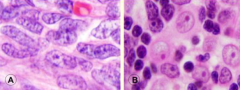
- Thymic epithelial cells (neoplastic proliferation)
- Abundant immature T-cells (non-neoplastic) - Composed of: spindle cells (A) or round epithelioid cells (B) or both |
|
|
What is thymoma associated with?
|
- Myasthenia Gravis
- Other paraneoplastic syndromes |
|
|
What is the prognosis if Thymoma?
|
- Slow growing tumor that may recur but rarely metastasizes
- Encapsulated tumors are cured by complete surgical excision - Invasive tumors tend to recur repeatedly and may eventually metastasize - Recurrent tumors may progress to thymic carcinoma |
|
|
What are the symptoms of Thymoma?
|
- Asymptomatic in 30%
- Cough, dyspnea, chest pain - Superior vena cava syndrome - Paraneoplastic syndromes |
|
|
What are the paraneoplastic syndrome associated with Thymoma?
|
- Myasthenia gravis
- Pure red cell aplasia - Hypogammaglobulinemia - Agranulocytosis (WBC aplasia) - Polymyositis; SLE - Pemphigus vulgaris, disseminated herpes |
|
|
What does thymic carcinoma look like histologically?
|
- Resembles other types of carcinoma occurring in other organs (squamous, small cell, adenocarcinoma, etc)
- No specific features permit definite histologic diagnosis |
|
|
When can you diagnose Thymic Carcinoma?
|
Diagnosis of exclusion:
- Must rule out other explanations before you can say it is Thymic Carcinoma - No specific features permit definite histologic diagnosis |

