![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
97 Cards in this Set
- Front
- Back
|
What is the anatomical location of the Pancreas?
|
Retroperitoneal
**except the tail |
|
|
80-85% of the glands in the Pancreas are __1__ cells organized into acini that drain into the __2__
|
1. Secretory
2. Duct of Wirsung = Main pancreatic duct |
|
|
The Duct of Wirsung normally drains into the __1__ just proximal to the __2__, but may enter the duodenum directly
|
1. Common Bile Duct
2. Ampulla of Vater |
|
|
What will a gallstone stuck at the Ampulla of Vater normally cause?
|
reflux of bile into the pancreatic duct
|
|
|
2 important enzymes that are detectable in the serum after Pancreatic damage
|
1. Lipase
2. Amylase |
|
|
Stimulation of this nerve increases the Pancreatic excretion
|
Vagus nerve
|
|
|
What 2 things stimulate the release of Cholecystokinin?
What causes the release of Secretin? |
Presence of Amino acids and pH < 3 -> Cholecystokinin -> stimulates pancreas to release digestive enyzmes from Acinar cells
Stomach distension -> Secretin -> stimulates pancreas to release Bicarbonate and Water from Ductal cells |
|
|
What do most cancer of the Pancreas arise from?
|
Pancreatic Ducts (Ductal Adenocarcinoma)
|
|
|
Pancreatitis: __1__ inflammatory condition of the __2__ pancreas that results from cellular injury to __3__ cells
|
1. Reversible
2. Exocrine 3. acinar |
|
|
Describe how a person would present with Acute/Chronic Pancreatitis
|
Severe, boring Mid-Epigastric and LUQ abdominal pain radiating to the back
|
|
|
What are the 2 most common causes of Acute Pancreatitis?
|
1. Alcohol (6 times more common in MEN)
2. Gallstones (3 times more common in women) |
|
|
List 5 complications of Acute Inflammation of the Pancreas
|
1. Shock = pancreatic enzymes eating through the Splenic Artery
2. Peritonitis 3. Hypocalcemia = Ca+ soaps formed during fat necrosis 4. Malabsorption 5. Pseudocyst formation |
|
|
What are the 2 elevated lab findings in Pancreatitis? Which one is elevated first? Which one is more specific for Pancreatitis?
|
Amylase and Lipase
First: Amylase Specific: Lipase |
|
|
What can Hypocalcemia result in?
What is the cause of Hypocalcemia? |
Tetani and seizures
Saponification reaction (Ca+ reacting with Fatty acids) in Acute Hemorrhagic Pancreatitis Fat Necrosis |
|
|
What is Chronic Pancreatitis associated with? (3)
|
Alcohol ingestion
Hemochromatosis Cystic Fibrosis |
|
|
What are 3 complications of Chronic Pancreatitis?
|
1. Pseudocyst formation
2. Malabsorption (Vitamin B12 deficiency) 3. Diabetes |
|
|
Cystic Fibrosis:
-lack of __1__ secretion is linked to impaired secretion of __2__, resulting in unusually viscid secretions -__3__ of the Pancreas ensues, with resultant __4__ and failure to thrive -death is almost always due to __5__ complications |
1. chloride
2. sodium and water 3. Atrophy 4. malabsorption 5. pulmonary |
|
|
Islet cells that secrete Glucagon
|
Alpha cells
|
|
|
Islet cells that secrete Insulin
|
Beta cells
|
|
|
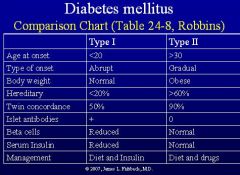
What groups of people is Type I Diabetes Mellitus most common in?
Races less common in |
Northern Europeans
Asians, African-Americans, & Native Americans |
|
|
When has Type I DM been noticed to increase in incidence in several studies?
|
Late fall and early winter
|
|
|
What HLA do 95% of Type I DM patients express?
|
DR3 or DR4
**compared to only 20% of the population expressing these HLAs |
|
|
__1__ antibodies are detectable in most Type I diabetics, but likely represents a __2__ response to proteins released by destruction of beta cells by __3__
|
1. Beta cells
2. humoral 3. T lymphocytes |
|
|
Seasonal variation of Type I DM in incidence suggests ______ as a possible cause of the abnormal immune response to beta cells
|
Viral infections
|
|
|
What are the 2 major risk factors for Type I DM?
|
1. immediate family member with Type 1 DM
2. Caucasians are at a greater risk than other ethnic groups |
|
|
What is the pathology seen in Type I DM?
|
1. Insulitis = inflammation of the islet
2. Beta cell depletion 3. Diffuse fibrosis of the pancreas |
|
|
Most of the pathology seen in Diabetes Type I is due to the __1__, which are thought to be related to the long-term deleterious effects of __2__
|
1. complications
2. Hyperglycemia |
|
|
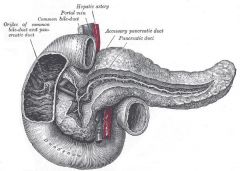
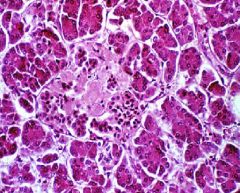
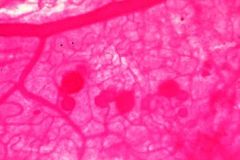
Normal Pancreas
-ducts are within fibrous septa -Islets of Langerhans |
What is this picture showing?
|
|
|
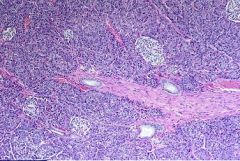
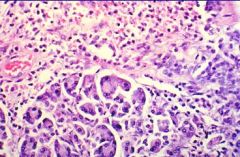
Normal Pancreas histology
-Acini of the Exocrine pancreas |
What is this showing?
|
|
|
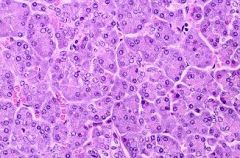
Isle of Langerhans
|
What is this showing?
|
|
|
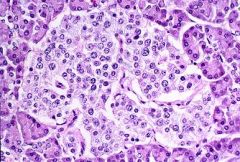
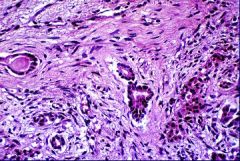
Acute Edematous Pancreatitis
-edema and inflammatory infiltrate |
What is this showing?
|
|
|
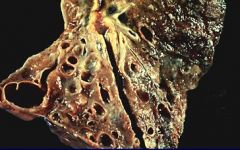
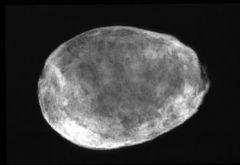
Pancreatic Pseudocyst from Acute Pancreatitis
Splenic Artery bleeding into the pseudocyst |
What can be seen here?
What could cause it to pulsate? |
|
|
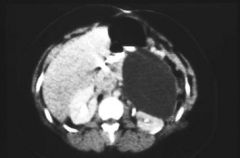
Pancreatic Pseudocyst
|

What is seen here?
|
|
|
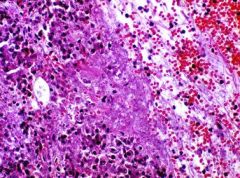
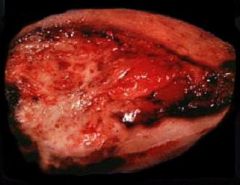
Hemorrhagic Pancreatitis
|

What can be seen here?
|
|
|
Hemorrhagic Pancreatitis
|
What is shown here?
|
|
|
Fat Necrosis with formation of calcium-fatty soaps
|
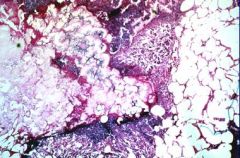
What is this showing?
|
|
|
Chronic Pancreatitis with punctate calcifications
|

What is shown here?
|
|
|
Chronic Pancreatitis
|

What is shown here?
|
|
|
Chronic Pancreatitis
|

What is shown here?
|
|
|
Chronic Pancreatitis
Absence of acinar structures & replacement by pink collagen = FIBROSIS |
What is this showing? How do you know?
|
|
|
Cystic Fibrosis, P. aeruginosa, & Bronchiectasis
|
What are the 3 associations here?
|
|
|
Cystic Fibrosis in the Pancreas
-ducts are dilated, with fibrosis surrounding them |
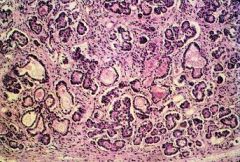
What is this showing?
|
|
|
Alpha cells = Glucagon
Beta cells = Insulin |
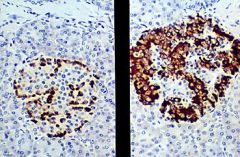
What cells are on the left & what do they secrete?
What cells are on the right & what do they secrete? |
|
|
Type I Diabetes Mellitus = Insulitis
|
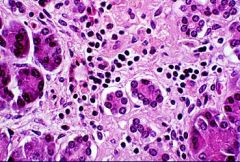
What is shown here?
|
|
|
What are 7 risk factors for Type II Diabetes?
|
1. Obesity
2. Age (generally >30) 3. family history of diabetes 4. lack of regular exercise 5. high BP &/or high conc. of fats in blood 6. history of gestational diabetes or giving birth to a baby weighing > 9 lbs. 7. Blacks, Hispanic, N. Americans, & Asian-Americans |
|
|
Describe the pathogenesis of Type II Diabetes (Non-Insulin Dependent)
|
-Genetically programmed failure of Beta cells to compensate for peripheral insulin resistance
-Multifactorial inheritance -Altered Beta cell function -Insulin resistance = may have increased amounts of Insulin, but decreased # receptors (or non-responsive) |
|
|
Describe the pancreatic pathology of Type II Diabetes
|
-No reduction in Beta cells
- May have increased islet fibrosis or Amyloidosis |
|
|
What is the stain for Amyloid?
|
Congo Red stain
|
|
|
Type II Diabetes with Amyloid infiltration of the Islet
|
What is shown here?
|
|
|
What are the treatments for Type II Diabetes?
|
1. Diet
2. Weight loss and exercise 3. Hypoglycemic drugs 4. Eventually Insulin |
|
|
What is the mode of action for Metformin?
|
makes muscle cells and fat cells utilize glucose in the peripheral tissue
|
|
|
What is the mode of action for Sulfonylureas and Thiazolidinediones?
|
Stimulate pancreas to make more insulin
|
|
-
|
-
|
|
|
Describe the pathogenesis leading to the complications seen in Diabetes
|
Nonenzymatic protein glycosylation through the polyol pathway
|
|
|
Explain the accelerated atherosclerosis as a complication of diabetes
|
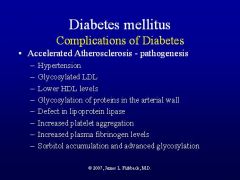
-
|
|
|
Nodular Glomerulosclerosis = Kimmelstiel-Wilson disease
-pink nodules ACE inhibitors |
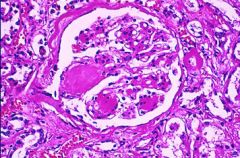
What is shown here?
What can prevent this complication? |
|
|
Papillary Necrosis = diabetes affects small vessels and end arteries
Papilla can slough off and occlude to ureter = hydroureter and kidney swelling |
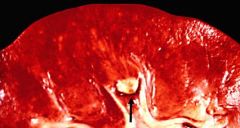
What is shown here? What is there risk of?
|
|
|
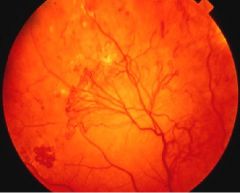
Describe the characteristics of Background Retinopathy
|
1. Hemorrhages
2. Microaneurysms 3. "cotton-wool" exudates 4. DOES NOT NORMALLY IMPAIR VISION!! |
|
|
What is the pathogenic cause of Diabetic Retinopathy?
|
Osmotic damage
|
|
|
Background Retinopathy
-follow the vessels out -vessels are thicker than normal and hemorrhaging can be seen -Starburst cotton-wool spots are seen at 3 o'clock |

What is shown here?
|
|
|
What is Proliferative Retinopathy?
|
Neo-vascular proliferation in the retina, which OBSCURES vision
|
|
|
What are common complications of Proliferative Retinopathy?
|
Retinal detachment and blindness
|
|
|
Proliferative Retinopathy
|
What is shown here?
|
|
|
Proliferative Retinopathy with Microaneurysms (due to Osmotic damage from increased Sorbitol)
|
What is seen here?
|
|
|
What is another name for Gallstones?
|
Cholelithiasis
|
|
|
What are the 10 F's that are associated risk factors for Cholesterol or Mixed Gallstones?
|
1. Fat = obese
2. Forty and above 3. Fertile = multiparous 4. Flatulent = intestinal disease or malabsorption 5. Female with Fatty, Foul, Fetid, Floating Feces |
|
|
What drugs can cause an increased risk for Cholesterol or Mixed Gallstones (Cholelithiasis)?
|
Cholesterol-lowering drugs
- Clofibrate - Cholestryramine |
|
|
When would a man be at an increased risk for developing Cholesterol Gallstones?
|
if he was on hormone therapy to treat Prostatic Carcinoma
|
|
|
What ethnicities are at increased risk for Cholesterol/Mixed Gallstones?
|
Pima & Navajo Indians
Scandinavian countries & Latin America |
|
|
List 4 examples of GI tract disorders that could lead to Cholesterol/Mixed Gallstones
|
1. Malabsorptive disorder
2. Ileal resection for obesity 3. Cystic Fibrosis with Pancreatic insufficiency 4. Chronic Diarrheal states |
|
|
What are the risk factors associated with Pigmented Gallstones?
|
1. Hemolytic anemias
2. Alcoholic Cirrhosis 3. Infected bile (E. coli) 4. Parasitic infections |
|
|
Examples of Hemolytic Anemias or Hemoglobinopathies that can cause Pigmented stones
|
1. Malaria
2. Sickle Cell anemia 3. Polycythemia vera |
|
|
What Parasitic infections can cause Pigmented (bilirubinate) stones?
|
Ascaris or Clonorchis sinensis
|
|
|
What is the most common type of Gallstone?
|
Mixed stone = composed primarily of cholesterol but also contain variable amounts of bilirubin and calcium salts
|
|
|
What clinical manifestation is characteristic of Cholelithiasis?
|
fatty food intolerance
|
|
|
What is the most common stone associated with Cholecystitis?
|
Mixed stone
|
|
|
What is the most common cause of both Acute and Chronic Cholecystitis?
|
Gallstones
-80% of acute -90% of chronic |
|
|
How do you diagnose Cholecystitis?
|
Murphy's sign = inspiratory arrest in response to palpation of the RUQ during deep inspiration
|
|
|
Acute Cholecystitis
-fibrinous exudates -red, congested = inflammation |

What is shown here?
|
|
|
Cholecystitis with stones (cholelithiasis)
|

What is seen here?
|
|
|
Cholecystitis with cholelithiasis
|

What is seen here?
|
|
|
Porecelain Gallbladder
-due to Dystrophic Calcification of the gallbladder -late complication of Chronic Cholecystitis |

What is seen here?
|
|
|
Porcelain Gallbladder
-consequence of transmural chronic inflammation -extensive fibrosis during the repair phase with scarring and DYSTROPHIC CALCIFICATION |
What is seen here?
Explain the pathogenesis |
|
|
What 2 things are present in 75-90% of cases of Carcinoma of the gallbladder?
|
Chronic Cholecystitis
Cholelithiasis |
|
|
What is a high-risk condition for Gallbladder Adenocarcinoma?
|
Porcelain gallbladder
|
|
|
Gallbladder Adenocarcinoma:
1. Gender preference 2. Age preference 3. Ethnic distribution 4. 5 year survival |
1. Female:Male = 2:1
2. Average age = 65 3. Pima and Navajo indians 4. 1% five-year survival |
|
|
Gallbladder Adenocarcinoma
-opened up, thicker than normal -fibrotic area |
What is seen here?
|
|
|
Gallbladder Adenocarcinoma
-Left: GB is thickened -Right: glandular structures indicating Adenocarcinoma |
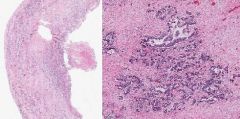
What is shown here?
|
|
|
What is the difference b/w Acute Interstitial Pancreatitis & Acute Hemorrhagic Pancreatitis?
|
Interstitial = mild inflammation characterized by widening edema and widening of interstitial spaces that contain scattered inflammatory cells
Hemorrhagic = Pancreatic Acinar cell injury results in activation of pancreatic enzymes and enzymatic destruction of pancreatic parenchyma |
|
|
What are the most common drugs associated with causing Acute Pancreatitis?
|
1. Azathiopurine
2. Mercaptopurine 3. Corticosteroids 4. high dose Estrogen |
|
|
Pseudocyst:
-massive necrosis leads to __1__ necrosis of the pancreatic tissue, which becomes enclosed by __2__. |
1. liquefactive
2. Granulation tissue |
|
|
What are 5 systemic complications of Acute Hemorrhagic Pancreatitis?
|
1. Shock = due to increased vascular permeability caused by pancreatic enzymes
2. DIC = pancreatic enzymes in circulation leads to formation of platelet and fibrin thrombi in small vessels 3. ARDS = due to enzymatic injury of the alveolar-capillary units in the lung -> hyaline membranes 4. Renal failure = due to shock 5. Subcutaneous Fat Necrosis = due to lipase enzymes from pancreas |
|
|
Explain Fat Necrosis and the Saponification reaction
|
Acute Hemorrhagic Pancreatitis causes release of Lipases which digest Fat, releasing Fatty acids which form Calcium soaps
|
|
|
Define Chronic Pancreatitis
|
Chronic inflammation with FIBROSIS leading to a progressive loss of pancreatic function
-reduction in size -often shows calcifications |
|
|
What do pigmented stones result from?
|
precipitation of excess insoluble unconjugated Bilirubin
Hemoglobin -> Heme -> Biliverdin -> Bilirubin |
|
|
What is the most common primary tumor of the Gallbladder?
|
Adenocarcinoma of the Gallbladder
|
|
|
Type of Diabetes that may cause Ketoacidosis?
|
Type 1 Insulin Dependent Diabetes
|

