![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
66 Cards in this Set
- Front
- Back
|
Outer zone of the kidney that contains Glomeruli and Tubules
|
Cortex
|
|
|
Part of Kidney that contains tubules, loops of henle, and collecting ducts
|
Medulla
|
|
|
Blood enters the glomerulus through the __1__ and exits through the __2__
|
1. Afferent arteriole
2. Efferent arteriole |
|
|
What do Afferent arterioles originate from?
|
Interlobular arteries
**which originate from Larger Lobar and Arcuate Arteries |
|
|
What is another name for Visceral Epithelial Cells of the Glomerulus?
|
Podocytes which have foot processes
|
|
|
Describe the Endothelial Cells of the Glomerulus
|
Form the capillary and are FENESTRATED, allowing filtration of plasma
|
|
|
Where are Mesangial Cells located?
|
central portion of the Glomerulus in the area where several loops meet; they are surrounded on all sides by mesangial matrix
|
|
|
Modified smooth muscle cells in the media of the Afferent arteriole that secrete Renin
|
Juxtaglomerular Cells
**Renin converts Angiotensin I -> Angiotensi II --> Vasoconstriction --> Aldosterone secretion from Adrenal Cortex = increased Sodium and Water reabsorption in distal tubules |
|
|
Cells of the distal tubule near the afferent arteriole; sense Sodium concentration in the tubule fluid; provide first impulse for the secretion of Renin
|
Macula Densa
|
|
|
Contractile and phagocytic cells of the Glomerulus
|
Mesangial cells
|
|
|
This is the most common form of Acute Renal Failures
What is the cause? What pathology is seen? |
Prerenal Failure
Hypoperfusion -Heart failure -Shock from surgery -Trauma Tubular Necrosis |
|
|
What are the 4 causes of Renal Failure?
|
1. Glomerular disease due to Acute Glomerulonephritis
2. Tubulointerstitial Nephritis due to a drug reaction 3. Vasculitis due to Wegener Granulomasotis 4. Toxic tubular necrosis due to Mercury poisoning |
|
|
What are 4 causes of Postrenal Failure?
|
1. Intratubular obstruction due to Acute Urate Nephropathy
2. Renal-pelvic obstruction due to Nephrolithiasis 3. Ureteric obstruction due to Urinary stones 4. Bladder/Urethral obstruction due to Prostatic hyperplasia |
|
|
What are the 4 progessive steps to Chronic Renal Failure?
|
1. Diminished Renal Reserve
2. Renal Insufficiency 3. Renal Failure 4. End-stage Renal Failure |
|
|
GFR that is 50% of normal
|
Diminished Renal Reserve
|
|
|
List the characteristics of Renal Insufficiency
|
1. GFR 30-50% of normal fxn
2. Azotemia = elevated blood nitrates (BUN & Creatinine) 3. Anemia = decreased EPO release = Normocytic, Normochromic 4. HTN 5. Reduced concentrating capacity |
|
|
List the characteristic of Renal Failure
|
1. GFR 20-25% of normal
2. Kidney cannot regulate solutes and fluid volume 3. Edema 4. Metabolic Acidosis |
|
|
What are the characteristics of End-stage Renal Disease?
|
Uremia
GFR is less than 5% of normal |
|
|
List the features of Uremia
|
1. Fluid and Electrolyte abnormalities = edema, acidosis, K+ increases
2. Phosphate increases and cannot be excreted = causes Ca+ imbalance = Hypercalcemia -> Parathyroid stimulation to secrete PTH -> Secondary Hyperparathyroidism 3. Bleeding time is prolonged due to abnormal platelets 4. GI effects = NVD, esophagitis, gastritis, colitis 5. Neuromuscular disorders -> Hypercalcemia = impulses cannot be transmitted b/c of imbalance b/w free and IC Ca+ |
|
|
Describe Potter Syndrome
|
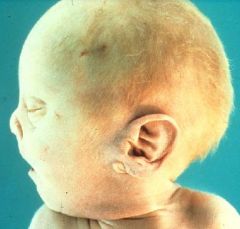
Renal agenesis resulting in Oligohydramnios (low amniotic fluid b/c baby cannot excrete it)
-Potter facies = flattened nose, low-set ears, recessed chin |
|
|
Where is the most common place for Ectopic Kidney?
|
Pelvis (pelvic brim)
**b/c of abnormal location, kinking or tortuosity of ureters may cause some obstruction to urinary flow |
|
|
Fusion of the kidneys, usually at the lower pole; may cause Urinary tract obstruction b/c of impingement on the Ureters
|
Horseshoe Kidneys
|
|
|
Describe the Adult form of Polycystic Kidney Disease
|
1. Autosomal Dominant
2. incidence of 1:1000 3. due to PKD-1 mutation 4. Bilaterally enlarged kidneys 5. Symptoms appear in adult life 6. Renal failure 5-10 years thereafter |
|
|
Explain the pathogenesis of the cysts in Adult Polycystic Kidney Disease
|
1. Mutation in PKD-1 gene
2. Polycystin-1 protein is a transmembrane protein that keeps cell anchored to eachother = mutated |
|
|
What are the associated conditions of Adult Polycystic Kidney Disease?
|
1. Liver Cysts (30%)
2. Splenic Cysts (10%) 3. Pancreatic cysts (5%) 4. Berry aneurysms (20%) 5. Diverticulosis coli 6. MITRAL VALVE PROLAPSE |
|
|
HTN, hematuria, and bilateral palpable renal masses in a patient with Mitral Valve Prolapse
|
Autosomal Dominant Polycystic Kidney Disease
|
|
|
List the 6 clinical findings in Nephritic Syndrome
|
1. Hematuria = inflammation causes the glomerulus to rupture thru the BM and leack blood into Bowman's Capsule = "smoky brown urine" or "bouillon-soup like"
2. Proteinuria = increased permeability of GBM 3. Hypoalbuminemia = causes Edema due to loss of oncotic pressure 4. Oliguria = due to reduced GFR 5. Edema = due to Salt and Water retention = Periorbital edema; Somnolence of affected kids is related to Brain Edema 6. Hypertension = due to reduced GFR -> Macula Densa -> JG apparatus -> Renin secretion |
|
|
List 3 general causes of Nephritic Syndrome
|
1. Immune-complexes deposit in the capillary of Glomeruli
2. Anti-GMB Ab's 3. Planted antigens from endogenous or Exogenous organisms = Strep antigen stuck in kidney |
|
|
Define Acute Postinfectious Glomerulonephritis
|
Acute NEPHRITIC syndrome 1-2 weeks after infection with Group A Beta-hemolytic Streptococci
|
|
|
A 10 year old girl presents to the clinic complaining of eye swelling. You remember this child from 3 weeks ago when she was seen for Pharyngitis. Upon taking a history and performing a physical, you find that the patient has pronounced periorbital edema, has been urinating very little despite adequate fluid intake, and has a blood pressure of 150/9. Lab findings include Azotemia, Hematuria, Red Cell Casts in the urine, and increased ASO Ab titer.
|
Acute Postinfectious Glomerulonephritis
**Immune-complex disease |
|
|
What age group does Acute Postinfectious Glomerulonephritis usually occur in?
|
Children
-90% recover -9% persistent hematuria, proteinuria -1% chronic renal disease |
|
|
What pathology is seen under the light microscope in ACUTE POSTINFECTIOUS GN
|
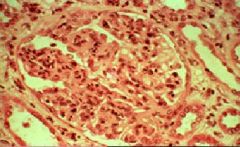
Hypercellularity
-Endothelial cells -Mesangial cells -PMNs |
|
|
What pathology is seen in Immunofluorescence in ACUTE POSTINFECTIOUS GN?
|
Irregular coarse granular Lumpy-bumpy pattern = deposits of IgG or C3
-deposits are in the Mesangium and along the Basement Membrane |
|
|
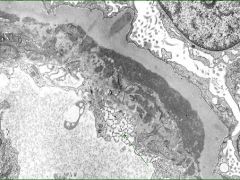
What pathology is seen on EM in ACUTE POSTINFECTIOUS GN?
|
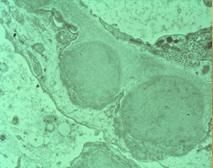
Electron-dense Humps on the EPITHELIAL side of the basement membrane = Subendothelial localization
|
|
|
Lupus is a systemic disease that is more common in __1__ and __2__
|
1. Women
2. African-americans |
|
|
In Lupus Glomerulonephritis, what is there a deposition of?
|
Immune-complexes
|
|
|
Lupus Glomerulonephritis is associated with deposits in these places
|
1. Blood vessels
2. Tubular Basement Membrane 3. Interstitium **can basically cause deposition anywhere in the kidney |
|
|
What test is used to judge the activity of Lupus?
|
Total Serum Complement
-low in lupus b/c it has been consumed |
|
|
Only disease that we know that causes deposits on the Subendothelial side
|
Lupus Glomerulonephritis
|
|
|
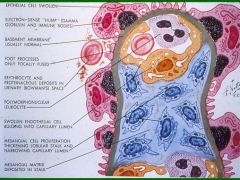
A = RBC
B = Endothelial cell C = Epithelial Cell D = Mesangial cell E = Bowman capsule |
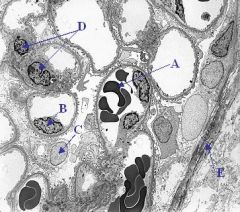
Label the letters
|
|
|
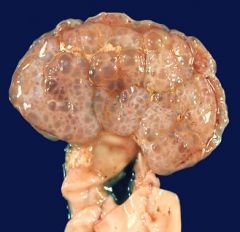
Autosomal Dominant Polycystic Kidney Disease
-both kidneys have large cysts |

What is this showing?
|
|
|
Autosomal Dominant Polycystic Kidney Disease
|

What is this picture showing?
|
|
|
Autosomal RECESSIVE PKD
- small cysts |
What is this picture showing?
|
|
|
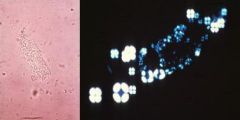
Acute Postinfectious GN
|
What would cause this pathology?
|
|
|
Capillary Lumens are occluded -> low GFR
-hypercellularity of Endothelial cells, Mesangial cells, PMN's Postinfectious GN |
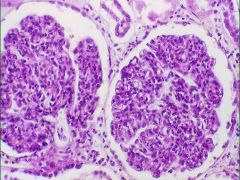
What is the obvious pathology here?
What is the cause? |
|
|
Subepithelial humps of immune complex deposits
Acute Postinfectious GN |
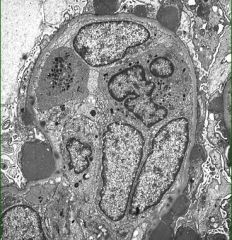
What pathology do you see here?
What is the cause? |
|
|
Acute Postinfectious GN
"lumpy-bumpy" IF = IgG, IgM, and C3 deposits throughout glomerulus |
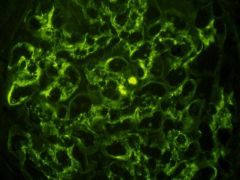
What is the cause of this?
|
|
|
Lupus Glomerulonephritis
|
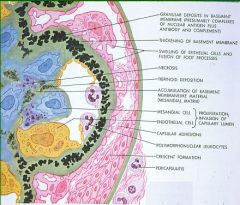
What would be the cause of these pathologies?
|
|
|
Subendothelial deposits
Lupus Glomerulonephritis |
What is seen here?
What is the cause? |
|
|
Subepithelial Deposits
capillary is occluded Lupus Glomeruonephritis |
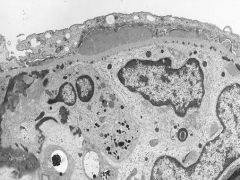
What is seen here?
What is the cause? |
|
|
BUN/Cr ratio is greater than 15: Pre-renal or Renal failure?
|
Pre-renal
|
|
|
What is Azotemia largely related to?
|
decreased GFR
|
|
|
When azotemia becomes associated with a constellation of clinical signs and symptoms
|
Uremia
|
|
|
Prerenal azotemia is encountered when there is _______ that impairs renal function in the ABSENCE of parenchymal damage
|
Hypoperfusion
|
|
|
When is Postrenal Azotemia seen?
|
whenever flow is obstructed below the level of the kidney
|
|
|
X-linked dominant disease with a defect in the synthesis of the alpha5-subtype of collage type IV in the GBM
|
Alport's Syndrome
|
|
|
A patient presents with hereditary nephritis, sensorineural hearing loss, and ocular defects. What is the diagnosis?
|
Alport Syndrome
|
|
|
A 10-year-old boy presents to the clinic complaining of a red tinge to his urine. A more detailed history reveals that he was diagnosed with mild nerve deafness 2 years earlier and also developed cataracts 1 year ago. Lab studies confirm hematuria as well as the presence of RBC casts
|
Alport syndrome
|
|
|
Development abnormality that may be uni- or bilateral. Results from irregular differentiation and morphogenesis of the Metanephros. Parenchyma of these abnormal kidneys consists of immmature nephrons, often showing signs of Cystic dilation
|
Cystic Renal Dysplasia
|
|
|
A child presents with an enlarged, unilateral flank mass. Biopsy shows abnormal structures persisting in the kidney (i.e. cartilage, immature collecting ductules, striated muscle)
|
Cystic Renal Dysplasia
|
|
|
Heavy proteinuria (> 3.5 grams/day)
Nephritic or Nephrotic? |
Nephrotic
|
|
|
Hematuria
Azotemia (BUN:Cr > 15) Proteinuria (<3.5 g/day) Oligouria Edema = periorbital HTN |
Nephritic Syndrome
|
|
|
RBC casts
Nephritic or Nephrotic? |
Nephritic
|
|
|
Generalized edema
Hyperlipidemia Lipiduria Nephritic or Nephrotic? |
Nephrotic
|
|
|
Nephrotic
|
Fatty casts with Maltese crosses and Oval Fat bodies
Nephritic or Nephrotic? |
|
|
Why is there HTN in Nephritic Syndrome?
|
reduced GFR causes a release of renin
|

