![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back
|
What part of TSH, LH, FSH, and hCG is the same? Which part determines its hormonal specificity?
|
- α subunit is the same
- β subunit gives specificity |
|
|
What are the types of pancreatic cells with endocrine function?
|
Islets of Langerhans:
- α cells - β cells - δ cells |
|
|
What is the source of Islets of Langerhans in the pancreas?
|
Arise from pancreatic buds
|
|
|
What is the function of the α, β, and δ cells in the Islets of Langerhans in the pancreas? Relative locations in Islet?
|
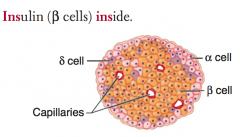
- α cells: glucagon (peripheral)
- β cells: insulin (central) = Insulin is Inside - δ cells: somatostatin (interspersed) |
|
|
How is insulin synthesized? Where?
|
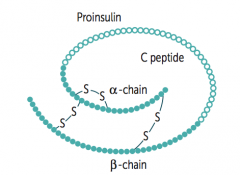
Takes place in β cells in Islets of Langerhans:
- Preproinsulin is synthesized in RER - Cleavage of "presignal" generates Proinsulin - Proinsulin is stored in secretory granules - Cleavage of Proinsulin → exocytosis of Insulin and C-peptide |
|
|
If you see both elevated Insulin and C-peptide vs only elevated Insulin, how does this help your differential?
|
- Elevated Insulin and C-peptide: Insulinoma
- Elevated Insulin without C-peptide: Exogenous Insulin administration |
|
|
How does insulin mediate its effects?
|
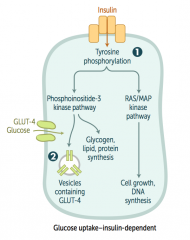
1. Binds insulin receptors (tyrosine kinase activity)
2. Induces glucose uptake (carrier-mediated transport) in insulin dependent tissues - Also induces gene transcription |
|
|
What happens when insulin binds to its receptor?
|
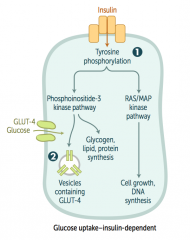
- Tyrosine phosphorylation
- Phosphoinositide-3 kinase pathway - Induces glycogen, lipid, and protein synthesis - Vesicles containing GLUT-4 are placed in membrane to allow entry of glucose into cell INsulin moves glucose INto cells |
|
|
What are the anabolic effects of insulin?
|
- ↑ Glucose transport in skeletal muscle and adipose tissue
- ↑ Glycogen synthesis and storage - ↑ Triglyceride synthesis - ↑ Na+ retention (kidneys) - ↑ Protein synthesis (muscles, proteins) - ↑ Cellular uptake of K+ and amino acids - ↓ Glucagon release |
|
|
What are the insulin-dependent glucose transporters? Locations?
|
GLUT-4: adipose tissue and skeletal muscle
|
|
|
What are the insulin-independent glucose transporters? Locations?
|
- GLUT-1: RBCs, brain, cornea
- GLUT-5 (fructose): spermatocytes, GI tract - GLUT-2 (bidirectional): β islet cells, liver, kidney, small intestine |
|
|
What type of glucose transporters are in the adipose tissue? Characteristics?
|
GLUT-4: insulin-dependent glucose transporter
|
|
|
What type of glucose transporters are in the skeletal muscle? Characteristics?
|
GLUT-4: insulin-dependent glucose transporter
|
|
|
What type of glucose transporters are in RBCs? Characteristics?
|
GLUT-1: insulin-independent glucose transporter
|
|
|
What type of glucose transporters are in the brain? Characteristics?
|
GLUT-1: insulin-independent glucose transporter
|
|
|
What type of glucose transporters are in the cornea? Characteristics?
|
GLUT-1: insulin-independent glucose transporter
|
|
|
What type of sugar transporters are in the spermatocytes? Characteristics?
|
GLUT-5 (fructose): insulin-independent transporter
|
|
|
What type of sugar transporters are in the GI tract? Characteristics?
|
- GLUT-5 (fructose): insulin-independent transporter
- GLUT-2 (bidirectional): insulin-indepdent transporter - small intestine |
|
|
What type of sugar transporters are in the β islet cells? Characteristics?
|
GLUT-2 (bidirectional): insulin-indepdent transporter
|
|
|
What type of sugar transporters are in the liver? Characteristics?
|
GLUT-2 (bidirectional): insulin-indepdent transporter
|
|
|
What type of sugar transporters are in the kidneys? Characteristics?
|
GLUT-2 (bidirectional): insulin-indepdent transporter
|
|
|
What kind of fuel does the brain use?
|
- Glucose for metabolism normally
- Ketone bodies during starvation |
|
|
What kind of fuel do RBCs use?
|
Always utilize glucose because they lack mitochondria fro aerobic metabolism
|
|
|
How do you remember the sites of insulin-indepdent glucose uptake?
|
BRICK L:
- Brain - RBCs - Intestine - Cornea - Kidneys - Liver |
|
|
What regulates insulin release?
|
- Glucose
- GH - β2-agonists |
|
|
How does glucose enter pancreatic β cells? What are the effects?
|
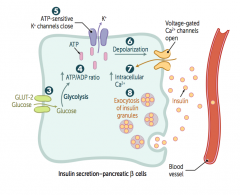
3. Glucose enters β cells via GLUT-2 (bidirectional) channels
4. ↑ ATP generated from glucose metabolism 5. Closes K+ channels 6. Depolarizes β cell membrane 7. Opens voltage-gated Ca2+ channels, resulting in Ca2+ influx 8. Stimulates insulin exocytosis |
|
|
What is the source of glucagon? Function?
|
- Made by α cells of pancreas
Functions in catabolism: - Glycogenolysis and gluconeogenesis → make more glucose - Lipolysis and ketone production → make alternative sources of energy |
|
|
What stimulates and inhibits glucagon secretion?
|
- Secreted in response to hypoglycemia
- Inhibited by insulin, hyperglycemia, and somatostatin |
|
|
What is the function of CRH?
|
↑ ACTH, MSH, and β-endorphin
|
|
|
What causes ↓ CRH?
|
Chronic exogenous steroid use
|
|
|
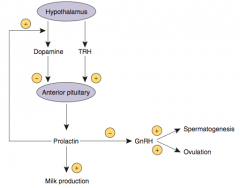
What is the function of Dopamine on the pituitary?
|
↓ Prolactin
|
|
|
What is the effect of Dopamine Antagonists (eg, anti-psychotics) on the pituitary?
|
Can cause galactorrhea (↑ prolactin)
|
|
|
What is the function of GnRH?
|
- ↑ FSH and LH
- Tonic GnRH suppresses the HPA axis - Pulsatile GnRH leads to puberty and fertility |
|
|
What regulates GnRH?
|
Regulated by Prolactin
|
|
|
What is the effect of tonic GnRH release?
|
Suppresses HPA axis
|
|
|
What is the effect of pulsatile GnRH release?
|
Leads to puberty and fertility
|
|
|
What is the function of Prolactin?
|
↓ GnRH
|
|
|
What are the consequences of a pituitary prolactinoma?
|
Amenorrhea (↓ GnRH) and Osteoporosis
|
|
|
What is the function of Somatostatin on the pituitary?
|
↓ GH and TSH
|
|
|
How can you treat acromegaly?
|
Somatostatin analogs (↓ GH)
|
|
|
What is the function of TRH?
|
↑ TSH and Prolactin
|
|
|
What are the effects of Prolactin?
|
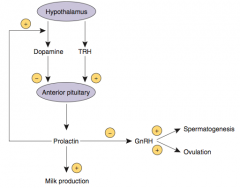
- Stimulates milk production in breasts
- Inhibits ovulation in females and spermatogenesis in males by inhibiting GnRH synthesis and release - Excessive prolactin associated with ↓ libido |
|
|
How is Prolactin regulated?
|
- Tonically inhibited by Dopamine from hypothalamus
- Prolactin inhibits its own secretion by ↑ Dopamine synthesis and secretion - TRH ↑ Prolactin secretion |
|
|
What drugs can be used to treat excess prolactin (such as prolactinoma)?
|
Dopamine Agonists - eg, Bromocriptine
- Dopamine inhibits Prolactin secretion |
|
|
What drugs may stimulate prolactin secretion?
|
- Dopamine antagonists (eg, anti-psychotics)
- Estrogens (OCPs, pregnancy) |
|
|
What are the effects of Growth Hormone (Somatotropin)?
|
- Stimulates linear growth and muscle mass through IGF-1 / somatomedin secretion
- ↑ Insulin resistance (diabetogenic) |
|
|
What is the effect of GH on insulin?
|
GH increases insulin resistance (diabetogenic)
|
|
|
What regulates Growth Hormone release?
|
- Released in pulses in response to GHRH (GH releasing hormone)
- Increases during sleep and exercise - Inhibited by glucose and somatostatin |
|
|
What can excess secretion of GH be due to? What can it cause?
|
- Could be due to pituitary adenoma
- Causes acromegaly (adults) or gigantism (children) |
|
|
What is the source of Anti-Diuretic Hormone (ADH)?
|
- Synthesized in hypothalamus (supraoptic nuclei)
- Released by posterior pituitary |
|
|
What is the function of Anti-Diuretic Hormone (ADH)?
|
- Regulates serum osmolarity (V2 receptors) and blood pressure (V1 receptors)
- ↓ serum osmolarity and ↑ urine osmolarity via regulation of aquaporin channel transcription in principal cells of renal collecting duct |
|
|
What diseases affect the levels / response to ADH?
|
- 1° Polydipsia: ADH is suppressed
- Central Diabetes Insipidus (DI): ADH ↓ - Nephrogenic Diabetes Insipidus (DI): ADH ↑ (kidney is resistant to its effects) |
|
|
What can cause nephrogenic diabetes insipidus?
|
Resistance to ADH can be mediated by a mutation in the V2 receptor (regulates serum osmolarity)
|
|
|
How do you treat central diabetes insipidus?
|
Desmopressin (ADH analog) - central DI is caused by insufficient production of ADH
|
|
|
What are the types of receptors that ADH acts on? Effects?
|
- V2 receptor: regulates serum osmolarity
- V1 receptor: regulates blood pressure |
|
|
How is ADH regulated?
|
- Osmoreceptors in hypothalamus (1°)
- Hypovolemia (2°) |

