![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
171 Cards in this Set
- Front
- Back
|
What is the initial thyroid precursor? Source? |
Thyroid Diverticulum - arises from floor of primitive pharynx
|
|
|
What happens to the Thyroid Diverticulum? What is it connected to?
|
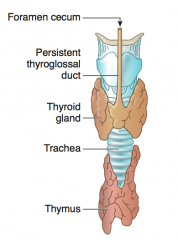
- Descends into neck from origin in floor of primitive pharynx
- Connected to tongue by thyroglossal duct |
|
|
How is the Thyroid initially connected to the Tongue? What happens to this connection?
|
- Thyroid diverticulum is connected to the tongue by the Thyroglossal Duct
- Normally disappears, but may persist as pyramidal lobe of thyroid - Foramen cecum is a normal remnant of the thyroglossal duct |
|
|
What is the normal remnant of the thyroglossal duct (connects tongue to thyroid diverticulum)?
|
Foramen Cecum
|
|
|
What is the most common ectopic thyroid tissue site?
|
Tongue
|
|
|
What diagnosis should you consider in a patient presenting with an anterior midline neck mass that moves with swallowing or protrusion of the tongue?
|

Thyroglossal Duct Cyst
|
|
|
What diagnosis should you consider if your patient presents with a mass in their lateral neck?
|
Branchial Cleft Cyst - persistent cervical sinus
|
|
|
What are the adrenal cortex and medulla derived from?
|
- Adrenal cortex: mesoderm
- Adrenal medulla: neural crest |
|
|
What are the layers of the adrenal cortex from external to internal?
|
- Zona Glomerulosa
- Zona Fasiculata - Zona Reticularis |
|
|
What is the primary regulatory control of the Zona Glomerulosa? Secretory product?
|
- Controlled by Renin-Angiotensin
- Secretes Aldosterone |
|
|
What is the primary regulatory control of the Zona Fasiculata? Secretory product?
|
- Controlled by ACTH and CRH
- Secretes cortisol and sex hormones |
|
|
What is the primary regulatory control of the Zona Reticularis? Secretory product?
|
- Controlled by ACTH and CRH
- Secretes sex hormones (eg, androgens) |
|
|
What kind of cells are in the Adrenal Medulla?
|
Chromaffin cells
|
|
|
What is the primary regulatory control of the Adrenal Medulla? Secretory product?
|
- Controlled by preganglionic sympathetic fibers
- Secretes catecholamines (epinephrine and norepinephrine) |
|
|
What is the most common tumor of the adrenal medulla in adults? What does it characteristically cause?
|
Pheochromocytoma
- Episodic hypertension |
|
|
What is the most common tumor of the adrenal medulla in children? What does it characteristically cause?
|
Neuroblastoma
- RARELY causes hypertension |
|
|
How is the adrenal gland drained on the left side?
|
Left adrenal gland → Left adrenal vein → Left renal vein → IVC
|
|
|
How is the adrenal gland drained on the right side?
|
Right adrenal gland → Right adrenal vein → IVC
|
|
|
What tissue are the anterior and posterior pituitary made from?
|
- Anterior Pituitary: oral ectoderm (Rathke pouch)
- Posterior Pituitary: neuroectoderm |
|
|
What is the other name for the posterior pituitary? What does it secrete?
|
Neurohypophysis
- Vasopressin / ADH - Oxytocin |
|
|
What is the source of ADH and Oxytocin?
|
They are both made in the hypothalamus and shipped to the posterior pituitary via the neurophysins (carrier proteins)
|
|
|
What is the other name for the anterior pituitary? What does it secrete?
|
Adenohypophysis
Think FLAT PiGs eat MuSH: - FSH - LH - ACTH - TSH - Prolactin - GH - MSH (Melanotropin) |
|
|
What kind of cells are there in the anterior pituitary? Functions?
|
- Acidophils: secretes Prolactin and GH
- Basophils: FSH, LH, ACTH, and TSH |
|
|
What are the subunits of the hormones released from the anterior pituitary? Functions?
|
- α subunit: hormone subunit common to TSH, LH, FSH, and hCG
- β subunit: determines hormone specificity |
|
|
Which hormones have the same α subunit?
|
- TSH
- LH - FSH - hCG |
|
|
What part of TSH, LH, FSH, and hCG is the same? Which part determines its hormonal specificity?
|
- α subunit is the same
- β subunit gives specificity |
|
|
What are the types of pancreatic cells with endocrine function?
|
Islets of Langerhans:
- α cells - β cells - δ cells |
|
|
What is the source of Islets of Langerhans in the pancreas?
|
Arise from pancreatic buds
|
|
|
What is the function of the α, β, and δ cells in the Islets of Langerhans in the pancreas? Relative locations in Islet?
|
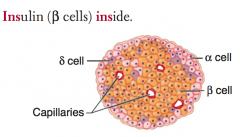
- α cells: glucagon (peripheral)
- β cells: insulin (central) = Insulin is Inside - δ cells: somatostatin (interspersed) |
|
|
How is insulin synthesized? Where?
|
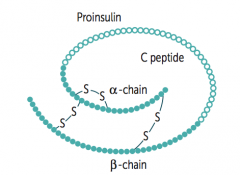
Takes place in β cells in Islets of Langerhans:
- Preproinsulin is synthesized in RER - Cleavage of "presignal" generates Proinsulin - Proinsulin is stored in secretory granules - Cleavage of Proinsulin → exocytosis of Insulin and C-peptide |
|
|
If you see both elevated Insulin and C-peptide vs only elevated Insulin, how does this help your differential?
|
- Elevated Insulin and C-peptide: Insulinoma
- Elevated Insulin without C-peptide: Exogenous Insulin administration |
|
|
How does insulin mediate its effects?
|
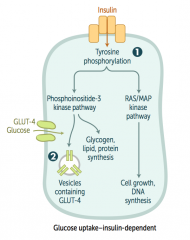
1. Binds insulin receptors (tyrosine kinase activity)
2. Induces glucose uptake (carrier-mediated transport) in insulin dependent tissues - Also induces gene transcription |
|
|
What happens when insulin binds to its receptor?
|
- Tyrosine phosphorylation
- Phosphoinositide-3 kinase pathway - Induces glycogen, lipid, and protein synthesis - Vesicles containing GLUT-4 are placed in membrane to allow entry of glucose into cell INsulin moves glucose INto cells |
|
|
What are the anabolic effects of insulin?
|
- ↑ Glucose transport in skeletal muscle and adipose tissue
- ↑ Glycogen synthesis and storage - ↑ Triglyceride synthesis - ↑ Na+ retention (kidneys) - ↑ Protein synthesis (muscles, proteins) - ↑ Cellular uptake of K+ and amino acids - ↓ Glucagon release |
|
|
What are the insulin-dependent glucose transporters? Locations?
|
GLUT-4: adipose tissue and skeletal muscle
|
|
|
What are the insulin-independent glucose transporters? Locations?
|
- GLUT-1: RBCs, brain, cornea
- GLUT-5 (fructose): spermatocytes, GI tract - GLUT-2 (bidirectional): β islet cells, liver, kidney, small intestine |
|
|
What type of glucose transporters are in the adipose tissue? Characteristics?
|
GLUT-4: insulin-dependent glucose transporter
|
|
|
What type of glucose transporters are in the skeletal muscle? Characteristics?
|
GLUT-4: insulin-dependent glucose transporter
|
|
|
What type of glucose transporters are in RBCs? Characteristics?
|
GLUT-1: insulin-independent glucose transporter
|
|
|
What type of glucose transporters are in the brain? Characteristics?
|
GLUT-1: insulin-independent glucose transporter
|
|
|
What type of glucose transporters are in the cornea? Characteristics?
|
GLUT-1: insulin-independent glucose transporter
|
|
|
What type of sugar transporters are in the spermatocytes? Characteristics?
|
GLUT-5 (fructose): insulin-independent transporter
|
|
|
What type of sugar transporters are in the GI tract? Characteristics?
|
- GLUT-5 (fructose): insulin-independent transporter
- GLUT-2 (bidirectional): insulin-indepdent transporter - small intestine |
|
|
What type of sugar transporters are in the β islet cells? Characteristics?
|
GLUT-2 (bidirectional): insulin-indepdent transporter
|
|
|
What type of sugar transporters are in the liver? Characteristics?
|
GLUT-2 (bidirectional): insulin-indepdent transporter
|
|
|
What type of sugar transporters are in the kidneys? Characteristics?
|
GLUT-2 (bidirectional): insulin-indepdent transporter
|
|
|
What kind of fuel does the brain use?
|
- Glucose for metabolism normally
- Ketone bodies during starvation |
|
|
What kind of fuel do RBCs use?
|
Always utilize glucose because they lack mitochondria fro aerobic metabolism
|
|
|
How do you remember the sites of insulin-indepdent glucose uptake?
|
BRICK L:
- Brain - RBCs - Intestine - Cornea - Kidneys - Liver |
|
|
What regulates insulin release?
|
- Glucose
- GH - β2-agonists |
|
|
How does glucose enter pancreatic β cells? What are the effects?
|
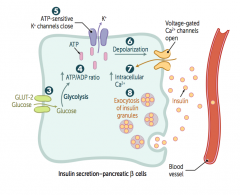
3. Glucose enters β cells via GLUT-2 (bidirectional) channels
4. ↑ ATP generated from glucose metabolism 5. Closes K+ channels 6. Depolarizes β cell membrane 7. Opens voltage-gated Ca2+ channels, resulting in Ca2+ influx 8. Stimulates insulin exocytosis |
|
|
What is the source of glucagon? Function?
|
- Made by α cells of pancreas
Functions in catabolism: - Glycogenolysis and gluconeogenesis → make more glucose - Lipolysis and ketone production → make alternative sources of energy |
|
|
What stimulates and inhibits glucagon secretion?
|
- Secreted in response to hypoglycemia
- Inhibited by insulin, hyperglycemia, and somatostatin |
|
|
What is the function of CRH?
|
↑ ACTH, MSH, and β-endorphin
|
|
|
What causes ↓ CRH?
|
Chronic exogenous steroid use
|
|
|
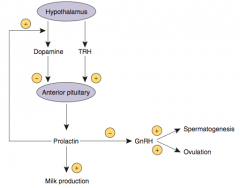
What is the function of Dopamine on the pituitary?
|
↓ Prolactin
|
|
|
What is the effect of Dopamine Antagonists (eg, anti-psychotics) on the pituitary?
|
Can cause galactorrhea (↑ prolactin)
|
|
|
What is the function of GnRH?
|
- ↑ FSH and LH
- Tonic GnRH suppresses the HPA axis - Pulsatile GnRH leads to puberty and fertility |
|
|
What regulates GnRH?
|
Regulated by Prolactin
|
|
|
What is the effect of tonic GnRH release?
|
Suppresses HPA axis
|
|
|
What is the effect of pulsatile GnRH release?
|
Leads to puberty and fertility
|
|
|
What is the function of Prolactin?
|
↓ GnRH
|
|
|
What are the consequences of a pituitary prolactinoma?
|
Amenorrhea (↓ GnRH) and Osteoporosis
|
|
|
What is the function of Somatostatin on the pituitary?
|
↓ GH and TSH
|
|
|
How can you treat acromegaly?
|
Somatostatin analogs (↓ GH)
|
|
|
What is the function of TRH?
|
↑ TSH and Prolactin
|
|
|
What are the effects of Prolactin?
|
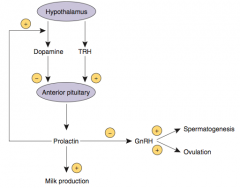
- Stimulates milk production in breasts
- Inhibits ovulation in females and spermatogenesis in males by inhibiting GnRH synthesis and release - Excessive prolactin associated with ↓ libido |
|
|
How is Prolactin regulated?
|
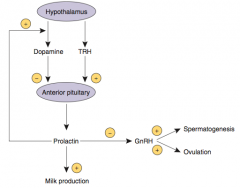
- Tonically inhibited by Dopamine from hypothalamus
- Prolactin inhibits its own secretion by ↑ Dopamine synthesis and secretion - TRH ↑ Prolactin secretion |
|
|
What drugs can be used to treat excess prolactin (such as prolactinoma)?
|
Dopamine Agonists - eg, Bromocriptine
- Dopamine inhibits Prolactin secretion |
|
|
What drugs may stimulate prolactin secretion?
|
- Dopamine antagonists (eg, anti-psychotics)
- Estrogens (OCPs, pregnancy) |
|
|
What are the effects of Growth Hormone (Somatotropin)?
|
- Stimulates linear growth and muscle mass through IGF-1 / somatomedin secretion
- ↑ Insulin resistance (diabetogenic) |
|
|
What is the effect of GH on insulin?
|
GH increases insulin resistance (diabetogenic)
|
|
|
What regulates Growth Hormone release?
|
- Released in pulses in response to GHRH (GH releasing hormone)
- Increases during sleep and exercise - Inhibited by glucose and somatostatin |
|
|
What can excess secretion of GH be due to? What can it cause?
|
- Could be due to pituitary adenoma
- Causes acromegaly (adults) or gigantism (children) |
|
|
What is the source of Anti-Diuretic Hormone (ADH)?
|
- Synthesized in hypothalamus (supraoptic nuclei)
- Released by posterior pituitary |
|
|
What is the function of Anti-Diuretic Hormone (ADH)?
|
- Regulates serum osmolarity (V2 receptors) and blood pressure (V1 receptors)
- ↓ serum osmolarity and ↑ urine osmolarity via regulation of aquaporin channel transcription in principal cells of renal collecting duct |
|
|
What diseases affect the levels / response to ADH?
|
- 1° Polydipsia: ADH is suppressed
- Central Diabetes Insipidus (DI): ADH ↓ - Nephrogenic Diabetes Insipidus (DI): ADH ↑ (kidney is resistant to its effects) |
|
|
What can cause nephrogenic diabetes insipidus?
|
Resistance to ADH can be mediated by a mutation in the V2 receptor (regulates serum osmolarity)
|
|
|
How do you treat central diabetes insipidus?
|
Desmopressin (ADH analog) - central DI is caused by insufficient production of ADH
|
|
|
What are the types of receptors that ADH acts on? Effects?
|
- V2 receptor: regulates serum osmolarity
- V1 receptor: regulates blood pressure |
|
|
How is ADH regulated?
|
- Osmoreceptors in hypothalamus (1°)
- Hypovolemia (2°) |
|
|
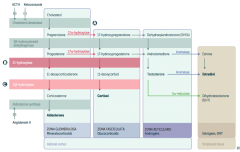
What is the first step in production of adrenal steroids?
|
Conversion of Cholesterol → Pregnenolone via Cholesterol Desmolase
|
|
|
How do you produce Aldosterone?
|
1. Cholesterol → Pregnenolone (Cholesterol Desmolase)
2. Pregnenolone → Progesterone (3β-hydroxysteroid dehydrogenase) 3. Progesterone → 11-deoxycorticosterone (21-hydroxylase) 4. 11-deoxycorticosterone → Corticosterone (11β-hydroxylase) 5. Corticosterone → Aldosterone (Aldosterone Synthase) |
|
|
What are the molecules on the way from Cholesterol to Aldosterone?
|
1. Cholesterol
2. Pregnenolone 3. Progesterone 4. 11-deoxycorticosterone 5. Corticosterone 6. Aldosterone |
|
|
What are the enzymes on the way from Cholesterol to Aldosterone?
|
1. Cholesterol Desmolase
2. 3β-hydroxysteroid dehydrogenase 3. 21-hydroxylase 4. 11β-hydroxylase 5. Aldosterone Synthase |
|
|
How do you produce Cortisol?
|
1. Cholesterol → Pregnenolone (Cholesterol Desmolase)
2. Pregnenolone → 17-hydroxypregnenolone (17α-hydroxylase) 3. 17-hydroxypregnenolone → 17-hydroxyprogesterone (3β-hydroxysteroid dehydrogenase) 4. 17-hydroxyprogesterone → 11-deoxycortisol (21-hydroxylase) 5. 11-deoxycortisol → Cortisol (11β-hydroxylase) Steps 2 and 3 can be switched around, but need both enzymes |
|
|
What are the molecules on the way from Cholesterol to Cortisol?
|
1. Cholesterol
2. Pregnenolone 3. 17-hydroxypregnenolone 4. 17-hydroxyprogesterone 5. 11-deoxycortisol 6. Cortisol OR 3. Progesterone (depending on order of enzymes) |
|
|
What are the enzymes on the way from Cholesterol to Aldosterone?
|
1. Cholesterol desmolase
2. 17α-hydroxylase 3. 3β-hydroxysteroid dehydrogenase 4. 21-hydroxylase 5. 11β-hydroxylase (Enzymes 2 and 3 can be done in either order) |
|
|
How do you produce Estradiol?
|
1. Cholesterol → Pregnenolone (Cholesterol Desmolase)
2. Pregnenolone → 17-hydroxypregnenolone (17α-hydroxylase) 3. 17-hydroxypregnenolone → Dehydroepiandrosterone (DHEA) 4. DHEA → Androstenedione 5. Androstenedione → Estrone (Aromatase) 6. Estrone → Estradiol OR 5. Androstenedione → Testosterone 6. Testosterone → Estradiol (Aromatase) |
|
|
What are the actions of Aromatase?
|
- Androstenedione → Estrone
- Testosterone → Estradiol |
|
|
What are the actions of 5α-Reductase?
|
Testosterone → Dihydrotestosterone (DHT)
|
|
|
Which enzyme deficiency would cause:
- Mineralocorticoids: ↑ - Cortisol: ↓ - Sex Hormones: ↓ |
17α-Hydroxylase (A)
Glucocorticoid and Androgen/Estrogen precursors cannot be produced, which shuttles more Pregnenolone / Progesterone substrate through the Aldosterone pathway |
|
|
Which enzyme deficiency would cause:
- Mineralocorticoids: ↓ - Cortisol: ↓ - Sex Hormones: ↑ |
21-Hydroxylase (B)
Progesterone and 17-Hydroxyprogesterone cannot continue towards formation of Aldosterone and Cortisol, so they get shuttled to the sex hormone pathway |
|
|
Which enzyme deficiency would cause:
- Mineralocorticoids: ↓ / ↑ - Cortisol: ↓ - Sex Hormones: ↑ |
11β-Hydroxylase (C)
- ↓ Aldosterone - ↑ 11-deoxycorticosterone (results in ↑ BP) - Cortisol can't be made - Sex hormones increased due to extra substrate |
|
|
What is similar about 17α-hydroxylase, 21-hydroxylase, and 11β-hydroxylase deficiencies?
|
All congenital adrenal enzyme deficiencies → enlargement of both adrenal glands due to ↑ ACTH stimulation (due to ↓ cortisol)
|
|
|
What labs are associated with 17α-hydroxylase deficiency?
|
- ↑ Mineralocorticoids
- ↓ Cortisol - ↓ Sex hormones (↓ DHT) - Hypertension - Hypokalemia |
|
|
How does a patient with 17α-hydroxylase deficiency present?
|
↑ Mineralocorticoids, ↓ Cortisol, and ↓ Sex hormones causes:
- XY: pseudo-hermaphroditism (ambiguous genitalia, undescended testes) - XX: lack secondary sexual development - Both: hypertension, hypokalemia |
|
|
What labs are associated with 21-hydroxylase deficiency?
|
- ↓ Mineralocorticoids
- ↓ Cortisol - ↑ Sex hormones (↑ 17-hydroxy-progesterone) - Hypotension - Hyperkalemia - ↑ Renin activity |
|
|
How does a patient with 21-hydroxylase deficiency present?
|
↓ Mineralocorticoids, ↓ Cortisol, and ↑ Sex Hormones causes:
- Presents in infancy with salt-wasting or in childhood with precocious puberty - XX: virilization - Hypotension, hyperkalemia, ↑ Renin activity |
|
|
What labs are associated with 11β-hydroxylase deficiency?
|
- ↓ Aldosterone
- ↑ 11-deoxycorticosterone (results in ↑ BP) - Hypertension - Low renin - ↓ Cortisol - ↑ Sex hormones |
|
|
How does a patient with 11β-hydroxylase deficiency present?
|
↓ Aldosterone, ↑ 11-deoxycorticosterone, ↓ Cortisol, and ↑ Sex hormones causes:
- XX: virilization - Hypertension |
|
|
What diagnosis should you consider in an XY patient who presents with pseudo-hermaphroditism (ambiguous genitalia, undescended testes)? Other findings?
|
17α-hydroxylase deficiency
- Hypertension - Hypokalemia - ↓ Sex hormones (↓ DHT) - ↓ Cortisol - ↑ Aldosterone |
|
|
What diagnosis should you consider in an XX patient lacking secondary sexual development? Other findings?
|
17α-hydroxylase deficiency
- Hypertension - Hypokalemia - ↓ Sex hormones (↓ DHT) - ↓ Cortisol - ↑ Aldosterone |
|
|
What diagnosis should you consider in an infant presenting with salt wasting? Other findings?
|
21-Hydroxylase deficiency
- Hypotension - Hyperkalemia - ↓ Mineralocorticoids - ↓ Cortisol - ↑ Sex hormones |
|
|
What diagnosis should you consider in an child with precocious puberty? Other findings?
|
21-Hydroxylase deficiency
- Hypotension - Hyperkalemia - ↓ Mineralocorticoids - ↓ Cortisol - ↑ Sex hormones |
|
|
What diagnosis should you consider in an XX patient with virilization? Other findings?
|
21-Hydroxylase deficiency
- Hypotension - Hyperkalemia - ↓ Mineralocorticoids - ↓ Cortisol - ↑ Sex hormones OR 11β-Hydroxylase deficiency - Hypertension (d/t ↑ 11-deoxycorticosterone) - ↓ Aldosterone - ↓ Cortisol |
|
|
What is the source of Cortisol? What does it bind in the blood?
|
- Adrenal Zona Fasciculata
- Binds to corticosteroid-binding globulin |
|
|
What are the effects of Cortisol?
|
Cortisol is a BIG FIB:
- ↑ BP - ↑ Insulin resistance - ↑ Gluconeogenesis, lipolysis, and proteolysis - ↓ Fibroblast activity - ↓ Inflammatory and immune responses - ↓ Bone formation |
|
|
How does cortisol affect BP?
|
↑ BP: upregulates α1-receptors on arterioles → ↑ sensitivity to NE and Epi
|
|
|
How does cortisol affect insulin?
|
↑ Insulin resistance → diabetogenic
|
|
|
How does cortisol affect stored forms of energy?
|
- ↑ Gluconeogenesis
- ↑ Lipolysis - ↑ Proteolysis |
|
|
How does cortisol affect fibroblasts? Effect?
|
↓ Fibroblast activity → causes striae
|
|
|
How does cortisol affect inflammation / immune responses?
|
↓ Inflammatory and Immune responses:
- Inhibits production of leukotrienes and prostaglandins - Inhibits leukocyte adhesion → neutrophilia - Blocks histamine release from mast cells - Reduces eosinophils - Blocks IL-2 production |
|
|
How does cortisol affect bones?
|
↓ Bone formation due to ↓ Osteoblast activity
|
|
|
What infections can be reactivated after administration of exogenous corticosteroids? How?
|
Reactivation of TB and Candidiasis
- Due to blocked IL-2 production |
|
|
How is Cortisol regulated?
|
- CRH (hypothalamus) stimulates ACTH release (pituitary), causing cortisol production in adrenal zona fasciculata
- Excess cortisol ↓ CRH, ACTH, and cortisol secretion |
|
|
What is the effect of chronic stress on cortisol?
|
Chronic stress induces prolonged secretion of Cortisol
|
|
|
What is the source of Parathyroid Hormone (PTH)?
|
Chief cells of parathyroid gland
|
|
|
What are the effects of PTH?
|
- ↑ Bone resorption of Ca2+ and PO4(3-)
- ↑ Kidney reabsorption of Ca2+ in distal convoluted tubule - ↓ Reabsorption of PO4(3-) in proximal convoluted tubule - ↑ 1,25-(OH)2-D3 (Calcitriol) production by stimulating kidney 1α-hydroxylase |
|
|
How does PTH affect the nephron? Which parts?
|
- ↑ Kidney reabsorption of Ca2+ in distal convoluted tubule
- ↓ Reabsorption of PO4(3-) in proximal convoluted tubule |
|
|
How does PTH affect the bones?
|
↑ Bone resorption of Ca2+ and PO4(3-)
- ↑ Production of macrophage colony-stimulating factor and RANK-L (receptor activator of NF-κB ligand) - RANK-L secreted by osteoblasts and osteocytes binds RANK (receptor) on osteoclasts and their precursors → stimulates osteoclasts and ↑ Ca2+ |
|
|
How does PTH affect the kidney, besides its action on the nephron?
|
↑ 1,25-(OH)2-D3 (Calcitriol) production by stimulating kidney 1α-hydroxylase
|
|
|
Which enzyme produces 1,25-(OH)2-D3 (calcitriol) in the kidney?
|
1α-Hydroxylase
|
|
|
What is the net effect of PTH on Ca2+ and PO4(3-) in the serum and urine?
|
- ↑ Serum Ca2+
- ↓ Urine Ca2+ - ↓ Serum PO4(3-) - ↑ Urine PO4(3-) (Phosphate Trashing Hormone = PTH) |
|
|
What peptide is similar to PTH? Source?
|
PTH-related peptide (PTHrP)
- Functions like PTH - Commonly ↑ in malignancies (eg, paraneoplastic syndrome) |
|
|
How is PTH regulated?
|
- ↓ Serum Ca2+ → ↑ PTH
- ↓ Serum Mg2+ → ↑ PTH - ↓↓ Serum Mg2+ → ↓ PTH |
|
|
What are common causes of ↓ Mg2+?
|
- Diarrhea
- Aminoglycosides - Diuretics - Alcohol abuse |
|
|
What is the effect of PTH on the intestine?
|
- Increases intestinal Ca2+ absorption
- Increases intestinal PO4(3-) absorption |
|
|
What are the forms of calcium in the plasma? What percent is in each form?
|
- Ionized (~45%)
- Bound to albumin (~40%) - Bound to anions (~15%) |
|
|
How does pH affect calcium homeostasis in the plasma?
|
↑ in pH → ↑ affinity of albumin (negative charge) to bind Ca2+
Clinical manifestations of hypocalcemia: - Cramps - Pain - Paresthesias - Carpopedal spasm |
|
|
What are the sources of Vitamin D? Activation?
|
- D3 from sun exposure in skin
- D2 ingested from plants - Both converted to 25-OH in liver and to 1,25-(OH)2 (active form) in kidney - 24,25-(OH)2-D3 is an inactive form |
|
|
What is the function of Vitamin D (Cholecalciferol)?
|
- ↑ Absorption of dietary Ca2+ and PO4(3-)
- ↑ Bone resorption → ↑ Ca2+ and PO4(3-) |
|
|
How is Vitamin D regulated?
|
- Increased 1,25-(OH)2-D production by: ↑ PTH, ↓ [Ca2+], ↓ [PO4(3-)]
- 1,25-(OH)2 feedback inhibits its own production |
|
|
What are the implications of a deficiency of Vitamin D?
|
- Rickets in kids
- Osteomalacia in adults |
|
|
What can cause a Vitamin D deficiency?
|
- Malabsorption
- ↓ Sunlight - Poor diet - Chronic kidney failure |
|
|
What is the source of Calcitonin?
|
Parafollicular cells (C cells) of Thyroid
|
|
|
What is the function of Calcitonin?
|
↓ Bone resorption of Ca2+ → Tones down Ca2+ levels
|
|
|
What regulates Calcitonin?
|
↑ Serum Ca2+ causes Calcitonin secretion (to tone down Ca2+ levels in serum)
|
|
|
How do PTH and Calcitonin relate?
|
- Calcitonin opposes actions of PTH
- Calcitonin is not important in normal Ca2+ homeostasis |
|
|
Which endocrine hormones signal via "cAMP"?
|
FLAT ChAMP + CGG:
- FSH - LH - ACTH - TSH - CRH - hCG - ADH (V2 receptor) - MSH - PTH - Calcitonin - GHRH - Glucagon |
|
|
Which endocrine hormones signal via "cGMP"?
|
Think vasodilators:
- ANP - NO (EDRF) |
|
|
Which endocrine hormones signal via "IP3"?
|
GOAT HAG:
- GnRH - Oxytocin - ADH (V1 receptor) - TRH - Histamine (H1 receptor) - Angiotensin II - Gastrin |
|
|
Which endocrine hormones signal via "steroid receptors"?
|
VETTT CAP:
- Vitamin D - Estrogen - Testosterone - T3 and T4 - Cortisol - Aldosterone - Progesterone |
|
|
Which endocrine hormones signal via "intrinsic tyrosine kinase"?
|
MAP kinase pathway, think growth factors
- Insulin - IGF-1 - FGF - PDGF - EGF |
|
|
Which endocrine hormones signal via "receptor-associated tyrosine kinase"?
|
JAK/STAT pathway, think acidophiles and cytokines (PIG)
- Prolactin - Immunomodulators: IL-2, IL-6, IL-8, IFN - GH |
|
|
What kind of signaling pathway is important for the MAP kinase pathway?
|
Intrinsic tyrosine kinase
|
|
|
What kind of signaling pathway is important for the JAK?STAT kinase pathway?
|
Receptor-associated tyrosine kinase
|
|
|
What is the signaling pathway of steroid hormones?
|
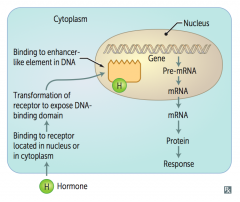
- Steroid hormone binds to receptor located in nucleus or cytoplasm
- Transformation of receptor to expose DNA-binding domain - Enters cell and binds to enhancer-like element in DNA - Affects gene transcription: pre-mRNA → mRNA → protein → response |
|
|
What happens to steroid hormones in the serum? Why?
|
Steroid hormones are lipophilic and therefore must circulate bound to specific binding globulins, which ↑ their solubility
|
|
|
What happens to men with increased sex-hormone binding globulin (SHBG)?
|
Gynecomastia
|
|
|
What happens to women with increased sex-hormone binding globulin (SHBG)?
|
Hirsutism
|
|
|
What can increase the amount of sex-hormone binding globulin (SHBG)?
|
- OCPs
- Pregnancy (Free estrogen levels remain unchanged) |
|
|
What are the iodine containing hormones that control the body's metabolic rate?
|
Thyroid Hormones: T3/T4
|
|
|
What is the source of the thyroid hormones (T3/T4)?
|
- Follicles of thyroid
- Most T3 formed in target tissues |
|
|
What are the functions of thyroid hormones?
|
- Bone growth (synergism with GH)
- CNS maturation - ↑ CO, HR, SV, contractility - ↑ Basal metabolic rate - ↑ Glycogenolysis, gluconeogenesis, lipolysis |
|
|
How do thyroid hormones affect the heart? Effects?
|
↑ β1 receptors in heart → ↑ CO, HR, SV, contractility
|
|
|
How do thyroid hormones affect the basal metabolic rate? Effects?
|
↑ BMR by ↑ Na+/K+ ATPase activity → ↑ O2 consumption, RR, and body temperature
|
|
|
What are the effects of thyroid hormones on energy storage?
|
↑ Glycogenolysis, gluconeogenesis, and lipolysis
|
|
|
What is the mnemonic to remember the T3 functions?
|
T3 functions - 4 B's:
- Brain maturation (CNS) - Bone growth - β-adrenergic effects (↑ β1 receptors) - Basal metabolic rate ↑ |
|
|
What binds the thyroid hormones in the blood? What hormones are active?
|
- Thyroxine-binding globulin (TBG) binds most T3/T4 in the blood
- Only the free hormone is active |
|
|
What can decrease the amount of Thyroxine-Binding Globulin (TBG)?
|
Hepatic Failure
|
|
|
What can increase the amount of Thyroxine-Binding Globulin (TBG)?
|
Pregnancy or OCP use (estrogen ↑ TBG)
|
|
|
What is the major thyroid product? What happens to it?
|
- T4 is the major thyroid product
- Converted to T3 in peripheral tissue by 5'-deiodinase |
|
|
What enzyme converts T4 to T3 in the peripheral tissues?
|
5'-deiodinase
|
|
|
Which form of the thyroid hormones can bind receptors with greater affinity?
|
T3 binds receptors with greater affinity than T4
|
|
|
What enzyme is responsible for oxidation and organification of iodide?
|
Peroxidase
|
|
|
What enzyme is responsible for coupling of monoiodotyrosine (MIT) and diodotyrosine (DIT)?
|
Peroxidase
|
|
|
What drug can inhibit both peroxidase and 5'-deiodinase?
|
Propylthiouracil
|
|
|
What drug can inhibit peroxidase but not 5'-deiodinase?
|
Methimazole
|
|
|
What regulates Thyroid Hormones (T3/T4)?
|
- TRH (hypothalamus) stimulates TSH (pituitary), which stimulates follicular cells
- Negative feedback by T3, T4 to anterior pituitary ↓ sensitivity to TRH - Thyroid stimulating immunoglobulins (TSIs), like TSH, stimulate follicular cells (eg, Graves disease) |
|
|
What is the name of the effect when excess iodine temporarily inhibits thyroid peroxidase? Effect?
|
Wolff-Chaikoff effect:
- ↓ Iodine organification → ↓ T3/T4 production |

