![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
115 Cards in this Set
- Front
- Back
|
Parkinson's Disease: Famous people with |
-- Michael J Fox.
-- Muhammed Ali. |
|
|
Parkinson's Disease:
Prognosis |
Slowly progressive and degenerative |
|
|
Parkinson's Disease:
What is disease progression in general |
The progression for Parkinson's Disease is: 1. Unilateral tremor. 2. Bilateral tremor. 3. Symptoms worsen. Onset of difficulties with ADL but can live independently. 4. Requires help with some or all ADLs. 5. Confined to wheelchair or bed. Maximally assisted. |
|
|
Spina bifida -- what are the root meanings of these two words |
Spina = spine. Bifida = split.
Spina Bifida literally means "split spine". |
|
|
Spina Bifida:
1. what is it ?
2. etiology? |
1, Spina bifida is a neural tube defect (neural tube is what becomes brain and spinal cord)
2, Etiology is unknown (idiopathic)
|
|
|
Spina Bifida: describe the 3 types |
1. Occult spinal dysraphism (OSD). -- presence of external manifestation but no protrusion. 2. Spina bifida w/ meningocele. -- protrusion BUT doesn't include spinal cord. 3. Spina Bifida w/ myelomeningocele. -- protrusion includes spinal cord or nerves roots. |
|
|
Muscular DystrophIES, as a category. Are they degenerative? |
Yes, MS or multiple sclerosis is a degenerative disorders. |
|
|
Muscular Dystrophies, as a category: Onset |
MD, or Muscular Dystrophy, can begin at any time during life. in Infancy, Childhood, or in Adulthood. |
|
|
Muscular Dystrophies, as a category:
1. What is its progression?
2. How is it diagnosed? |
1. MD, mulscular dystrophy, may be rapid and fatal, or may remain stable throughout life.
(Those starting early in life, tend to be more severe and progress more rapidly.)
2. Dx: Blood test for muscle enzymes or proteins |
|
|
Muscular Dystrophies, as a category:
Name 4 symptoms |
1. Low muscle tone, & weakness. (these contribute to abnormal movement pattern & delayed developmental milestones) 2. Oral motor feeding may be difficult 3. Deformities of the extremities and spine, (these are caused by muscle weakness) 4. Breathing difficulty. This may require tracheostomies or mechanical ventilators. Breathing difficulties often lead to death. |
|
|
define dystrophy |
Dystrophy is a disorder in which tissue or an organ wastes away. |
|
|
Muscular Dystrophy -- In the test prep course, what did she suggest we learn about Muscular Dystrophy? |
General info about MD and Duchenne's MD. |
|
|
(Duchenne's) do shanes Muscular Dystrophy: What gender gets it? |
Do shanes Muscular Dystrophy sex-linked to males. |
|
|
(Duchenne's) do shanes Muscular Dystrophy:
1. When is it usually detected?
2. What is the prognosis regarding a person's lifespan? |
(MD can have onset anytime in life. But do shanes hits early and is detected age 2 - 6)
2. The lifespan for someone with do shanes Muscular Dystrophy is usually in their early 20's. This is due to respiratory problems, infections, and/or cardiovascular problems. |
|
|
Huntington's Disease can also be referred to as what? |
Huntington's Disease can also known as Huntington's korea. (Chorea)
(Although technically, it is now referred to Huntington's Disease.) |
|
|
What is HUNTINGTON'S DISEASE, and what is it's prognosis? |

(Image: Huntington's Disease is a headhunter!) Huntington's Disease causes a progressive breakdown of nerve cells in the brain. |
|
|
Huntington's Disease is characterized by what 2 symptoms?
(Also, what third symptom MAY be involved?) |
1. Choreiform movement.
2. Progressive intellectual deterioration. . (Also, there may be psychiatric disturbance preceding onset of the movement disorder) |
|
|
ALS:
1. What's its complete name? |
ALS is Amyotrophic Lateral Sclerosis. |
|
|
ALS. What is it? |
[Image] ALS is an MND. ALS is a motor neuron disease. It is characterized by progressive degeneration of certain parts of the spinal cord. |
|
|
ALS:
1. onset is usually when?
2. death usually occurs when? |
1. The onset of ALS is at an average age of 57.
2. Death from ALS is usually 2-5 years after diagnosis. |
|
|
ALS:
What are the symptoms? |
The sypmtoms of ALS are primarily muscle weakness and atrophy. Many problems result from this, including dysarthria and dysphagia. |
|
|
What is the brachial plexus? |
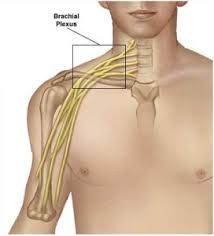
[Image]
The Brachial Plexus is a bundle of nerves in the chest that control the arm. |
|
|
Brachial Plexus Disorder:
1. What is the etiology?
2. What are some of the symptoms? |
1. Etiology. Traction during birth or otherwise; invasion of metastatic cancer, etc.
2. The symptoms of Brachial plexus disorder can be varied. They include motor and sensory disorders of the corresponding limb. |
|
|
Peripheral Neuropathies:
1. Where do they come from?
2. What does is cause? |
1. Peripheral neuropathy is damage to your peripheral nerves.
2. Peripheral neuropathy often causes weakness, numbness and pain. This is usually in your hands and feet. (It can also affect other areas of your body.) |
|
|
Guillain-Barre Syndrome.
What is it? |
Guillian-Barre is an autoimmune disorder. The body's immune system specifically attacks part of the peripheral nervous system. This causes demyelnation of the nerves. |
|
|
Guillain-Barre Syndrome.
1. When does recovery from this syndrome usually begin?
2. What is the potential long term prognosis? This question is not to be confused with the general progression, which is on another card. |
1. Recovery from Guillain-Barre Syndrome usually begins about 2 to 4 weeks after onset.
2. Potential long term prognosis is as follows. A small percentage die. Most are ambulatory in 6 months, (80%). Half display residual neurological effects. |
|
|
Guillain-Barre Syndrome.
-- what is the etiology |
The etiology of Guillain-Barre Syndrome is idiopathic. It may occur after an infectious disorder, surgery, or an immunization. |
|
|
Who gets Guillain-Barre Syndrome? |
Anyone can get it. |
|
|
What is the progression of Gullain-Barre Syndrome? |
Progression is rapid, goes from feet up:
1. Weakness or tingling sensations in the legs. 2. May spread to arms and upper body. 3. Increase in intensity until certain muscles cannot be used at all. When severe, the person is almost totally paralyzed. |
|
|
Myasthenia Gravis - what is its literal translation? |
Myasthenia Gravis means "grave muscle weakness".
(It is referred to as "weakness" because proper function in the neuromuscular junction can be reduced by 80% from this condition, not 100%) |
|
|
Myasthenia Gravis.
What is the usual progression? |
Myasthenia Gravis is usually progressively disabling. Death may occur from respiratory complications. |
|
|
Who gets Myasthenia Gravis? |
Everyone can. |
|
|
What is Myasthenia Gravis? |
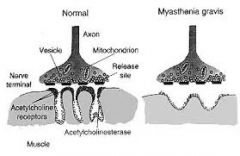
Myasthenia Gravis is autoimmune. It debilitates function of neuromuscular junction, causing muscle weakness. (Note the shallow "GRAVES" on image.) |
|
|
What are symptoms of Myasthenia Gravis? |
The symptoms of Myasthenia Gravis are.
1. Change throughout the day 2. Muscle fatigue after exercise 3. Dysarthria, dysphagia 4. Involvement of respiratory muscle may be life threatening |
|
|
What is M.S.? |
MS is multiple sclerosis. MS is an autoimmune disease. Bad T cells attack the myelin sheaths on neurons in the brain. Then info can't transfer well through these neurons. This results in varied problems throughout different parts of the body. |
|
|
What are some symptoms of M,S? |
Some symptoms of M.S. are: 1. Multiple and varied neurological symptoms and signs. These usually have remissions and exacerbations. 2. Weakness and clumsiness in the leg or hand is common. 3. Emotional disturbances . |
|
|
Name the 5 kinds of paralysis: |
1. Monoplegia: 1 extremity. |
|
|
Name the 5 kinds of paralysis (this includes the image of 5 types of paralysis) |
1. Monoplegia. 1 extremity. 2. Hemiplegia. upper & lower extremity of same side 3. Paraplegia. Legs only. (hint: parachute pants cover legs) 4. Tetraplegia. (prev quadriplegia) all extremities 5. Diplegia. Legs worse than arms |
|
|
What does the ASIA scale measure? |
The ASIA scale measures the degree of impairment and severity of injury of spinal cord injuries. |
|
|
What is autonomic dysreflexia. And tell what its symptoms are? |
1. Autonomic dysreflexia is an abnormal response to a noxious stimulus, like catheter blockage, sitting on a sharp object, etc. 2. The symptoms of autonomic dysreflexia are increased blood pressure, pounding headache, sweating. 3. It is deemed a medical emergency if not reversed quickly by removing stimulus. |
|
|
What is heterotrophic ossification? What is the hint to help remember this? |

[Image] Heterotrophic ossification is the formation of bone in strange places.
Hint: hetero- means "different". |
|
|
What is the full name for a TBI ? |
TBI is traumatic brain injury. |
|
|
What scales are used to rate where is a person is at after they have a TBI? |
The two scales used are the Glasgow Coma Scale
and
the Rancho Level of Cognitive Functioning. |
|
|
Rancho de los Amigos:
1. What is its full name?
2. What does it measure? (What is the memory trigger for this?) |
1. Rancho de los Amigos Levels of Cognitive Functioning.
2. Rancho los Amigos measures level of cognitive function. [HINT: the THREE AMIGOS! were low level cognitive functioning! They needed this test.] |
|
|
Rancho de los Amigos Levels of Cognitive Functioning:
What is the memory hint to remember the number of levels? |
[Image] Hint: Los tres amigos... times 3-1/3! (Visualize them introducing like in the movie, but they keep coming...10 times!) |
|
|
CVA: what is the full name and what is it? |
CVA is cerebral vascular accident, or stroke.
A CVA occurs from an insufficient blood supply to the brain, which causes tissue death. |
|
|
What are some of the functions of the left and right sides of your brain? |
Left: Right sided movement, processing, sensory info, & visual perception. Also Verbal processing. Bilateral motor praxis. Verbal memory. Speech. Processing verbal auditory. Right: Left sided movement, processing, sensory info, & visual perception. Plus visual spatial processing. Nonverbal memory. Emotion. Processing nonverbal auditory . |
|
|
What is rheumatoid arthritis? |
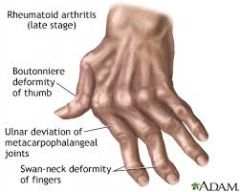
[Image] Rheumatoid arthritis is a systematic (i.e. methodical) and progressive condition. Rheumatoid arthritis flows to many joints, especially the HANDS. |
|
|
What does the root word -rheum (r.h.e.u.m.) mean? This makes up the word rheumatoid. |
"rheum" (r.h.e.u.m.) itself is a Greek word that means "flow." The word was first ascribed to the disease of rheumatism because of the way it seemed to spread — or flow — within a patient's body. |
|
|
Rheumatoid arthritis: There are 3 deformites common to rheumatoid arthritis. Describe the one that is not Boutonniere Deformity or Swan Neck Deformity |

[Image]
Ulnar deviation or ulnar drift and subluxation of wrists and MCP joints. |
|

Rheumatoid arthritis: Describe Boutonniere's Deformity. |
![Boutonniere Deformity is P.I.P. flexion & D.I.P. hyper-extension.
[HINT: Fingers positioned to adjust boutonniere flower, or if closed, to hold pin to pin it on.]](https://images.cram.com/images/upload-flashcards/30/15/35/9301535_m.jpg)
[Image] It is P.I.P. flexion & D.I.P. hyper-extension. [HINT: Fingers positioned to adjust boutonniere flower, or to hold pin to pin it on.] |
|

Rheumatoid arthritis: Describe Swan Neck Deformity. |

[Image]
Swan Neck Deformity is hyper-extention of the PIP, flexion of the DIP. |
|
|
What is osteo-arthritis? |
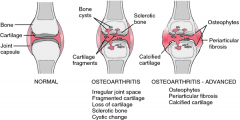
[Image] Osteoarthritis is a degenerative joint disease resulting from WEAR & TEAR. Commonly affects large, weight bearing joints. |
|
|
Joints of the hand: Name the abbreviations and full names for them. |
[Image] 1. D.I.P. is distal inter-phalangeal joint. 2. P.I.P. is proximal inter-phalangeal joint. 3. M.C.P. is meta-carpo-phalangeal joint. |
|
|
Name the bones of the hand. |
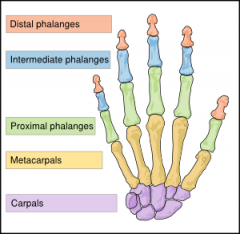
[Image] 1. Phalanges. Including distal, intermediate, and proximal. 2. Meta-carpals. 3. Carpals or carpal bones. |
|
|
S.C.I. - what does it stand for? |
S.C.I. stands for spinal cord injury. |
|
|
What is ortho-static hyper-tension? |
Orthostatic hypertension is a severe drop in blood pressure that occurs when someone assumes an upright position. |
|
|
What is spinal shock? |
Spinal shock, an issue in S.C.I., can occur during the first 4 to 8 weeks after a spinal injury. All reflex activity is gone below the level of injury, resulting in flaccid paralysis.
You have to let this run it's course BEFORE diagnosing. |
|
|
What is Osteo-genesis Imperfecta and what is the way to remember it according to it root words? |

[Image] Osteo-genesis Imperfecta is imperfect bone growth. [HINT: the short character on the show CARNIVAL has it.] |
|
|
Osteo-genesis Imperfecta: name some of the symptoms. |
Some of the symptoms of Osteo-genesis Imperfecta include:
1. Brittle bones that easily fracture.
2. Multiple fractures as a growing child.
3. Deformities of the arms and legs. |
|
|
What are some of the ways to medically manage Osteo-genesis Imperfecta? |
Osteo-genesis Imperfecta can be managed medically in these ways:
1. Casts and braces.
2. Pain management.
3. Activity restrictions. |
|
|
Amputation. Wrapping of residual limbs.
What is the proper way to wrap a residual limb and why? |
A limb should be wrapped diagonally. This keeps the limb from having circulation cut off. |
|
|
Amputation. Wrapping of residual limbs.
Why is it done and when should a limb have wrapping on it? |
Wrapping a residual limb keeps it from swelling and fits it for prosthesis.
A limb should be wrapped at all times. |
|
|
Amputation. Describe the nomenclature for the levels of amputation. |
1. Forequarter, which is the loss of clavicle, scapula, & entire upper extremity. 2. Disarticulation, which is the separation of 2 bones at the joint (like the wrist, elbow, hip, knee) 3. Trans, like trans-femoral, trans-humeral, trans-radial, and trans-tibial. 4. Finger amputation |
|
|
Amputation. What does treatment for the residual limb consist of? (One thing.) |
Treatment of the residual limb consists of desensitization as well as other really cool stuff. |
|
|
What is R.L.P. stand for? |
R.L.P. stands for residual limb pain. |
|
|
What is residual limb pain (R.L.P.)? |
R.L.P., or residual limb pain, is the pain that originates in the remaining part of your limb. (This is not Phantom limb pain.) |
|
|
What is phantom limb pain? |
Phantom limb pain is a sensation of pain perceived to originate from a body part that, in reality, is not there. |
|
|
What's another name for Total Hip Replacement? |
Another name for "Total Hip Replacement" is "Total Hip Arthroplasty". |
|
|
What are the types of "Total Hip Arthroplasty"? |
There are two types of "Total Hip Arthroplasty", as follows:
1. Total Hip Implant. Here they replace both the acetabulum and the femoral head.
2. The Austin Moore, or Partial Hip Replacement. Here they replace only the femoral head. |
|
|
What are the total hip precautions for a Total Hip Replacement? |
The total hip precautions for a Total Hip Arthroplasty are: 1. No flexing beyond 90 degrees. 2. No adducting or crossing legs. 3. No rotating hips, meaning don't point your toes inward or outward. ALSO: 4. No pivoting at the hips. 5. Sit only on a raised chair and toilet seat. 6. Transfer sit to stand by keeping the operated hip in slight abduction and extended out front. |
|
|
C.O.P.D. What does it stand for? |
C.O.P.D. stands for Chronic Obstructive Pulmonary Disease. |
|
|
What is C.O.P.D. and what is it caused by? |
C.O.P.D. is a lung disease that makes it difficult to breathe. It is caused by damage to the lungs over many years, usually from smoking. |
|
|
C.O.P.D. is usually a mix of what 2 diseases and describe those diseases? |
C.O.P.D. is usually a mix of chronic bronchitis and emphasema.
1. Chronic bronchitis is the airways that carry air to the lungs get inflamed and make a lot of mucus. This can narrow or block the airways, making it hard to breathe.
2. Emphasema is when the air sacs in the lung are damaged and lose their stretch. Less air gets in and out and makes you feel short of breath. |
|
|
What is the etiology of hip fractures? |
The etiology of hip fractures includes the following: 1. Trauma to the hip. 2. Osteoporosis. 3. Pathological fractures, for example from cancer. 4. More. |
|
|
What are the types of hip fractures? |
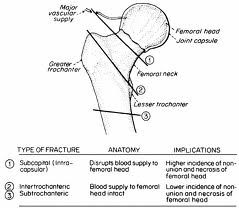
[IMAGE.] The types of hip fracture are. 1. Femoral neck fracture. 2. Inter-trochantric fracture. 3. Sub-trochantric fracture. |
|
|
What is the medical management of hip fractures and define all the parts of your answer? |
Hip fractures are medically managed in 3 ways: 1. Closed reduction. This is for minimally displaced fractures & is done without surgery. 2. O.R.I.F. Open reduction internal fixation. Open means surgery, reduction means returning the bone to its proper place, internal fixation means the bone is fixated to something internal. 3. Joint replacement. |
|
|
Hip fracture. What are the precautions? |
The precautions for hip fracture are determined by the surgeon. This includes the weight bearing status, amount of ROM, and when to begin OT. |
|
|
Edema. How is it best treated? |
Edema is best treated with elevation and A.R.O.M. |
|
|
Glasgow Coma Scale. What does it measure? |
The Glasgow Coma Scale is the most common scale used to determine the level of consciousness of a person after they've had a TBI. Basically, it's used the gauge the severity of an acute brain injury. |
|
|
Glasgow Coma Scale. What is the range for possible score and what do the highest and lowest scores mean? |
The scoring range for the Glasgow Coma Scale is from 3 to 15. A 3 means the person is in a deep coma or is dead. A 15 means fully awake. NOTE, therefore, that all component scores have a highest and lowest rating. A 1 for all of them means no response. Or this rhyme. . one is none. The highest score always means "normal". Just learn the middle scores. |
|
|
Glasgow Coma Scale. What are the different categories that are rated and added to determine a score. |

The categories rated for the Glasgow Coma Scale are:
1. eye opening. 2. verbal responses. 3. motor responses. |
|
|
Glasgow Coma Scale. How do you remember how many scores there are for each category? |
For eyes, think of the old nickname for kids with glasses. "4 eyes". . . For verbal responses, think that the word verbal starts with a V, which is roman for 5. For motor responses, think of a 6 cylinder engine. |
|
|
Glasgow Coma Scale. . Name all of the sub-ratings. |
Eye Opening (E). A score of 4 means eye opening is spontaneous. 3 is when they respond to voice. 2 is response to pain. 1 is none. Verbal Response (V). A 5 reflects normal conversation. 4 is disoriented, but coherent. 3 is words, but incoherent. 2 is only sounds, no words. 1 is none. Motor Response (M). A 6 is normal. 5 has the patient crossing mid-line to resolve a pain issue, like push an I.V. away. 4 means they withdraw from pain. 3 is decorticate posture, or flexion. 2 is decerebrate, or extenion. 1 is none. |
|
|
Glasgow Coma Scale. What do the final scores mean? |
Brain injury is generally classified as:
1. Severe, which is a score of 3 to 8.
2. Moderate. which is a score of 9 to 12.
3. Mild. which is a score of 13 to 15. |
|

What posture is this? |
Decordicate posture, in which the patient is in flexion. |
|

What posture is this? |
Decerebrate posture, in which the patient is in extension. |
|
|
What is C.R.P.S.? |
C.R.P.S., or CRAPS as I like to call it, is Complex Regional Pain Syndrome. |
|
|
What is neuro-pathic pain? |
Neuropathic can be broken down to "neuro-", or nerves, and "-pathic", which would mean disease. So neuro-pathic pain means pain that result from a messed up part of the nervous system.
Neuro-pathic pain is pain that results from lesions in some part of the nervous system. |
|
|
C.R.P.S. How many types of C.R.P.S. are there, name them, and describe them. |
There are 2 types of C.R.P.S.: Type 1 and Type 2. 1. Type 1 C.R.P.S. is pain characterized by abnormal burning pain & hypersensitivity to light touch. It's usually because of a traumatic injury. 2. Type 2 C.R.P.S. is pain occurring along the branches of a nerve. |
|
|
Tell me about shingles and what does it look like? |
Shingles, or Herpes Zoster, is characterized by vesicular eruption. It looks fairly like psoriasis. It can last 10 days to 5 weeks. Pain may persist for months. |
|
|
What is phantom limb pain? |
Phantom limb pain is pain experienced in a body part that is no longer there.
Phantom limb sensation is far more common. |
|
|
What is referred pain? |
Referred pain is pain that is perceived in part of the body when the source of the pain is in another part of the body. |
|
|
What is the full name of S.P.D.? |
S.P.D. is sensory processing disorder. |
|
|
S.P.D. What are some signs and symptoms of Sensory Processing Disorder? |
Signs and symptoms of S.P.S. include: 1. Hypo-sensitivity, sometimes called under-responsivity. 2. Hyper-sensitivity, sometimes called over-responsivity. 3. Tactile processing dysfunction. 4. Proprioceptive processing dysfunction. 5. Vestibular processing dysfunction. |
|
|
What is a seizure? |
A seizure is uncontrolled electrical activity in the brain that may result in physical convulsion, minor physical changes, thought disturbances, or a combo deal of these symptoms.
This depends on where the abnormal electrical activity takes place in the brain, what its cause is, and stuff like age and state of health. |
|
|
What are the intervention procedures if you are present when someone has a seizure? |
1. Remain calm. 2. Safety. Remove dangerous objects from area. 3. Safety. If person upright, gently glide them to floor and loosen clothes. 4. Safety. Turn him on his side to prevent chocking. |
|
|
What is the proper post-seizure care? |
Proper post seizure care includes: 1. Allow the individual to rest or sleep after seizure. 2. more stuff 3. Observe safety precautions is person seems groggy, confused, or weak following seizure. |
|
|
What are C.T.D., or cumulative trauma disorders, and name 3 examples of them? |
Cumulative trauma disorders are are a group of repetitive strain injuries. 3 examples are: 1. DeQuervains. 2. Epicondylitis, either lateral or medial. 3. Trigger finger. |
|
|
What is deQuervain's disease? |

Image. . A painful inflammation of tendons in the thumb that extend to the wrist. Swollen tendons & coverings rub against their narrow tunnel. The result is pain at the base of thumb, extending into lower arm. HINT: the quer wrist. |
|
|
What is the technical term for tennis elbow and what is it? |
Tennis elbow is lateral epicondylitis. This is an irritation through overuse of the wrist extensors. |
|
|
What is the technical term for golfer's elbow? |
Golfer's elbow is medial epicondylitis. This is over use of the wrist flexors. |
|
|
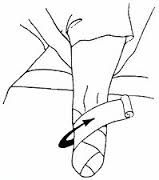
What is trigger finger? |
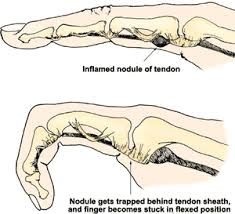
IMAGE. HINT. is obvious. Trigger finger is tenosynovitis of the finger flexors, especially the first. It's caused by repetition. |
|
|
What is carpal tunnel syndrome? |
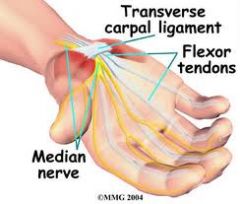
Image. Carpal tunnel syndrome is pain, tingling, and numbness in the hand (but not the pinky) that is a result of pressure on the median nerve. |
|
|
Name the nerves of the hand and what areas they are associated with. |
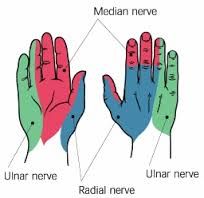
Image. The names of the nerves of the hand are median, ulnar, and radial nerves.
Please look at image for areas. |
|
|
Burns. What are the names of the different kinds of burns? |
To replace the old terms of 1st, 2nd, & 3rd degree burns, the terms are now superficial, partial thickness, and full thickness. Partial thickness was divided into 2, as follows: 1. Super-ficial burn. 2. Super-ficial partial thickness burn. 3. Deep partial thickness burn. 4. Full thickness burn. |
|
|
What is a superficial burn? |
A superficial burn used to be called 1st degree burn. It's the equivalent of a light burn with a curling iron. It involves only the superficial aspect of the skin organ, which is the epidermis.
There is minimal pain and edema, and there are no blisters. They heal in 3 to 7 days. |
|
|
Yo slappy, what is a partial thickness burn? |
A partial thickness burn is a 2nd degree burn. They are burns that extend down to the second layer of skin. into the dermis. (So they effect the epidermis and the dermis.) There are 2 kinds of partial thickness burns. superficial and deep. |
|
|
What is a superficial partial thickness burn? |
A superficial partial thickness burn is a more superficial 2nd degree burn. Its a burn that affects the superficial level of the second layer of skin, the dermis. It's red, blistering, and wet. It heals in 7 to 21 days. This would be a sunburn. |
|
|
What is a deep partial thickness burn? |
A deep partial thickness burn is a deep 2nd degree burn. It affects deep into the dermis and affects hair follicles and sweat glands. They are red, white, and elastic. They take 3 to 7 weeks to heal. |
|
|
What is a full thickness burn? |
A full thickness burn is a 3rd degree burn. In addition to the epidermis, dermis, hair follicles and sweat glands, this burn type effects nerve endings. They appear white, waxy, and leathery. There is no pain and skin grafts are required. Healing can take months. |
|
|
What is a 4th degree burn? |
A 4th degree burn involves fat, muscle, and bone. There is destruction of nerves along the pathway. Rule of nines is a method of assessing burn wound size. |
|
|
What is the rule of nines and what are its components? |
The rule of nines has the following measurements:
The head and arms are 9% each. The torso is 36%. The legs are each 18%. The pubic area i s1%
|
|
|
When a hand is burned and requires splinting, describe the position of the hand. (This doesn't include splinting for a burn on the volar, or palmer, surface of the hand, which is different.) |
1. the wrist in 20 to 30 degree extension. 2. MCP joints in 50 to 70 degree flexion. 3. IP joints in full extension. 4. Thumb abducted and extended |
|
|
Describe the position of a splinted hand that was burned on the volar side. |
The volar side is the palmer side. (Picture a Volare car in palm of hand with guy singing that song.) 1. Wrist in 0 to 30 degrees extension. 2. MCP joints in neutral and abducted. 3. IP joints in full extension. 4. Thumb abducted and extended.d |

