![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back
|
Tachypnea
|
Rapid breathing
|
|
|
Apnea
|
Absence of breathing
|
|
|
Hyperpnea
|
Breathing deeper and more rapid than normal
|
|
|
Hypercapnea
|
High levels of carbon dioxide in the blood
|
|
|
Hypoventilation
|
Decreased amount of air being moved in and out of lungs
|
|
|
Hyperventilation
|
Increased amount of air being moved in and out of lungs
|
|
|
Minute Volume
|
The amount of air moved in and out of lungs per minute
|
|
|
Respiratory Minute Volume
|
total volume moved in and out of lungs per minute
|
|
|
Alveolar Minute Volume
|
Amount of air available for gas exchange per minute
Minute ventilation = (tidal volume)(breaths/min) |
|
|
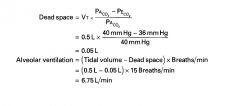
Dead Space
|
Regions of the respiratory system that contain air but are not exchanging °2 and CO2 with blood are considered dead space (conductive bronciholes)
|
|
|
Alveolar Ventilation
|
Alveolar Ventilation = (Tidal volume - dead space)(breaths/min)
|
|
|
Cardiac output =
|
heart rate x stroke volume
|
|
|
Resting Tidal Volume
|
500 ml
|
|
|
Average Volume of the anatomic Dead Space
|
150 ml
|
|
|
normal respiration rate
|
14-16 breaths per minute (15)
|
|
|
Alveolar Minute Volume
|
Breaths per minute x (volume per breath - anatomic dead space) = 15 x (500-150) = 5250 ml/minute
|
|
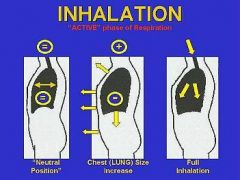
Steps in the Mechanics of Respiratoin
|
1. Ribs expand and diaphragm contracts (pleural volume increases, intra pleural pressure decreases)
2. Patm > Palv, alveolar volume increases as lungs expand thus decreasing the pressure in the alveoli below atmospheric pressure 3. As air enters lungs, increased volume of air raises pressure and when pressure in the alveoli = atmospheric presure than air flow ceases (Patm =Palv) 4. Reverse (ribs/diaphragm relax, decreases alveolar and pleural volume increasing pressure and forcing air out due to Patm < Palv) |
|

|

Mechanics of breathing
On inspiration, alveolar and pleural pressure decreases bc of increased surface area (Pressure = Force/Area); on expiration alveolar and pleural pressure increases due to decreased volume of the cavity which forces air out |
|
|
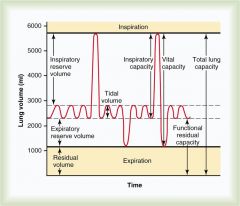
Residual Volume: Amount of air left in lungs after full exhalation
Tidal Volume: Air moved in and out during normal resting respiration Vital Capacity: Total amount of air the lungs can move in and out per breath |
|
|
How would left heart failure influence ventilation?
|
Left heart failure would result in pulmonary edema which would lead to fluid accumulation in the lungs. This would initially reduce ventilation that would lead to compensatory changes resulting in increased rate and depth of breathing
|
|
|
How would right heart failure influence ventilation?
|
Right heart failure would result in decreased blood flow to the lungs. This would initially reduce oxygen delivery and carbon dioxide removal which would lead to compensatory changes resulting in increased rate and depth of breathing
|
|
|
How would pulmonary edema affect ventilation?
|
Fluid would decrease the volume of the alveoli
Fluid would decrease gas exchange Fluid would alter the compliance of the lungs Fluid would affect ventilation/perfusion ratio |
|
|
How would muscle pathologies influence ventilation?
|
Decreased muscle function would lead to the inability to change volumes of the chest cavity as the ribs or diaphragm would either be more difficult to move or not move at all; (paralysis, guillain barree syndrome, myasthenia gravis, neurological disorders or poisons)
|
|
|
How will obstructive lung blockage affect volume and capacities?
|
Increase residual volume
|
|
|
How will restrictive lung disease affect lung volumes and capacities?
|
Decrease total lung capacity
|
|
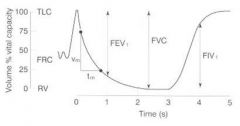
FEV1
|
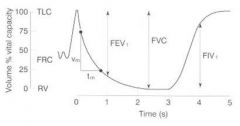
Volume of air that can be expired in the first second of forced maximal expiration; it's normally 80% of the forced vital capacity
FEV1/FVC = .8 |
|
|
Tidal Volume
|
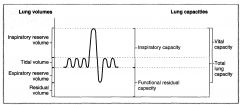
Volume inspired or expired with each normal breath
|
|
|
Inspiratory Reserve Volume
|
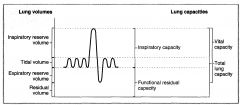
Volume that can be inspired over and above the tidal volume; is used during exercise
|
|
|
Expiratory Reserve Volume
|
Volume that can be expired after the expiration of tidal volume
|
|
|
Residual Volume
|
Volume that remains in the lungs after a maximal expiration; cannot be measured by spirometry
|
|
|
A person with a tidal volume (Vt) of 0.5L is breathing at a rate of 15 breaths/min. The PC02 of his arterial blood is 40 mmHg, and the PC02 of his expired air is 36 mmHg. What is his rate of alveolar ventilation?
|
|
|
|
Inspiratory Capacity
|
Sum of tidal volume and IRV
|
|
|
Functional Residual Capacity
|
Sum of ERV and residual volume
Volume remaining in the lungs after a tidal volume is expired Includes the residual volume so it CANNOT BE MEASURED BY SPIROMETRY |
|
|
Vital Capacity/Forced Vital Capacity
|
Sum of the tidal volume, IRV, and ERV; volume of air that can be forcibly expired after a maximal inspiration
|
|
|
Total Lung Capacity
|
Sum of all four lung volumes; volume in the lungs after a maximal inspiration; includes residual volume, so it cannot be measured by spirometry
|
|
|
How would asthma affect FEV1?
|
In obstructive lung diseaes, FEV1 is reduced more than FVC so that FEV1/FVC is decreased
|
|
|
How is FEV1 affected in fibrosis?
|
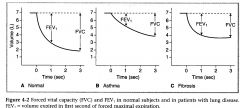
In restrictive lung disease, both FEV1 and FVC are reduced and FEV1/FVC is either normal or is increased
|
|
Dorsal Respiratory Group
|
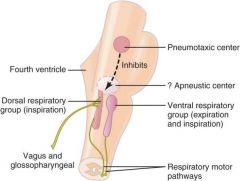
Inspiration; generates the basic rhythm for breathing
Input: Vagus and glossopharyngeal Output: Phrenic nerve to diaphragm |
|
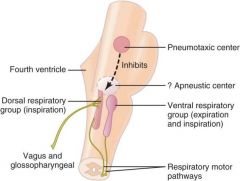
Ventral Respiratory Group
|
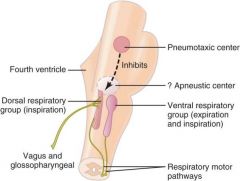
Expiration; not active during passive breathing; activated during exercise when expiration becomes an active process
|
|
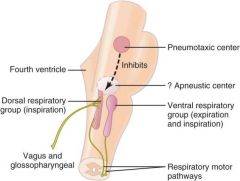
Apneustic Center
|
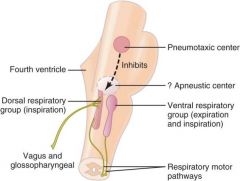
Stimulates inspiration, producing deep/prolonged inspiratory gasps (apneusis)
|
|
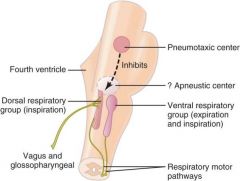
Pneumotaxic Center
|
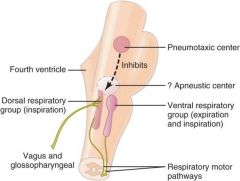
Upper pons
Inhibits inspiration; regulates inspiratory volume and respiratory rate |
|
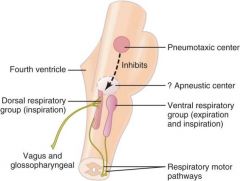
Hering-Bruer Inflation Reflex
|
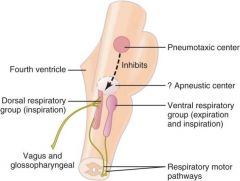
Prevents overinflation of lungs; stretch receptors in smooth muscle of bronchi/bronchioles send inhibitory signal through vagus to DRF/apneustic center
|
|
|
Where are dentral chemoreceptors located?
|
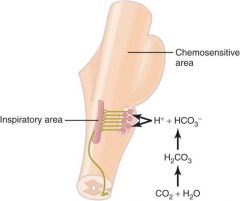
Medulla; must occur IN THE CSF
CO2 crosses BBB, reacts with water to decrease pH |
|
|
Neural Effects of H+ and C02
|
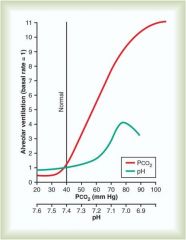
Increased PC02 = increased ventilation
|
|
|
Where are peripheral chemoreceptors located?
|
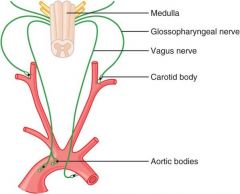
Cartid bodies located at bifurcation of common carotids
Aortic bodies located above and below the aortic notch |
|
|
relatoinship between arterial P02 and breathing rate
|
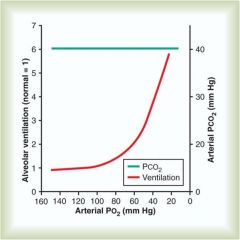
Decreases in arterial P02 stimulate peripheral chemoreceptors and increase breathing rate; when P02 decreases below 60 mmHg breathing rate rapidly increases
|
|
|
Increases in arterial PC02
|
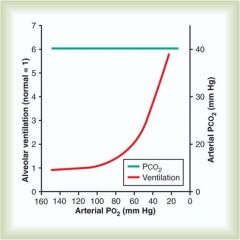
Stimulate peripheral chemoreceptors and increase breathing rate; potentiate stimulation of breathing caused by hypoxemia
|
|
|
How is venous PC02 affected by exercise?
|
Increases during exercise bc excess C02 produced by exercising muscle is carried to the lungs in venous blood
|
|
|
How is dead space affected by exercise?
|
pulmonary blood flow increases because cardiac output increase during exercise. As a result, more pulmonary cpaillaries are perfused and more gas exchange occurs.
The distribution of V/Q ratios throughout the lung is more even during exercise then when at rest, thus there is a decrease in physiologic dead space. |
|
|
Cheyne-Stokes Breathing Explained
|
When a person overbreathes, thus blowing off too much carbon dioxide from the pulmonary blood while at the same time increasing blood oxygen, it takes several seconds before the changed pulmonary blood can be transported to the brain and inhibit the excess ventilation. By this time, the person has already overventilated for an extra few seconds. Therefore, when the overventilated blood finally reaches the brain respiratory center, the center becomes depressed an excessive amount. Then the opposite cycle begins.
|
|
|
Sleep Apnea
|
Loud snoring/labored breathing after falling asleep; snoring interrupted by long silent period during which no breathing occurs; periods of apnea result in significant decreases in P02 and increases in PC02, which stimulate respiration -> sudden attempts to breathe (loud snorts, gasps, followed by snoring and repeated episodes of apnea)
|
|
|
Daltons Law of Partial Pressures
|
Partial pressure = (total pressure)(fractional gas concentration)
|
|
|
Pressure of air around us
|
760 mmHg
|
|
|
Assume that total pressure is atmospheric and the fractional conc. of 02 is 0.21. What is the partial pressure of dry inspired air (P02)?
|
P02 = 760 mmHg x 0.21 = 160 mmHg
|
|
|
Why must the total pressure be modified for tracheal air?
|
Tracheal air is humidified (H20 vapors) at 37C and thus the calculation is modified to correct for the partial pressure of H20, which is 47 mmHg
P tot = (760 mmHg - 47 mmHg = 713 mmHg P02 (tracheal) = (713)(.21) = 150 mmhg |
|
|
Physiologic shunt
|
2% of the systemic cardiac output bypasses the pulmonary circulation; the resulting admixture of venous blood w oxygenated arterial blood make sthe P02 of arterial blood slightly lower than that of alveolar air
|
|
|
Why is the partial pressure of P02 decreased to 100 and the PC02 increased to 40 in alveolar air?
|
P02: 02 has diffused from alveolar air into pulmonary capillary blood, decreasing the P02 of alveolar air
PC02: C02 has been added from pulmonary capillary blood into alveolar air |
|
|
What does putting oxygen on a pt who is saturating at 100% do?
|
Increase dissolved oxygen (which is normally about .3 ml 02/100ml blood
|
|
|
What things shift the Hb-02 curve to the right
|
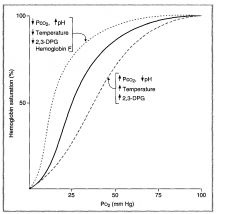
Right shifts occur when the affinity of Hg for 02 is decreased; facilitates unloading of 02 from arterial blood to tissues
|
|
|
What things shift the Hb-02 curve to the left
|
Left shifts occur when the affinity of Hg for 02 is increased (high Hg sat at lower P02)
|
|
|
What is the difference in P02 between alveolar air and systemic arterial blood (pulmonary capillaries)?
|
No difference; they are equilibrated at 100
|
|
|
What is the difference between PC02 in alveolar air vs systemic arterial blood (pulmonary capillaries)?
|
No difference; they are equilibrated at 40
|
|
|
What is the main form of C02 transport in the blood?
|
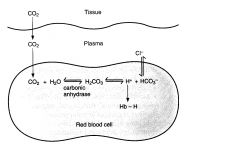
HC03 (from hydration of C02 in the rBCs); 90%
|
|
|
Carbonic Anhydrase
|
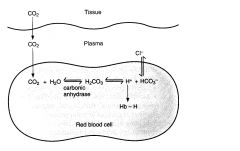
Hydrates C02 in RBCs to form HC03 + H
|
|
|
Chloride Shift
|
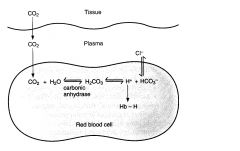
HC03 leaves RBCs in exchange for Cl- and is transported to the lungs in the plasma (HC03- is major form in which C02 is transported to the lungs)
|
|
|
What buffers H+ inside RBCs?
|
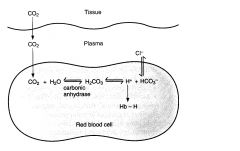
Deoxyhemoglobin
|
|
|
What happens to C02 once it is in the lungs?
|
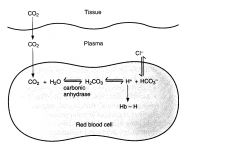
All the tissue reactions occur in reverse
HC03- enters RBCs in exchange for Cl-. HC03 recombines with H+ -> H2C03 which decomposes into C02 and H20; thus C02 generates in the tisuses is expired |
|
|
Why is there a slight left shift in CO poisoning?
|
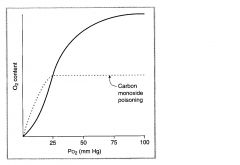
Binding of CO to Hg increases the affinity of remaining sites for 02, causing a shift of the curve to the left
|
|
|
How does a physiologic shunt affect V/Q?
|
V/Q < normal
Low ventilation |
|
|
How does a physoilogic dead space affect V/Q?
|
V/Q > normal
Wasted ventilation |
|
|
Where in the lung is V/Q/ highest?
|
At the apex (top of the lung); P02 is highest and PC02 is lower bc there is more gas exchange (bc blood flow is slowest here)
|
|
|
Where in the lung is V/Q lowest?
|
At the base (base of the lung)
P02 is lowest and PC02 is higher bc there is less gas exchange |
|
|
Acidemia
|
Condition that results in a lower than normal pH (7.1-7.3), <7.1 = fatal
|
|
|
Alkalemia
|
Higher than normal pH, 7.44-7.69, >7.70 can be fatal
|
|
|
Acidosis
|
A condition that adds acid to the blood or removes bases from the blood
|
|
|
Alkalosis
|
A condition that adds bases to the blood or removes acids from the blood
|
|
|
Respiratory Acidosis
|
Respiratory acidosis is a condition that occurs when the lungs cannot remove all of the carbon dioxide the body produces. This disrupts the body's acid-base balance causing body fluids, especially the blood, to become too acidic; can be caused by an increased rate of respiration (short trip to higher elevation, hyperventilation, respiratory stimulants)
Kidneys will increase bicarbonate secretion to balance |
|
|
Respiratory Alkalosis
|
Respiratory alkalosis is a condition marked by low levels of carbon dioxide in the blood due to breathing excessively.
can be caused by anxiety, fever, hyperventilation |
|
|
A 6 year old child is seen in the emergency room. He is wheezing and has a bluish hue to the mucosal membranes. His mother indicates the child has been diagnosed with asthma. Does the child have respiratory acidosis or alkalosis?
|
Acidosis (not blowing off their C02?
|
|
|
A 55 year old man is seen in the internal medicine clinic. His major compliant is shortness of breath, a condition that has become progressively worse over the last 5 years. He is a 2 pack a day smoker. Stat labs reveal the following:
Plasma concentrations HCO3- = 40 meq/l K+ = 4.5 meq//l HCT = 45+ Hb = 12 mg/dl Plasma protein 6.0/dl Glucose = 80 mg/dl BUN = 12 mg/dl Creatinine = 1.4 mg/dl Arterial PCO2 = 70 mmHg pH (arterial) = 7.35 Does he have respiratory acidosis or alkalosis? |
Acidosis (not blowing off his C02)
|
|
|
A 23 year old woman is in the delivery room. She is in hard labor. Her Lamaze coach has instructed her to “puff and blow” when the labor pains become intense. She was told to bring a small paper bag with her to breathe into during the labor pains. The purpose of the bag is to prevent her form developing respiratory acidosis or alkalosis?
|
Respiratory alkalosis; she hyperventilates, is not blowing off C02 and thus becomes mroe acidic, preventing respiratory alkalosis
|
|
|
What side chain on hemoglobin and albumin allows them to function as protein buffers?
|
Histidine; these residues can donate and accept H+ at physiologic pH making them good buffering agents
A buffer functions effectively within one pH unit of its pKa |

