![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back

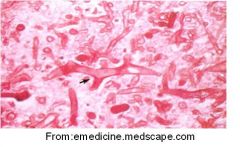
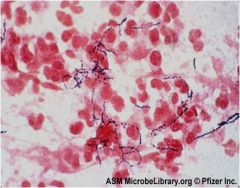
A 42-year-old woman presents to ED with a 2 week history of dry cough and 1 day history of fever, vomiting, headache. 3 days earlier, the patient had seen her GP, who made a provisional diagnosis of bronchitis and prescribed antibiotics in case she did not improve. She took one dose of antibiotic but then started vomiting. Her past history included a splenectomy at 19 years of age following a car accident. On exam, she looks unwell. Her temperature is 39.2, pulse100/min, BP 100/70 and RR 20/min. There are bilateral chest crepitations. Marked neck stiffness is present. A presumptive diagnosis of septicemia/pneumonia/meningitis is made.* Blood cultures are drawn and intravenous antibiotic therapy is initiated. The organism later isolated from her blood cultures is shown.
1. causative organism 2. why is the pt immunocompromised 3. why did the pt get this particular organism |
1. strep pneumoniae
2. splenectomy, acquired immune deficiency 3. phagocytosis of this organism is inefficient due to its capsule; phagocytosis is further compromised by lack of spleen, which has many residency phagocytes |
|
|
Opportunistic Infection
|
Infectoin caused by microbe that does not usually cause disease in a healthy person
|
|
|
Immunocompromised patient
|
Immune deficient due to primary (genetic, rare) or secondary (acquired, more common) immune defect
|
|
|
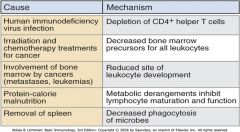
Describe some common causes for acquired immune deficiencies
|
|
|
|
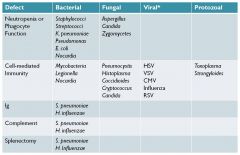
Immunocompromised pneumonia associated opportunistic pathogens
|
|
|
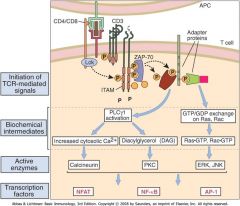
How does cyclosporine affect the immune system?
|
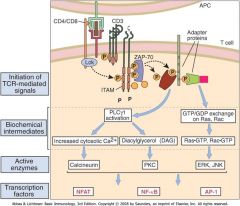
Inhibits T cell activation by antigen (inhibits NFAT activation)
|
|
|
Why does pneumocystis jiroveci cause pneomoniae in immunocompromised patients?
|
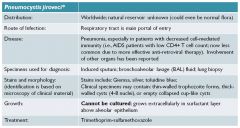
Pneuocystis inactivates macrophages, which are needed to kill p. jiroveci
|
|
|
Why does Nocardia cause disease in immunocompromsied patients?
|
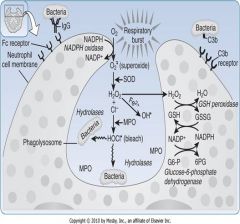
Cord factor -> inhibits phagosome-lysosome fusion; seen in pts with decreased cell mediated immunity (can't activate phagocytes) and pts with neutropenia or decreased phagocyte funcction
Avoids phagocytic killing by secreting dismutase (converts superoxide to H202) and catalase (breaks down H202) |
|
|
Why does Aspergillus cause dz in immunocompromised pts?
|
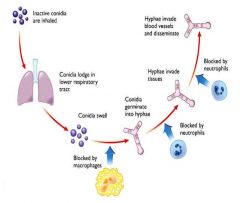
Major predisposing factor for highly invasive disseminated asperillosis is neutropenia
|
|

|
Rhizopus'; rapidly progressiv epulmonary dz in pts immunocompromised by malignancy
|
|

Why does Rhizopus cause mucormycosis in immunocompromised pts?
|
Major predisposing factors:
- neutropenia (usually caused by leukemia or chemotherapy) - diabetes (especially during ketoacidosis or in transplant patients with diabetes mellitis) - steroids |
|
|
Rhizopus; long sporangiophores (stalks) with terminal bulbs bearing sporangiospores, root like strutures caled rhizoids may be present; broad ribbon like sparsely septate twisted hyphae with branches that form right angles
|
|
|
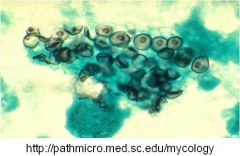
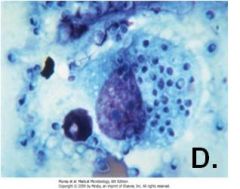
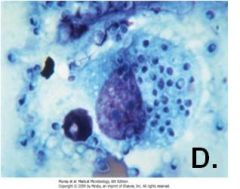
Pneuomocystis jireoveci; thin walled trophozoite forms thick walled cysts or empty collapsed cup like cysts
CANNOT be cultured; grows extracellularly in surfactant layer above alveolar epithelium |
|
|
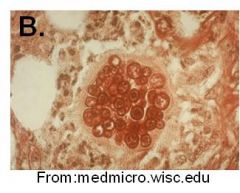
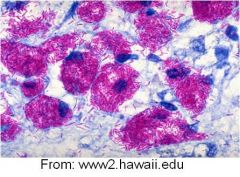
PAS stain of lung biopsy showing a spherule of coccidiodes immitis (San Joaquin Valley Fever); inhaled arthroconidia grow into spherules
|
|
|
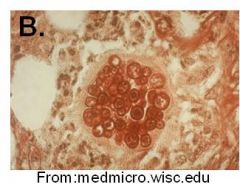
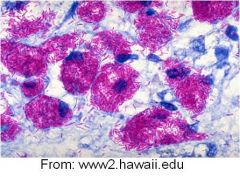
Wright's stain of Cryptococcus neoformans showing budding yeast inside large capsules; dx by demonstration of yeast w large capsule on routine stain or india ink prep; diagnostic test for cryptococcal antigen
|
|
|
Histoplasma capsullatum; dx by isolation and culture or by ag detection in blood or urine
|
|
A 63-year-old female patient was diagnosed with seropositive rheumatoid arthritis (RA). ). Long-term treatment with prednisone failed and she was placed on anti-TNF therapy in combination with methotrexate* (MTX). Her chest x-ray was normal before the start of this new treatment. Eight months later, this treatment was stopped due to occurrence of pulmonary and subcutaneous nodules. Gram stain of sputum and pus from skin nodules revealed gram-positive filamentous bacilli that were weakly acid-fast (see figure).
|
Nocardia asteroides; Immunocompromised by steroid tx (decreased phagocyte function), MTX (suppress bone marrow), anti-TNF therapy (mechanism unknown)
|
|

A 47-year-old non-diabetic male patient received heart transplantation as treatment for dilated cardiomyopathy. Prophylaxis against CMV was given, as well as cyclosporine and steroids to prevent rejection. Two months later he developed dyspnea, cough, purulent sputum and a fever of 38.5oC. Despite treatment with ceftriaxone the patient’s dyspnea progressed, requiring increasing support with oxygen. Radiograph of the chest revealed pulmonary infiltration and a cavity lesion in the superior lobe of the right lung. Cultures of sputum and bronchioalveolar lavage (BAL) washings rapidly grew colonies of mold. Lactophenol cotton blue staining of material from these colonies showed long conidiophores with terminal vesicles bearing conidia in chains.
|

Aspergillus fumigatus; caused by neutropenia and diminished macrophages caused by steroids and lack of cytokines from T cells;
differs from Rhizopus from arrangement of spores (chains vs in a sac); hyphae branch differently (45 vs 90 degree angles) |
|
|
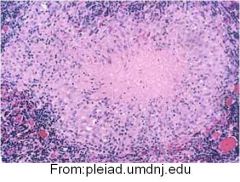
TB Granuloma; Full activation of macrophages requires IFN-gamma from CD4+ TH1 T cells which surround the granuloma
AIDS pts with low CD4+T cell counts are at very high risk for TB |
|
|
Mycobacterium avium intracellulare complex (MAC) in aids; hallmark of MAC infection in HIV pts in abundant acid fast bacilli within macrophages
|

