![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
two-year-old with acute onset altered mental status
|
(AEIOU) plus TIPS” causes of altered mental status:
Alcohol, ingested toxins Epilepsy, encephalitis, endocrine, electrolytes Infection, insulin Overdose, opiates, oxygen deprived Uremia (renal failure) Trauma, temperature Insulin, infection Psychosis Stroke, shock, space occupying lesions |
|
|
likely from the ddx
|
temperature is only mildly elevated, but tachycardia and hypotension raise concern for infection
Acute onset of altered mental status in a previously healthy child raises suspicion for ingestion, despite parental report non-accidental trauma |
|
|
unlikely from the ddx
|
not
history of alternating agitation and unresponsiveness is atypical for seizure. A metabolic disorder would most likely have previous episodes or history of recent illness preceding this episode of altered mental status. An intracranial mass would most likely present as gradual onset of signs and symptoms |
|
|
possible medication ingestions
|
hypoglycemia at presentation and her great aunt’s history of diabetes strongly suggest an ingestion of an anti-hyperglycemic agent. The great-aunt probably takes a medication like a beta blocker for her hypertension. Older adults can suffer from chronic pain and, in addition to acetaminophen and ibuprofen she could have opioids like codeine in the home. Many adults are treated with antidepressants after the death of a spouse. She could have also been prescribed a sedative-hypnotic medication. She may also be taking antihistamines or decongestants for her allergies.
|
|
|
Cholinergic: (organophosphates)
|
Miosis and blurred vision
Increased gastric motility (nausea, vomiting, diarrhea) Excessive tearing, salivation, sweating and urination Bronchorrhea and bronchospasm Muscle twitching and weakness Bradycardia Seizures and coma "SLUDGE": Salivation, Lacrimation, Urination, Defecation, GI mobility, Emesis. |
|
|
Anticholinergic: (diphenhydramine, tricyclic antidepressants)
|
Mydriasis (dilated pupils) "blind as a bat"
Dry skin "dry as a bone" Red skin (flushed) "red as a beet" Fever "hot as Hades" Delirium and seizures "mad as a hatter" Tachycardia, Urinary Retention, Ileus |
|
|
Sedative-Hypnotic:(benzodiazepines, barbiturates)
|
Blurred vision (miosis or mydriasis)
Hypotension Apnea and bradycardia Hypothermia Sedation, confusion, delirium, coma |
|
|
Opioids: (codeine, morphine, heroin)
|
Miosis (constricted pupils)
Respiratory depression Bradycardia and hypotension Hypothermia Depressed mental status (sedation, confusion, coma) |
|
|
Sympathomimetics: (cocaine, amphetamines, pseudoephedrine)
|
Mydriasis
Fever and diaphoresis Tachycardia Agitation and seizures |
|
|
dialated pupils?
|
anticholinergic or sympathomimetics may cause mydriasis, Diphenhydramine is an anticholinergic and pseudoephedrine is a sympathomimetic.
Miosis or constricted pupils= cholinergics and opiods, in this case codeine. Lorazepam, a benzodiazepine, may cause nystagmus, Acetaminophen and Aspirin do not cause ocular findings. |
|
|
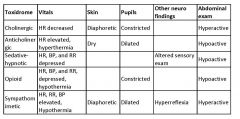
Ingestions table
|
|
|
|
mydriasis, tachycardia, agitation, hypotension and sedation
|
Tricyclic antidepressant
Selective serotonin reuptake inhibitor (SSRI) Antihistamine Decongestant oral hypoglycemic |
|
|
iron presents with
|
severe abdominal symptoms followed by signs of shock.
|
|
|
An ingestion of a beta-blocker to treat hypertension causes
|
bradycardia.
|
|
|
An ingestion of acetaminophen
|
initially presents with minimal symptoms (though gastrointestinal symptoms are not uncommon) followed by symptoms of liver toxicity.
|
|
|
An ingestion of aspirin
|
does present with agitation and tachycardia but there is no mydriasis.
|
|
|
An ingestion of an opioid or sedative-hypnotic causes
|
sedation and constricted pupils.
|
|
|
Tricyclic ingestion
|
Agitation, cardiac manifestations (especially hypotension), dilated pupils and dry, hot skin are classic findings in TCA ingestions
SSRI antidepressants are more commonly prescribed than tricyclic antidepressants, but there is data that older adults tolerate TCAs better and they are more effective for severe depression. |
|
|
SSRI OD
|
SSRI antidepressant requires a significant overdose to cause toxicity. These overdoses cause a serotonin syndrome. The serotonin syndrome presents with
profuse sweaty skin, agitation, fever, mental status changes, diarrhea, myoclonus, hyperreflexia, ataxia and shivering. |
|
|
overdose of a decongestant results in a
|
sympathomimetic toxidrome. This presents with tachycardia and hypertension, as well as agitation, sweating, fever, mydriasis and seizures.
|
|
|
Antihistamine ingestions present with
|
anticholinergic effects, much like those in TCA ingestions. TCA ingestions have additional mechanisms that cause unique cardiac manifestations.
|
|
|
TCA ingestion mechanism
|
inhibit synaptic reuptake of norepinephrine and serotonin (altered mental status),
antagonize muscarinic acetyl choline receptors (anticholinergic effects), peripheral alpha receptors (hypotension), result in sodium channel blockade (dysrhythmias) block GABA receptors (seizures) Clinically patients present with an altered mental status, anticholinergic signs and symptoms, hypotension (a hallmark of TCA toxicity), dysthythmias and seizures. Hypotension stems from direct myocardial depression from sodium channel blockade, and especially peripheral vasodilatation from alpha-1 adrenergic blockade. Refractory hypotension is the most common cause of death from TCA overdose. |
|
|
labs to order for toxicity
|
Continued monitoring serum glucose
Octreotide, a somatostatin analog inhibits insulin release and may be indicated as an antidote in dextrose refractory sulfonylurea overdose. CBC evidence against infection. Electrolytes and a blood gas can be used to identify metabolic acidosis/anion gap – characteristic of aspirin/NSAID toxicity. EKG since tachycardic and tricyclic anti-depressant ingestions can cause serious dysrhythmias. Abnormal levels of Calcium can also affect her heart. A toxicology screen from the urine or blood should be done to confirm, results not immediately available, but obtain the sample early. An acetaminophen level should be ordered since acetaminophen toxicity initially presents with minimal symptoms. It is the most common accidental ingestion LFTs and a urine analysis are of low yield in this case. Infection is low on the differential; there is no indication for a blood culture or lumbar puncture at this time. A CT scan of the head is mandatory for a child with altered mental status and agitation, but there is no historical nor clinical evidence for an intracranial mass lesion or increased intracranial pressure. Some physicians would order a head CT but it would have a very low yield. The same can be said for a chest x-ray. Madelyn has no localizing signs on her chest exam. |
|
|
enhance toxin elimination
|
syrup of ipecac, activated charcoal, gastric lavage, cathartics, hemodialysis and hemoperfusion.
Specific agents may have additional methods such as urinary alkalinization for salicylate intoxication. |
|
|
activated charcoal
|
ndicated for ingestions not due to small molecules or heavy metals. It is contraindicated in a patient with a loss of protective airway reflexes due to the risk of aspiration. Elective intubation should be considered for Madelyn. Additional doses of activated charcoal may be indicated due to decreased gastrointestinal motility as a result of the anticholinergic effects of tricyclics. A single dose of a cathartic agent may be given with the initial dose of charcoal.
|
|
|
Gastric lavage
|
has not demonstrated consistent clinical benefit.
One adult study demonstrated improved clinical outcomes within one hour of a tricyclic ingestion. It would be technically difficult to a pass a large enough tube in a two-year-old child. |
|
|
Hemodialysis and hemoperfusion
|
not indicated due to the high level of protein binding of tricyclics.
|
|
|
Syrup of ipecac
|
contraindicated in our patient due to a risk of aspiration with an altered mental status and potential for serious cardiac side effects and seizures. The AAP recommends that syrup of ipecac not be used as first line therapy for ingestions due to potential side effects.
|
|
|
cardiac tox of TCA ingestion
|
Cardiotoxicity primarily responsible for most morbidity and mortality in TCA overdose.
The wide-ranging effects on neurotransmitters and myocardial cells, including the cardiac conduction system, account for the triad of conduction delays, dysrhythmias, and hypotension. results from TCA effects on the myocardial action potential, direct effects on peripheral vascular tone, and effects mediated by the autonomic nervous system. Sodium channel blockade affects the His-Purkinje conduction system as well as myocardial cells = increased PR interval, QRS widening, and QT interval prolongation (the last can predispose to torsades de pointes, although uncommon). Sinus tachycardia from peripheral muscarinic antagonism and the inhibition of norepinephrine reuptake wide-complex tachycardia is the characteristic life-threatening dysrhythmias seen with severe TCA toxicity. In addition to the effects on neurotransmitters and sodium channel blockade, hypoxia, tissue ischemia, and metabolic acidosis may predispose the heart to ventricular tachycardia. The wide-complex tachycardia seen with TCA toxicity, however, is often not ventricular tachycardia, but sinus tachycardia with a wide QRS / aberrant conduction. slow, wide-QRS idioventricular rhythm is usually pre-terminal. QRS duration of >100 msec is associated with an increased risk of serious toxicity, including seizures, coma, hypotension, and dysrhythmias. The terminal 40 msec of the QRS has been touted as an important measurement for risk stratification, but this is not easy to measure. Qualitatively, it is manifested as a negative deflection (terminal S wave) in I and aVL, and a positive deflection (terminal R wave) in aVR. NB: This is not the same as the QRS axis. (triad = conduction delays, dysrhythmias, and hypotension) |
|
|
management TCA ingestion
|
Continuous cardiac monitoring and serial EKG’s
Most develop major clinical toxicity within several hours of presentation tx for cardiotoxicity (triad = conduction delays, dysrhythmias, and hypotension)= serum alkalization and sodium loading indicated for: QRS > 100msec, Rwave in AVR > 3mm, wide complex tachycardias, fluid refractory hypotension and seizures. serum pH affects protein binding of TCA’s, and metabolic acidosis can depress cardiac function. Hypertonic sodium bicarbonate is given as a 1 mEq/kg bolus initially and every three to five minutes until the QRS narrows and hypotension improves. target serum pH is 7.50-7.55, and close monitoring of blood gases Serum alkalization is continued for 12-24 hours after the EKG normalizes, because of the drug’s redistribution from the tissues. For life-threatening dysrhythmias, lidocaine can be administered. Class IA antiarrhythmic drugs, which are sodium channel blockers, are contraindicated Class III antiarrhythmic drugs (which can prolong the QT interval) may also be contraindicated. For hypotension, beta-adrenergic agonists and dopamine are contraindicated. Volume expansion, and serum alkalization and sodium loading are the mainstays of therapy, while norepinephrine may be used in refractory situations (0.1-0.2 mcg/kg/min). Seizures are generally brief. In addition to alkalinization, benzodiazepines, barbiturates or propofol may be used Phenytoin use is controversial and is usually not indicated due to its potential for cardiac toxicity. |

