![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
24 Cards in this Set
- Front
- Back
|
Where is the vomit coming from?
Undigested food: Digested food: Bile: Blood: Feculent: |
Undigested food: Esophageal or gastric origin
Digested food: Gastroduodenal origin Bile: Postampullary origin Blood: Above the ligament of Treitz Feculent: Bacterial overgrowth, colon, necrotic bowel |
|
|
nml newborn feeding and stooling
what's a temp? |
breastfed infant initially stools approximately 6 to 8 times per day, although this number often decreases by 1-2 months of age
4-week-old will typically breastfeed every 2 to 4 hours for 10 to 15 minutes on each breast. The infant may sleep up to 5 hours at a time during the night rectal temperature above 100.4 F (or more than 38 C) is considered a fever |
|
|
dehydration may include
|
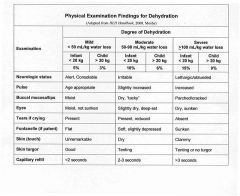
decreased activity level, decreased urine output and increased thirst (in children old enough to indicate thirst). Signs may include tachycardia, tachypnea (if associated with acidosis) weight loss, decreased production of tears, tacky or “dry” mucous membranes, sunken fontanelle and delayed capillary refill. Hypotension and loss of skin turgor (e.g., skin tenting) may be seen with severe dehydration.
Comparing current dehydrated weight to a previous euvolemic weight is a useful and simple way to determine the percent of weight loss and the degree of dehydration. |
|
|
Gravida, Para
|
total # of preg including abortions
viable infants at least 500g and 20wks given birth to regardless if they are alive (multiple birth is one parous event) |
|
|
Apgar
|
assess if child needs ressus
heart rate, resp effort, muscle tone, response to nasal suctioning, color not predict neonatal mortality, cerebral palsy, or cog development |
|
|
GE reflux
|
vomiting no bile
decreased PO b/c post paranial pain |
|
|
pyloric stenosis
|
escalating pattern of forceful nonbilious vomiting
vigorous appetite Hypertrophic pyloric stenosis male:female ratio 4:1 most common reason for an abdominal operation in the first 6 months of life > in northern Europeans, < in African-Americans, very rare in Asians. aggregate in families, esp children of an affected mother higher incidence in infants with blood O or B. vomiting starts at 3-4 weeks of age, but symptoms may develop as early as 1 week of age and as late as 3 months almost never symptomatic in the newborn nursery vomiting may have variable force, but classically projectile immediately after feedings as the pylorus becomes progressively more obstructed nonbilious. no Fever nor diarrhea Appetite initially preserved, though severely dehydrated =lethargy and decreased feeding palpating the pyloric mass (firm, mobile, 2 cm, olive shaped, in the midepigastrium above and to the right of the umbilicus); easier to palpate after vomiting when the musculature more relaxed. jaundice may be associated with pyloric stenosis significant electrolyte abnormalities assc w continuous vomiting hypochloremic metabolic alkalosis, due to the loss of hydrochloric acid in the vomitus. Na low K nml dx w Pyloric ultrasound GI study w contrast if no experienced US-er= very narrow pyloric channel (sometimes referred to as the string sign), indentation of the hypertrophied pylorus on the antrum of the stomach, and delayed gastric emptying |
|
|
CNS disease
|
must be considered in vomiting w/o fever or diarrhea
includes nonaccidental trauma |
|
|
enteritis
|
diarrhea may be absent early in the course but is there if it is true enteritis
nonbilious vomiting fever decreased PO |
|
|
SBO
|
vomiting (bilious below the ligament of Treitz)
decreased PO no fever or diarrhea |
|
|
metabolic disorders
|
vomiting
diminished PO due to lethargy and irritability |
|
|
UTI
|
vomiting (nonGI)
decreased PO fever diarrhea |
|
|
new born screening
|
All state programs: PKU and congenital hypothyroidism. More than 40 programs screen for sickle cell disease, and 48 screen for galactosemia.
Some: congenital adrenal hyperplasia, homocystinuria, maple syrup disease and biotinidase deficiency A few: cystic fibrosis and tyrosinemia |
|
|
signs of dehydration
|
decrease in weight and tachycardia are early indicators of dehydration, and that a drop in blood pressure is associated with severe dehydration
|
|
|
weight gain is expected per day in a 4-week-old infant?
|
5-30 grams (0.5 - 1 oz)
|
|
|
adventitious sounds
|
abnml sounds
|
|
|
diarrhea
|
diarrhea is a change in stools, usually defined as a passage of loose or watery stools. It may also be defined as excessively frequent stools or increased volume. The average stool output for a child is about 100 grams per day. Objectively, diarrhea is defined as stool output greater than 10 grams/kg/day in children who weigh less than 20 kg, or 200 grams total in 24 hours in children weighing more than 20 kg.
infxn most common cause of acute diarrhea leading cause of death in children second common cause of death world wide (children and elderly in developing countries from dehydration |
|
|
acute vs. persistent vs. chronic diarrhea
|
Acute diarrhea lasts less than 14 days;
"persistent" diarrhea lasting more than 14 days chronic- longer than 1 month Important clinical history includes the onset of illness, duration of symptoms, weight loss, whether contacts are sick, history of traveling to an endemic area, exposure to an untreated water, medication use and daycare attendance. phys exam: dehydration and signs of systemic toxicity. Fecal leukocyte, lactoferrin and occult blood are often present in patients with diarrhea due to bacterial infection (i.e., salmonella, shigella, Yersinia), which cause diffuse colonic inflammation. useful in febrile patients with significant acute diarrhea because if negative, the likelihood of getting a positive culture is very low. degree of dehydration is to subtract the patient's dehydrated weight from their weight prior to the illness. The assumption is that all of the weight loss is from total body water. The weight loss in grams is equivalent to the water loss in cc's |
|
|
diarrhea and electrolytes
|
Most episodes of dehydration caused by gastroenteritis are isonatremic, and serum electrolytes determination is often unnecessary.
Electrolyte levels measured in: (1) Children with moderate to severe dehydration; (2) Dehydrated children whose history and physical findings are inconsistent with a straightforward diarrheal episode; and (3) Children at risk for hyponatremia or hypernatremia. hypernatremic dehydration requires very slow replacement of fluids 1meq/2hr (10meq/24hr). occurs when water intake is reduced in the face of excessive water loss (from vomiting or diarrhea). ingestion of hypertonic fluids (boiled milk, home-made solutions to which salt is added, improperly mixed formula or significantly inadequate breast milk supply). Hyponatremic dehydration develops when there is ingestion of hypotonic fluids, such as fluids without salt (including free water) and improperly mixed formula. Infants with pyloric stenosis may also have significant electrolyte abnormalities associated with continuous vomiting. hypochloremic metabolic alkalosis, due to the loss of hydrochloric acid in the vomitus. sodium and potassium are nml |
|
|
most common cause of gastroenteritis at this age group?
|
Rotavirus
(Reoviridae) affects almost all children by age 5 most common in winter months in temperate climate. most severe disease and high proportion of severe episodes. dx rotavirus antigens in feces, done by two methods: enzyme immunoassay (EIA) 95-100% sens and spec or latex agglutination (LA). much faster, but is less sensitive and specific. fecal-oral route. Outbreaks in daycare centers incubation 48 hours selectively infects and destroys villus tip cells in the small intestine (duodenum) upper villus enterocytes are differentiated, which have both digestive and absorptive functions: (1) Digestive: hydrolysis of disaccharide; (2) Absorptive: transport of water and electrolytes via glucose and aminoacid co-transporters spared enterocytes secrete water and electrolytes creating an imbalance in the ratio of intestinal fluid absorbed to secreted. Malabsorption of complex carbohydrates (lactose) In 2006, the U.S. licensed RotaTeq, an oral, human-bovine reassortant rotavirus vaccine. three doses= efficacy against severe gastroenteritis 98%; against any severity, efficacy is 74%. at 2 months, 4 months, and 6 months side effects include a slightly increased incidence of mild, self-limited vomiting and diarrhea within 7 days after vaccination. Unlike the previous rotavirus vaccine (Rotashield), no increased incidence of intussusception |
|
|
Oral rehydration solution
|
commercially prepared solutions in cases of mild dehydration bc as effective as intravenous therapy and is much less costly.
also in moderate dehydration (10-15%) once vomiting stops x advantages over IV therapy: cheaper administered in home. evaluated glucose electrolyte solutions with Na 50-90 mmol/L successful in 90% of the patients and with fewer complications than IV therapy. available commercially: Na 45-50 mmol/L. These solutions (Naturalyte, Pediatric electrolyte, Pedialyte, Infalyte, Rehydralyte) best for maintenance. mild or moderate dehydration. Glucose-electrolyte solutions, formulated on physiologic principles vs popular, nonphysiologic liquids used to treat diarrhea that have low electrolyte content and that are hypertonic due to their high glucose content. ex: apple juice, colas and ginger ale. dehydrated should be fed as soon as they have been rehydrated |
|
|
Calculating Fluid Therapy for Children with Dehydration (4 steps)
|
1. Support cardiovascular circulation
diminished urine output or impaired cardiac output (tachycardia) IV fluid bolus of 20 mL/kg of normal saline (without dextrose) over 20 minutes to one hour repeated until the patient urinates and tachycardia improved. Caution w increased ICP, renal failure or cardiac failure. 2. Correct dehydration calculate and replace the patient's current fluid deficit. multiply weight in grams (grams and milliliters are interchangeable) by the estimated percent dehydration mild-moderate dehydration- replaced over next 24 hours: half replaced over the first 8 hours and second half over final 16 hours hypernatremia (Na >150) should have their deficit replaced evenly over 48 hours, not to drop the sodium faster than 1mEq/2hrs. deficit replaced with either IV or oral rehydration solutions. oral route, no more than 5 to 10 mL every 1-5 minutes. D5 1/4 normal saline. A solution of D5 1/2 normal saline may be used for patients >10kg. once voiding, 20 mEq/L of KCl should be added to the IV fluids. 3. Provide maintenance fluids Maintenance fluids fxn of metabolic rate and replace usual body losses infants <10kg, 100 mL/kg/d. either IV or oral rehydration solutions, or with full-strength formula or breast milk. addition to the bolus and deficit fluids 4. Replace any ongoing losses ongoing vomiting and/or diarrhea, insensible losses from fever or tachypnea. stool volume over 5g/kg/4hr should be replaced w 1/2 normal saline with 20mEq of KCL (no dextrose) |
|
|
Holliday-Segar formula:
|
0-10 kg: 100 mL/kg per day
10-20 kg: 1000 mL (+ 50 mL/kg for each >10 kg) per day >20 kg: 1500 mL (+ 20 mL/kg for each >20 kg) per day 100 mL/kg/day for the first 10 kg of body weight 50 mL/kg/day for the second 10 kg of body weight 20 mL/kg/day for each additional 1 kg of body weight |
|
|
refeeding after ORT
|
early refeeding showed that the duration of the diarrhea was reduced by 0.43 days b/c better nutrition
start 6hrs after rehydration started |

