![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
172 Cards in this Set
- Front
- Back
|
What is the gender difference of Hirschprung disease?
|
M:F = 4:1
|
|
|
Hirschprung disease:
__1__ of the colon proximally to an __2__ segment of the rectum |
1. Dilation
2. aganglionic |
|
|
Why does Hirschprung disease occur?
|
faulty migration of precursors of intestinal ganglionic cells
- develop from the neural crest and migrate into fetal intestine |
|
|
What is there a lack of in Hirschprung disease?
|
Auerbach and Meissner plexuses
|
|
|
How is Hirschprung disease diagnosed?
|
Rectal biopsy looking for absence of ganglion cells
|
|
|
How does Hirschprung disease present clinically?
|
- delayed passage of meconium
- chronic constipation in a young child |
|
|
What gene mutation is associated with Hirschsprung disease 50% of the time?
|
RET gene or RET ligand gene
|
|
|
What syndrome is Hirschsprung disease associated with?
|

Down syndrome
|
|
|
What other defects is Hirschsprung disease associated with?
|
VSD
Hydrocephalus Meckel diverticulum |
|
|
What can be a cause of acquired Hirschsprung disease?
|
Chagas' disease and destruction of ganglion cells by leishmania
|
|
|
What is Meckel Diverticulum a remnant of?
|
Vitelline duct (Omphalomesenteric)
|
|
|
Describe the Four 2's in Meckel Diverticulum
|
- 2% of the normal population
- 2 feet from ileocecal valve - 2 cm in length - 2% symptomatic - 2% of ectopic ulcers |
|
|
Decreased blood flow and ischemia of the bowel secondary to Atherosclerosis with thrombosis, thromboembolism, or reduced cardiac output from shock
|
Ischemic Bowel Disease
|
|
|
What group of people is Ischemic Bowel disease most common in?
|
Older individuals
|
|
|
What vessel supplies blood to the Small intestine?
|
Superior Mesenteric Artery
|
|
|
Twisting of a segment of the bowel on its vasculature mesentery, resulting in intestinal obstruction and infarction
|
Volvulus
|
|
|
Where does Volvulus most often occur?
|
Sigmoid colon but also in the Small Intestines
|
|
|
Telescoping of a proximal segment of the bowel into the distal segment
|
Intussusception
|
|
|
In adults what can cause Intussusception?
|
Tumors
|
|
|
Tortuous dilation of mucosal and submucosal blood vessels prone to rupture and bleeding
|
Angiodysplasia
|
|
|
What parts of the Colon are most susceptible to ischemia?
|
Splenic flexure
Rectosigmoid junction |
|
|
Where does Angiodysplasia most often occur?
|
Cecum and Right Colon
|
|
|
What age range is Angiodysplasia most common in?
|
> 50 yoa
|
|
|
What two diseases may Angiodysplasia be associated with?
|
Hereditary Hemorrhagic Telangiectasia (Osler-Weber-Rendu Syndrome) = spider veins
CREST syndrome |
|
|
What is the clinical presentation of Angiodysplasia?
|
Multiple episodes of Rectal bleeding
|
|
|
Varicose dilation of anal and rectal submucosal venous plexuses
|
Hemorrhoids
|
|
|
What are 3 risk factors for Hemorrhoids?
|
1. Constipation and prolonged straining during pooping
2. Pregnancy 3. Cirrhosis = Portal Hypertension |
|
|
Internal Hemorrhoid:
- Covered with what mucosa? - What veins? |
1. Rectal mucosa
2. Superior Hemorrhoidal veins |
|
|
External Hemorrhoid:
- Covered with what mucosa? - What veins? |
1. Anal squamous mucosa
2. Inferior hemorrhoidal veins |
|
|
How do Hemorrhoid patients present clinically?
|
streaks of bright red blood on hard stool
|
|
|
What are 5 complications of Hemorrhoids?
|
1. Bleeding
2. Thrombosis 3. Prolapse 4. Strangulation 5. Infection |
|
|
Diarrhea: increased passage of feces including:
-frequency? -Volume? -Consistency? |
> 3-4 / day
> 250 g / day Soft, fluid, watery |
|
|
Low volume, bloody, painful diarrhea
|
Dysentery
|
|
|
Describe the cause of Osmotic Diarrhea
|
Caused by nonabsorbable osmotic substances in the intestinal lumen
|
|
|
List some examples of things that cause Osmotic Diarrhea
|
1. Mannitol or Sorbitol in Sugar-free gum
2. Magnesium salts 3. Milk with Lactase deficiency |
|
|
Form of diarrhea where the intestinal cells secrete more water than they can absorb
|
Secretory diarrhea
|
|
|
List 4 causes of Secretory Diarrhea
|
1. Cholera toxin
2. E. coli toxin 3. Enteropathogenic viruses - Norwalk, Rota 4. Vasoactive Intestinal Peptide |
|
|
Describe Pancreatic cholera
|
Pancreatic VIPoma secreting massive amounts of VIP causing extensive SECRETORY Diarrhea
|
|
|
What are other names for Pancreatic cholera?
|
VIPoma
Verner-Morrison Syndrome WDHA = watery diarrhea and resultant dehydration, hypokalemia, achlorhydria |
|
|
Diarrhea that develops in the course of diseases that disrupt the intestinal layer or damage the mucosa
|
Exudative diarrhea
|
|
|
List some causes of Exudative diarrhea
|
1. Invasive bacteria
- Shigella and Salmonella 2. Amoebes 3. IBD |
|
|
Cause of viral diarrhea in infants 6-24 months
|
Rotavirus
|
|
|
Cause of viral diarrhea in epidemics, older children, or adults
|
Calicivirus = Norwalk virus
|
|
|
How does Cholera toxin work?
|
activates cAMP which causes Cl- secretion into intestinal lumen = water follows
|
|
|
Inadequate absorption of nutrients in the Small Intestine
|
Malabsorption syndromes
|
|
|
List the 3 modes of pathogenesis leading to Malabsorption syndromes
|
1. Defective intraluminal digestion
2. Mucosal dysfunction 3. Transport of nutrients across the mucosa and thru the lymphatics |
|
|
List 4 things that can cause malabsorption due to defective intraluminal digestion
|
1. Pancreatic insufficiency
2. excess gastric acid production (Zollinger-Ellison Syndrome) = inactivates Pancreatic enzymes 3. Biliary obstruction 4. Bacterial overgrowth = deconjugation of bile salt |
|
|
Excessive, large, sticky, stools that float = ?
|
Steatorrhea
|
|
|
Give some synonyms of Celiac disease (2)
|
1. Non-tropical sprue
2. Gluten-sensitive enteropathy |
|
|
Hypersensitivity to Gluten (and gliadin), resulting in loss of small bowel villi and malabsorption
|
Celiac sprue
|
|
|
What is the genetic predisposition to having Celiac Sprue?
|
HLA-DQ2 (95%)
|
|
|
In Celiac disease, what are people hypersensitive to?
|
Gluten (gliadin)
|
|
|
What pathological changes are seen in a small intestinal mucosal biopsy in Celiac disease?
|

-flattening of villi
-elongation of crypts -mucosal inflammation |
|
|
What parts of the SI are most common affected in Celiac disease?
|
Proximal > Distal intestine > stomach
|
|
|
What other disease is Celiac disease associated with?
|
IgA-mediated Dermatitis Herpetiformis
|
|
|
What gender does Celiac disease most commonly affect?
|
Female (josh's girlfriend or ceCELIA)
|
|
|
What antibodies are found in 90% of patients with Celiac disease?
|
Anti-Endomysial Ab's
|
|
|
How does a person with Celiac disease clinically present?
|
Usually in childhood with Malabsorption and Steatorrhea
|
|
|
Longterm-wise, what does Celiac Disease increase the incidence of?
|
T-cell Lymphoma of the Intestines and Stomach
|
|
|
What is Whipple disease caused by?
|
Intracellular bacteria = Tropheryma whippelii
|
|
|
What gender and age group does Whipple Disease usually affect?
|
White males 30-60 yoa
|
|
|
What is the diagnostic feature of Whipple Disease?
|
Biopsy
- SI Lamina Propria contains numerous Macrophages leading to widening of the villi - Macrophage stain with PAS or E.M. and contain bacteria (Tropheryma whippelii) |
|
|
How does a patient present clinically with Whipple disease?
|
Chronic diarrhea with abdominal pain, polyarthralgia, skin pigmentation, and anemia
|
|
|
Rare infectious disease involving many organs, including small intestines, joints, lung, heart, liver, spleen, and CNS
|
Whipple disease
|
|
|
Why does malabsorption occur in Whipple disease?
|
obstruction of the lymphatics in the intestinal villi due to macrophages
|
|
|
What are the 2 types of Inflammatory Bowel Disease?
|
1. Ulcerative colitis
2. Crohn's disease |
|
|
Systemic inflammatory disease of unknown etiology affecting predominantly the Colon and Terminal Ileum
|
Crohn Disease
|
|
|
What ethnicities/races are more often affected by Crohn's Disease?
|
Whites
Ashkenazi Jews |
|
|
What age range does Crohn's disease affect most?
|
15-30 years old
|
|
|
What is the distribution of Crohn's disease?
|
Mouth to Anus but "discontinuous/skips"
|
|
|
What is the intestinal wall like in Crohn's disease?
|
Thickened and rigid = due to chronic transmural inflammation
|
|
|
Describe the lumen in Crohn's disease
|
Stenosis = "string sign" on barium studies
|
|
|
Describe the mucosa in Crohn's disease
|
Deep linear ulceration with cobble-stone like pattern
|
|
|
Describe the inflammation in Crohn's disease
|
Transmural chronic inflammation which leads to thickening of the intestinal wall
- covered with fat tissue under the serosa |
|
|
List some complications of Crohn's disease
|
1. Fistulas
2. Obstructions 3. Adhesions |
|
|
Are granulomas seen in Ulcerative colitis or Crohn's?
|
Crohn's disease
|
|
|
How does a person with Crohn disease clinically present?
|
-recurrent episodes of diarrhea
-tenesmus, cramps, blood in stool - recurrences are common, last longer, with shorter and shorter asymptomatic intervals |
|
|
Chronic systemic inflammatory disease of unknown etiology, predimonantly limited to the mucosa of the colon
|
Ulcerative colitis
|
|
|
What is the distribution and location of Ulcerative Colitis?
|
Ulceration begins in rectum and spreads proximally to involve the entire colon
- no skipped areas = continuous |
|
|
Describe the inflammation in Ulcerative Colitis
|
limited only to the mucosa
|
|
|
Describe the gross appearance of Ulcerative Colitis
|
- extensive ulceration
- pseudopolyps |
|
|
Remnants of normal or regenerating colonic mucosa surrounded by ulcerations = ?
What are they associated with? |
Pseudopolyps in Ulcerative colitis
Ulcerative Colitis |
|
|
Accumulation of neutrophils inside colonic crypts = ?
What are they associated with? |
Crypt abscesses in Ulcerative colitis
Ulcerative Colitis |
|
|
What is Toxic Megacolon?
|
Complication of Ulcerative Colitis
- massive dilation of the entire large intestine |
|
|
List 5 Extraintestinal complications of IBD (Crohn's / UC)
|
1. Migratory polyarthritis
2. Iridiocyclitis = inflammation of eye and iris 3. Pyoderma gangrenosum = pus coming out of skin 4. Erythema nodosum = red nodules on skin 5. Primary sclerosing cholangitis = fibrosis around the common bile duct leading to jaundice |
|
|
IBD that has a greater risk of developing cancer
|
Ulcerative colitis
|
|
|
Outpouching of mucosa and/or muscularis through a defect in the intestinal wall
|
Diverticulosis
|
|
|
What are the 2 types of Diverticulosis and where are they most often located?
|
1. Congenital = Small intestine
2. Acquired = Sigmoid colon |
|
|
What parts of the world is Diverticulosis more common and why?
|
Developed nations due to constipation related to low-fiber diets
|
|
|
What is the etiology of Diverticulosis? (2)
|
1. straining during defecation
2. defect in the muscle layer |
|
|
What are 3 complications of Diverticulosis?
|
1. Diverticulitis
2. Pericolitis = inflammation around the colon 3. Rupture |
|
|
How does Diverticulitis clinically present?
|
1. "Left-sided appendicitis" = Left lower quadrant pain
2. Fever 3. Leukocytosis |
|
|
What is the cause of Diverticulitis?
|
Stool impacted in the diverticulum sac
- bacteria = inflammation - ischemia and ulceration |
|
|
When a segment of the bowel becomes imprisoned within a hernia which can lead to intestinal obstruction and infarction
|
Incarcerated hernia
|
|
|
Fibrous tissue between 2 loops of bowel = ?
|
Adhesion
|
|
|
Lack of interstinal peristalsis associated with stagnation of intestinal contents = ?
|
Paralytic Ileus
|
|
|
What is the most common cause of Ileus?
|
Abdominal surgery
|
|
|
What would be a myopathic disease causing Ileus? Neuropathic?
|
Myopathic = Myasthenia
Neuropathic = Hirschsprung |
|
|
Most common intestinal polyp
- small, dew-like, glistening nodules |
Hyperplastic polyps
|
|
|
Where are Hyperplastic polyps most often found?
|
Rectum or Sigmoid colon
|
|
|
What are Juvenile polyps?
|
-Acquired hamartomas typically found in the rectum of children <10 yoa
-Pedunculated, round, with smooth surface -Composed of mucus-filled cystic glands and edematous, inflamed stroma |
|
|
What is the inheritance pattern of Peutz-Jeghers polyps?
|
Autosomal dominance
|
|
|
In Peutz-Jeghers Syndrome, what is also present besides the polyps?
|

Pigmented macules on the lips and perioral skin
|
|
|
Ulcerative colitis or Crohn's disease: inflammatory pseudopolyps?
|
Ulcerative colitis
|
|
|
List the 3 categories of Neoplastic Polyps
|
1. Tubular adenoma
2. Villous adenoma 3. Tubulovilous adenoma |
|
|
Most common neoplastic polyp
|
Tubular adenoma (>90%)
|
|
|
What is the distribution of Tubular Adenomas?
|
equally distributed throughout the entire large intestine
|
|
|
What are Tubular Adenomas composed of?
|
Tubular glands lined by dysplastic columnar epithelium
|
|
|
What % of Tubular Adenomas give rise to Adenocarcinoma?
|
2-3%
|
|
|
What is the risk of cancer in Tubular Adenomas proportional to?
|
Increasing size and number of polyps
|
|
|
Which neoplastic polyp has a greater tendency to transform to malignancy?
|
Villous (40% vs. 2-3%)
|
|
|
What is the appearance of Villous Adenomas?
|
Sessile (broad-based)
Larger than Tubular adenomas Finger-like protrusions lined with Columnar epithelium |
|
|
What do Villous adenomas secrete?
|
Mucin
|
|
|
What is the normal size of Tubular adenomas?
What is the size of Villous Adenomas? |
< 1 cm
~4 cm |
|
|
What are Tubulovillous adenomas?
|
Tubular adenomas that contain villous parts
-represent an intermediate step between tubular and villous adenomas |
|
|
What is the inheritance type of Familial Adenomatous Polyposis Coli?
|
Autosomal dominant
|
|
|
What is the cause of Adenomatous Polyposis Coli?
|
linked to the deletion of the tumor suppressor gene APC
|
|
|
What chromosome is the APC gene on?
|
5q21
|
|
|
T or F: all patients with Familial Polyposis develop tubular adenomas and cancer
|
True
|
|
|
With FAP, at what age is cancer found in 100% of patients?
|
by 40 yoa
|
|
|
What is performed in mid-life with people with Familial Adenomatou Polyposis Coli?
|
Prophylactic Colectomy
|
|
|
List the genes involved in the pathway from adenomatous polyps to cancer
|
1. loss of APC tumor suppressor
2. mutation of k-ras oncogene 3. loss of tumor suppressor gene p53 |
|
|
What mutation that leads to cancer does not involve adenoma precursor lesions?
|
DNA mismatch repair genes (MSH2)
|
|
|
What is the most common GI malignancy
|
Carcinoma of the large intestine
|
|
|
Variant of FAP with multiple osteomas, fibromatosis, and epidermal inclusion cysts
|
Gardner syndrome
|
|
|
Variant of FAP characterized by numerous colonic adenomatous polyps and CNS tumors (Gliomas)
|
Turcot Syndrome
|
|
|
What are the precursor lesions of Carcinoma of the Large Intestine?
|
Adenomas
|
|
|
How does a person with Right-sided Colon Cancer present?
|
Bleeding
1. occult blood in stool 2. Iron deficiency anemia |
|
|
How does a person with Left-sided Colon Cancer present?
|
Obstruction
1. constipation or diarrhea 2. reduced caliber stools |
|
|
What is the appearance of Left-sided Colon cancer?
|
Circumferential growth producing a "napkin-ring" configuration
|
|
|
What is the appearance of Right-sided Colon Cancer?
|
Exophytic or flat, broad-based lesion = Polypoid mass
|
|
|
List the parts of the Large Intestine where most carcinomas develop
|
1. Left-side = 55%
2. Right-side = 35% 3. Transverse = 10% |
|
|
In a barium enema studies, what are Left-sided tumors described as looking like?
|

"apple-core" like lesions
|
|
|
How do Colorectal Cancer metastasize?
1. Lymphatic spread? 2. Hematogenous spread? |
1. Mesenteric lymph nodes
2. Portal vein to liver |
|
|
What are 3 risk factors associated with Colon Cancer?
|
1. high calorie intake
2. low-fiber food associated with constipation 3. high fat contect and refined sugars |
|
|
-Glycoprotein secreted by fetal intestinal cells into the meconium
-Also secreted by Adenocarcinoma cells in the blood of patients with Colorectal Cancer |
Carcinoembryonic Antigen (CEA)
|
|
|
Why is CEA not used for screening of persons at risk of developing Colon Cancer?
|
CEA test lacks specificity
|
|
|
What conditions are associated with elevated blood CEA? (5)
|
1. Colon Adenocarcinoma
2. Adenocarcinoma of Pancreas, Gallbladder, Lung 3. Ulcerative colitis and Crohn's Disease 4. Alcohol Cirrhosis 5. Smoking |
|
|
Define Carcinoid tumors
|
Low-grade malignant tumors composed of Neuroendocrine cells often producing Serotonin
|
|
|
At what size do Carcinoid tumors metastasize?
|
> 2 cm
|
|
|
What are the most common locations of Carcinoid tumors of the GI?
|
1. Appendix = 40%
2. Rectum 3. Terminal Ileum 4. Stomach |
|
|
How do you recognize Carcinoid tumors under EM?
|
Neuroendocrine granules
|
|
|
What 3 things can you stain with in Immunohistochemistry to identify Carcinoid tumors?
|
1. Neuropeptide hormones
2. Chromogranin 3. Synaptophysin |
|
|
In Carcinoid tumors, which site rarely metastisizes?
|
Appendix Carcinoid tumors
|
|
|
What has to happen to produce Carcinoid Syndrome?
|
Metastasis to the Liver from the GI
|
|
|
What are the clinical features of Carcinoid Syndrome?
|
1. Facial flushing
2. Bronchospasm = wheezing 3. Cardiac fibrosis of Tricuspid and Pulmonic valve 4. Diarrhea |
|
|
In Cardinoid tumors, what may be elevated in the urine?
|
5-hydroxylindolacetic acid (5-HIAA)
|
|
|
What are the most common sites of GI Lymphoma>
|
1. Stomach = 55%
2. SI = 25% 3. LI = 20% |
|
|
What type of GI Lymphoma are 90% of the cases?
|
MALToma
|
|
|
What are the risk factors for GI Lymphoma?
|
1. H. pylori
2. Celiac disease 3. Familial Mediterranean Fever |
|
|
What are MALTomas?
|
Primary GI tumor that are low-grade malignant B-cell lymphomas originating from the Mucosa-associated Lymphoid Tissue
|
|
|
What are Gastrointestinal Stromal Tumors (GIST) sensitive to?
|
Gleevec
|
|
|
Sarcoma of smooth muscle = ?
|
Leiomyosarcoma
|
|
|
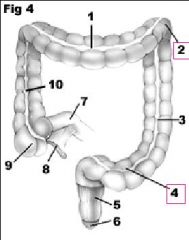
Meckel Diverticulum
|

What is this?
|
|
|
Massive infarction leading to hemorrhaging
Obstruction of the Mesenteric Arter |
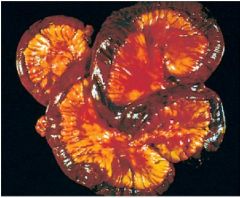
What happened here?
What was the cause? |
|
|
Pseudomembranous colitis
C. difficile |
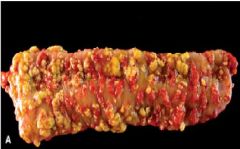
What is this?
What causes it? |
|
|
Pseudomembrane in Pseudomembrane colitis
|
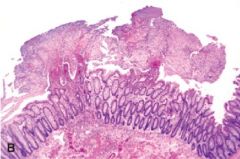
What is this showing?
|
|
|
Malabsorption Syndrome, given is the clinical finding...you tell the deficiency:
1. Growth retardation, muscle wasting, edema 2. Microcytic-hypochromic anemia 3. Macrocytic, megaloblastic anemia 4. Night blindness, Keratomalacia 5. Osteomalacia 6. Bleeding tendency 7. Tetany, paresthesia, secondary hyperparathyroidism |
1. Protein
2. Iron 3. Folate / B12 4. Vitamin A 5. Vitamin D 6. Vitamin K 7. Calcium |
|
|
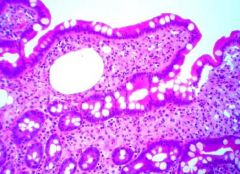
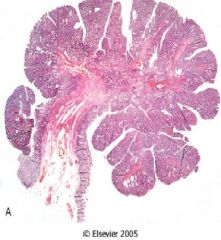
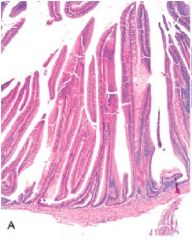
Celiac disease causes atrophy of the villi leading to malabsorption
|
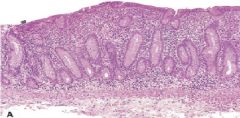
This is the Small Intestine...what is the pathology?
|
|
|
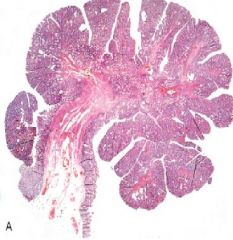
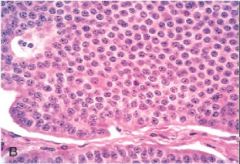
Crohn's b/c there is a Granuloma present
|
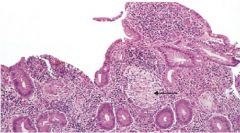
Is this Crohn's or Ulcerative Colitis? How do you know?
|
|
|
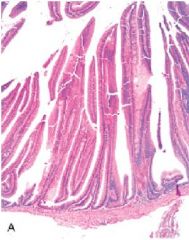
Ulcerative Colitis
- pseudopolyps are present |
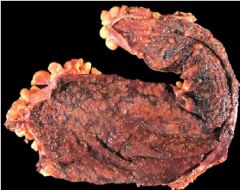
What is this?
|
|
|
Crohn's
Ulcerative colitis |
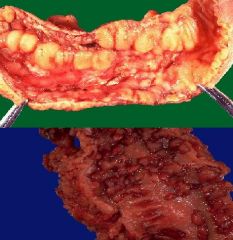
Top = ?
Bottom = ? |
|
|
Summary of Crohn's and Ulcerative Colitis
|
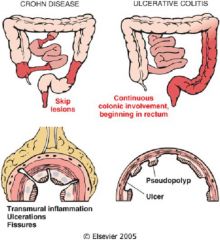
-
|
|
|
Toxic Megacolon
Ulcerative colitis |

What is this called?
What caused it? |
|
|
Diverticulosis
Sigmoid colon Age Low-fiber diet |

What is this?
Most common site? Related risk factor? Presumed cause? |
|
|
Diverticulosis
|

What is this?
|
|
|
Autosomal dominant disease with multiple Hamartomatous polyps in the Small Intestine + melanin pigmentation on the Oral Mucosa
|
Peutz-Jeghers Syndrome
|
|
|
Tubular adenoma
Benign but transforms 2-3% of the time |
What is this showing?
Benign or Malignant? |
|
|
Villous Adenoma
|
What is this?
|
|
|
Familial Adenomatous Polyposis Coli
|

What is this?
|
|
|
Colorectal Adenocarcinoma
|

What is this?
|
|
|
Carcinoid tumor
|
What is this?
|

