![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
251 Cards in this Set
- Front
- Back
|
What is the precursor of Skeletal Muscle?
|
- Paraxial Mesoderm --> somites (body wall and limbs)
- Head Mesoderm (head and neck) |
|
|
What is the precursor of Cardiac Muscle?
|
Splanchnic Mesoderm
|
|
|
What is the precursor of Smooth Muscle?
|
- Visceral smooth - Splanchnic Mesoderm
- Vascular smooth - Local Mesenchyme (including ectoderm-derived neural crest mesenchyme) |
|
|
What muscles develop from ectoderm?
|
Smooth muscle of constrictor and dilator pupillae as well as myoepithelial cells of mammary and sweat glands
|
|
|
what do the skeletal muscles of the body wall and limbs form from?
|
Paraxial mesoderm --> Somites (40+ pairs)
|
|
|
What transcription factors and signaling molecules help mediate the migration of muscle-forming mesenchyme?
|
- Transcription factors: myogenic regulatory factors - MyoD, Myf5, Myf4, myogenin, Mef2
- Signaling molecules: Fgf, Wnt, Tgfβ |
|
|
What develops from the somite?
|
Precursor cells for skeletal muscle, bone, cartilage, and connective tissue --> skeletal muscle of trunks and limbs
|
|
|
How does the location in the somite affect what signals impact it?
|
- Dorsolateral / dorsal part - influenced by Wnts originating from neural tube and surface ectoderm
- Ventraomedial - form scleratome (cartilage and bone precursors --> vertebral column / ribs / sternum) |
|
|
What happens to the cells on the dorsolateral part of the somite?
|
- Under influence of Wnts from neural tube and surface ectoderm
- Maintain epithelial characteristics - Become known as Dermomyotome (DM) |
|
|
What happens to the cells in the Dermomyotome (DM) - previously the dorsolateral part of somite?
|
- Exposed to gradient of Bmp4 from lateral mesoderm (LM)
- Modulated across DM by noggin (Bmp inhibitor) from dorsal and ventral neural tube - Other DM cells influenced by Wnt and Shh from neural tube and notochord - Dorsomedial and dorsolateral edges undergo epithelial to mesenchyme transformation (EMT) - Relocate beneath epithelial portion of DM (become myogenic cells) |
|
|
What happens to the cells on the dorsomedial and dorsolateral edges/lips of the Dermomyotome (DM)?
|
- Undergo Epithelial to Mesenchyme Transformation (EMT)
- Relocate under epithelial portion of DM - Become myogenic cells that form a layer called the "Myotome" |
|
|
What are the precursor cells for skeletal muscle of trunk and limbs?
|
Myogenic cells in layer called the Myotome (previously in Dermomytome and before that the Somite)
|
|
|
What happens to the cells on the central portion of the Dermomyotome (DM)?
|
- Remain epithelial - eventually form two populations of precursor cells
- One becomes an additional population of myogenic cells (undergo EMT and migrate/displaced under the myotome) - many become satellite cells - Others undergo EMT and contribute to formation of dermis of skin on back (Dermatome) |
|
|
Cells that form the Dermatome originate as what?
|
Population of cells located in central portion of dermomyotome (DM) that remain epithelial --> undergo EMT --> contribute to dermis of skin on back
|
|
|
Where is the Lateral Somite Frontier (LSF)?
|
- Boundary between the lateral edge of the somite and medial edge of the lateral mesoderm (LM)
- Interface set up by interaction of different signaling molecules originating from somites, LM, and surrounding tissues |
|
|
What is the significance of the Lateral Somite Frontier (LSF) - the boundary between the lateral edge of the somite and the medial edge of the lateral mesoderm (LM)?
|
Defines two environments or domains within which Dermomyotome-derived cells develop into skeletal muscle
|
|
|
What happens to the cells originating from the dorsomedial portion of the Dermomyotome?
|
- Remain adjacent to neural tube and notochord
- Influenced by Wnt and Shh - Express Myogenic Regulatory Factors Myf5 and MyoD and form intrinsic muscles of back, prevertebral and intercostal muscles = Primaxial Domain - Attach to bones from scleratome cells of somite |
|
|
What is the origin of the intrinsic muscles of the back, prevertebral muscles, and intercostal muscles = Primaxial Domain?
|
Dorsomedial portion of Dermomyotome (DM) (influenced by Wnt and Shh)
|
|
|
What happens to the cells originating from the ventrolateral portion of the Dermomyotome?
|
- Migrate across Lateral Somite Frontier (LSF) into somatic mesoderm
- Influenced by Wnt and Bmp4 - Express myogenic regulatory factor MyoD - Become muscles of abdominal wall, limbs, and infrahyoid muscles = Abaxial Domain |
|
|
What is the origin of themuscles of abdominal wall, limbs, and infrahyoid muscles = Abaxial Domain?
|
Ventrolateral portion of Dermomyotome (DM) (influenced by Wnt and Bmp4)
|
|
|
Once cells become part of the myotome portion of the Dermomyotome (DM), what happens to their potential?
|
Restricted to skeletal muscle lineage = now called myogenic cells or pre-myoblasts
|
|
|
What do the Myogenic cells / Pre-myoblasts do?
|
- Proliferate
- Migrate - Upregulate certain myogenic regulatory factors (Myf5 and MyoD) - Become post-mitotic, committed myoblasts (removed from cell cycle) |
|
|
What happens to the Myogenic cells / Pre-myoblasts once they have been removed from the cell cycle?
|
- Synthesize actin and myosin
- Secrete adhesive glycoprotein once they are at definitive location - Align into chains of myoblasts - Fuse to become Multinucleated Myotubes (requires M-cadherin) |
|
|
What happens to Myoblasts, once they are in their definitive location in the embryo?
|
- Align into chains of myoblasts
- Fuse to become Multinucleated Myotubes - Fusion requires adhesion molecule M-cadherin |
|
|
What is happening in the Multinucleated Myotubes (fused myoblasts)?
|
- Troponin and Topomyosin mediate myofiber and sarcomere formation
- Results in differentiated muscle cells or muscle fibers = Primary Muscle Fibers |
|
|
When do Primary Muscle Fibers form?
|
- First muscle fibers to form
- Form after the first myotubes form troponin and topomyosin, which mediate myofiber and sarcomere formation - Become SLOW muscle fibers |
|
|
When do Secondary Muscle Fibers form?
|
- Form later around the primary fibers at a time when branches of spinal nerves approach and innervate forming muscle masses
- Become FAST muscle fibers |
|
|
What forms the Fast muscle fibers? Slow muscle fibers?
|
- Fast = Secondary muscle fibers
- Slow = Primary muscle fibers |
|
|
When is skeletal muscle fiber formation completed?
|
By birth - postnatal growth of skeletal muscle is accomplished by myogenic stem cells (Satellite cells)
|
|
|
Where are Satellite cells? What is their function?
|
- Lie between the muscle fibers and its basement membrane
- Necessary for postnatal growth of skeletal muscle |
|
|
What is necessary for formation of Satellite Cells?
|
Form from myogenic cells of central Dermomyotome (DM) - mediated by expression of Pax3 and Pax7
|
|
|
What are some proposed strategies for the formation of individual named skeletal muscles?
|
- Change in fiber direction
- Fusion of adjacent myotomes - Longitudinal splitting - Tangential splitting into layers - Atrophy (partial or complete) - Migration |
|
|
What is an example of "change in fiber direction" for forming individual skeletal muscles?
|
Abdominal wall and intercostal muscles (also dependent on tangential splitting into layers)
|
|
|
What is the basis for innervation of skeletal muscles by multiple spinal cord levels?
|
Fusion of adjacent myotome levels (most muscles)
|
|
|
What is an example of "longitudinal splitting into parts" for forming individual skeletal muscles?
|
Strap (infrahyoid) and trapezius / sternocleidomastoid muscles
|
|
|
What is an example of "tangential splitting into layers" for forming individual skeletal muscles?
|
Abdominal wall and intercostal muscles (also dependent on change in fiber direction)
|
|
|
What is an example of "atrophy" for forming individual skeletal muscles?
|
Fronto-occipitalis muscle
|
|
|
What is an example of "migration" for forming individual skeletal muscles?
|
Superficial back and serratus muscles
|
|
|
What are muscles in the head and neck derived from? Innervation?
|
- Derived from head mesoderm and occipital myotomes
- Innervated by cranial nerves |
|
|
What are muscles in the trunk derived from? Innervation?
|
- Derived from ventrolateral and ventromedial edges of myotome
- Innervated by spinal nerves |
|
|
With respect to innervation, how is a myotome subdivied?
|
- Dorsal = epaxial --> receive motor innervation from dorsal primary rami of spinal nerves
- Ventral = hypaxial --> receive motor innervation from ventral primary rami of spinal nerves |
|
|
What do the terms "primaxial" and "abaxial" refer to?
|
Embryonic domain in which the skeletal muscle developed
- All abaxial domain muscles would be innervated by ventral primary rami / hypaxial - Some primaxial domain muscles are innervated by dorsal primary rami / epaxial and others by ventral primary rami / hypaxial |
|
|
What do the terms "epaxial" and "hypaxial" refer to?
|
Innervation
- Epaxial = dorsal primary rami - Hypaxial = ventral primary rami |
|
|
What are some of the malformations that can occur in the muscular system?
|
- Absence of skeletal muscle(s) - e.g., Poland Sequence and Prune Belly Syndrome
- Variation in size/shape and attachment of muscles - Congenital Muscular Torticollis (wryneck) - Muscular Dystrophy - e.g., Duchenne Type and Becker's Type |
|
|
What are some common muscles that can be absent?
|
- Palmaris longis
- Serratus anterior - Quadratus femoris - Others |
|
|
When skeletal muscles are absent, what are the consequences?
|
- Usually unilateral
- Often asymptomatic |
|
|
What are the common symptoms of Poland Sequence?
|

- Absence of Pectoralis Major (usually sternocostal head) and also Pectoralis Minor muscles
- Nipple displaced laterally or may be missing - Breast tissue is either hypoplastic or missing - Deficiency of subcutaneous fat and axillary hair - Rib cage may be hypoplastic - Upper limb anomalies also associated (including shortened limb segments and hand defects like syndactyly and brachydactyly) |
|
|
On what side does Poland Sequence occur? Who is most affected by it? How frequent?
|

- Twice as common on right side (missing pec major/minor)
- More common in males - 1/20,000-1/50,000 births |
|
|
What is the cause of Poland Sequence?
|

Unknown but may result from interference w/ formation of subclavian artery
|
|
|
What are the symptoms of Prune Belly Syndrome?
|
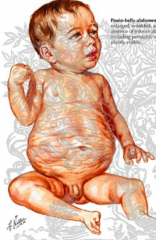
- Absence of abdominal muscles
- Undescended testes - Bladder and urinary tract anomalies |
|
|
What is the cause of Prune Belly Syndrome?
|
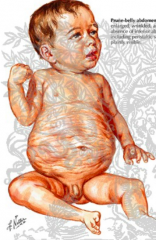
- Prenatal accumulation of fluid in lower abdomen d/t urinary system anomalies may interfere w/ development or cause degeneration of abdominal muscles
- After birth, the abdominal distention is reduced causing skin over area to be very wrinkled |
|
|
Who is most affected by Prune Belly Syndrome? How common is it?
|
- Almost exclusively affects males
- 1/40,000 births |
|
|
How can skeletal muscle vary in size/shape/attachment? Impact?
|
- Muscle may have an extra belly or additional tendons at its attachment to bone
- Usually these variations are functionally and clinically insignificant |
|
|
What are the symptoms of Congenital Muscular Torticollis (Wryneck)?
|
- Fixed rotation and tilting of the head to one side
- More common on right side - Also have congenital hip dysplasia - Sometimes associated w/ acquired plagiocephaly (asymmetrically distorted skull) |
|
|
What is the cause of Congenital Muscular Torticollis (wryneck)?
|
- Can occur in absence of trauma
- Suggests primary defect with SCM or insufficient space for fetus in uterus - Can also be acquired (secondary to infections or trauma to SCM muscle) |
|
|
What are the symptoms of Muscular Dystrophy?
|
- Progressive weakness and deterioration of skeletal muscle
- Without CNS or PNS pathology - Onset in infancy to lat adult |
|
|
What is the most common type of Muscular Dystrophy? How is it inherited? Who does it affect?
|
- Duchenne Type
- X-linked recessive - Affects boys in early childhood (1/3500 births) |
|
|
What is the cause of Ducehenne Muscular Dystrophy?
|
- Skeletal myocytes lack dystrophin (membrane associated actin binding glycoprotein)
- These myofibers are more susceptible to damage when physically stressed (replaced by fibrous tissue) |
|
|
What is the milder form of Muscular Dystrophy? How is it different from Duchenne Type?
|
- Becker's Type
- Later onset and milder condition |
|
|
What are the primary tissues that provide a supporting framework for cells, organs, and structures in the body?
|
- Cartilage
- Bone - Fibrous connective tissue (all considered connective tissue b/c they are composed of cells suspended in ECM containing collagen, proteoglycans, etc) |
|
|
What kind of tissues are referred to as skeletal tissues?
|
Bone and cartilage
|
|
|
What are the characteristics of embryonic CT?
|
- Mesenchymal
- Arranged in ECM as scattered, individual cells or condensed into aggregates - High ratio of CELLS : ECM - Fibrous proteins in hydrated, amorphous ground substance (proteoglycans and hyaluronic acid) |
|
|
What are the characteristics of mature CT?
|
- Cells: sparse to abundant
- Lower Cells : ECM ratio - Loose and dense fibrous CT, bone, cartilage, blood, lymph |
|
|
What is the function of Dense Fibrous (mature) CT?
|
Supporting tissue that forms organ capsules, tendons, fascia
|
|
|
What is the organization/function of cartilage (mature CT)?
|
Fibers and cells are embedded highly hydrated, amorphous ECM; avascular; provides flexible support
|
|
|
What is the organization/function of bone (mature CT)?
|
Fibers and cells are embedded within a mineralized ECM; richly vascular; provides rigid support
|
|
|
What do bone and cartilage develop from?
|
Skeletal Tissue Forming Mesenchyme (STFM)
|
|
|
What does the Skeletal Tissue Forming Mesenchyme (STFM) that develops into bone and cartilage originate from?
|
- Trunk: Scleratome tissue of somites (paraxial mesoderm) and Somatic Mesoderm (lateral mesoderm)
- Head: Neural crest (ectomesenchyme) and Head Mesoderm (unsegmented paraxial mesoderm) |
|
|
What are the general characteristics of the Skeletal Tissue Forming Mesenchyme (STFM)?
|
- Often migrates or is displaced from site of origin
- Often condenses into Pre-Skeletal Condensations - Differentiation influenced by Specific Transcription Factors and Signals from adjacent epithelium |
|
|
At the site of bone and cartilage formation, what does the Skeletal Tissue Forming Mesenchyme (STFM) form? How?
|
- Preskeletal Condensation of epithelial-like cells
- Express N-cadherin that promotes mesenchyme-to-epithelial MTE transformation - Condensation forms as a result of inductive signaling from surrounding tissues - Maintained by expression of cell adhesion molecules (N-CAM) |
|
|
What transcription factors stimulate Skeletal Tissue Forming Mesenchyme (STFM) to become cartilage?
|
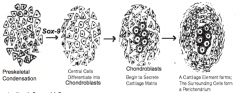
Sox-9 --> Chondroblasts
|
|
|
How does Sox-9 expression from STFM cells affect the STFM cells?
|
- Differentiate into chondroblasts
- Secrete Type II collagen, aggrecan, and other components of cartilage matrix |
|
|
What are the three types of cartilage?
|
- Hyaline
- Elastic - Fibrocartilage |
|
|
What forms around developing hyaline and elastic cartilage elements?
|
Fibrous capsule-like Perichondrium
|
|
|
What transcription factors stimulate Skeletal Tissue Forming Mesenchyme (STFM) to become bone?
|
BMP --> causes them to express Runx-2 (Cbfa-1) --> transform into Osteoblasts
|
|
|
What is the process of Intramembranous Ossification?
|
Formation of some bones directly from a preskeletal condensation that resembles a membrane of mesenchymal cells
|
|
|
How does Runx-2 expression from STFM cells affect the STFM cells?
|

- Transforms them into Osteoblasts
- Secrete needle-like spicules of bone tissue containing Type I collagen and bone specific proteins (e.g., osteocalcin and osteopontin) |
|
|
Where do needle-like spicules radiate from?
|
Primary ossification center w/in forming bone
|
|
|
What kind of bones form via Intramembranous Ossification?
|
Usually superficial bones (e.g., flat skull bones)
|
|
|
How do flat bones grow?
|
Addition of new bone on outer surface (by osteoblasts) accompanied by removal of bone on inner surface (by osteoclasts)
|
|
|
What is the process of Endochondral Ossification?
|
- Cells in STFM condensation form a cartilage model of bone
- Indian Hedgehog (Ihh) and Runx-2 cause chondrocytes to undergo hypertrophy and secrete Type X collagen and bone specific proteins - Collar of bone forms in area to become Diaphysis - Hypertrophied chondrocytes secrete Vegf to stimulate BV ingrowth accompanied by invasion of osteoblasts - Osteoblasts form bone tissue to replace calcified areas of cartilage |
|
|
Where does Endochondral Ossification occur?
|
- Begins in middle of cartilage model (particularly in long bones of limb)
- Ends of bone (epiphysis) ossify at a later time in same manner as diaphysis |
|
|
What is the function of Endochondral Ossification?
|
- Allows bones to grow in length due to presence of cartilage growth plate (epiphyseal plate) at one or both ends of forming bone
- Epiphyseal plate is continually producing new cartilage and is subsequently replaced by bone tissue |
|
|
What happens if a person is a homozygous Runx-2 null mutant?
|
- They don't form bones
- Skull made of fibrous CT - Partially calcified cartilaginous skeleton - Smaller with shorter limbs - Die shortly after birth because the chest collapses and can't sustain respiration (d/t no bones) |
|
|
What important signaling factors are involved in transforming STFM to Cartilage?
|
Sox-9 only
|
|
|
What important signaling factors are involved in transforming STFM to Bone via Endochondral Ossification?
|
- Sox-9 --> Cartilage model
- Ihh; Vegf --> Bone replaces model - Runx-2 --> Endochondral ossification |
|
|
What important signaling factors are involved in transforming STFM to Bone via Intramembranous Ossification?
|
Runx-2 only
|
|
|
What are Ossification Centers?
|
Areas of bone premordia in which the ossification process begins
|
|
|
What is knowledge about ossification centers clinically important for?
|
- Determining bone age (the amount of epiphyseal cartilage retained within skeleton)
- Used as an index of skeletal growth and maturation compared to chronological age |
|
|
What does "Bone Age" mean?
|
Amount of epiphyseal cartilage retained in skeleton
|
|
|
What is a Primary Ossification Center? How many are there per bone? When do they appear?
|
- Initial ossification center to form in developing bone
- Some have only one, but many have multiple primary ossification centers - First center appears at 7 weeks |
|
|
Where is a Primary Ossification Center in long bones? in flat bones?
|
- Long bones - usually in shaft region (metaphysis) of bone
- Flat bones - usually at center of bone primordia |
|
|
What hormones influence bone growth and maturation once ossificationb egins?
|
- Estrogen
- Thyroid hormones - Growth hormone |
|
|
What is a Secondary Ossification Center? How many are there per bone? When do they appear?
|
- Additional centers of bone formation appearing in the prenatal, postnatal, or post-pubertal period
- Disappear during or after puberty and as late as early second or third decade of life |
|
|
Where do Secondary Ossification Centers appear?
|
- Ends of long bones
- Heads of ribs - Surface of vertebrae - Etc. |
|
|
Where is the epiphyseal plate located relative to the primary and secondary ossification centers? How do these centers affect the epiphyseal plate?
|
It is in between them (in long bones) - closure of secondary center results in disappearance of epiphyseal plate
|
|
|
What are some disorders impacting skeletal development?
|
Defects in bone or cartilage formation:
- Chondrodystrophias - Marfan Syndrome - Mucopolysaccharidoses Disorders - Osteogenesis Imperfecta Endocrine disorders impacting skeletal development: - Hyperpituitarism - Hypothyroidism |
|
|
What is the usual defect in bone or cartilage formation?
|
Abnormal ECM production
|
|
|
What are Chondrodystrophias?
|
Disorders characterized by disproportionate growth
|
|
|
What is the most common Chondrodystrophia? What is the cause? How common is it?
|
- Achondroplasia / short stature - dwarfism
- Autosomal dominant inheritance, although 80% appear spontaneously (mutation in Fibroblast Growth Factor Receptor 3 - FGFR-3 which interferes w/ cartilage formation) - 1/1000 live births |
|
|
What is the most common cause of short stature (dwarfism)?
|
Achondroplasia
|
|
|
What happens in a person with Achondroplasia?
|
- Interference w/ epiphyseal plate development results in disproportionally shortened limbs (mainly proximal segment)
- Normal sized trunk - Base of skull is shortened making midface appear small and immature - Short fingers and accentuated lordosis - Normal intelligence |
|
|
What are the symptoms of Marfan Syndrome?
|
- Spider-like, elongated digits
- Aortic aneurysms - Eye and spine abnormalities - Joint hypermobility |
|
|
How is Marfan Syndrome inherited? What is the mutation? How common?
|
- Autosomal dominant (although 15-25% spontaneous mutation)
- Defect of production of fibrillin (component of ECM) - 1-5/10,000 births |
|
|
What are Mucopolysaccharidoses? Symptoms?
|
- Family of metabolic diseases that affect bone formation
- Results in dwarfism and bone irregularities - Chronic, progressive distortions of face and skull - Thickened, hairy skin - Organ enlargement - Often altered mental status |
|
|
What is the cause of Mucopolysaccharidoses? How common?
|
- Autosomal recessive inheritance
- Absence or defects in an enzyme --> accumulation of glycosaminoglycans in tissues and cells - 1-2 / 100,000 births |
|
|
What is Osteogenesis Imperfecta characterized by?
|
- Brittle bones
- Causes multiple fractures - Eyes have blue sclera - Affects ears, joints, spine, and teeth - Symptoms range from severe to mild |
|
|
What is the cause of Osteogenesis Imperfecta? How common?
|
- Dominant inheritance or spontaneous mutation
- Defect in expression of Type I collagen gene - 1/10,000 - 1/20,000 live births |
|
|
What are the symptoms of Hyperpituitarism?
|
- Prior to epiphyseal plate closure: gigantism (very rare)
- After epiphyseal plate closure: Acromegaly - enlargement of face, hands, and feet |
|
|
What is the cause of Hyperpituitarism / gigantism / acromegaly?
|
Overproduction of growth hormone d/t tumor of pituitary gland tissue
|
|
|
What are the symptoms of Hypothyroidism?
|
- Pituitary dwarf (cretinism)
- Mental retardation - Skeletal and ear anomalies - Bone age is younger (more epiphyseal tissue) than it should be for their chronological age |
|
|
How many vertebrae are there?
|
33: made of 5 segments
|
|
|
How many ribs are there?
|
12: 10 directly or indirectly attached to sternum
|
|
|
What is the kind of mesoderm on either side of the notochord?
|
Paraxial Mesoderm
|
|
|
What happens to the paraxial mesoderm on either side of the notochord?
|
Becomes segmented into paired condensations of mesenchyme called somites
|
|
|
What kind of tissue is in the somites?
|
- Initially mesenchyme
- Transformation to epithelial tissue |
|
|
Once the mesenchymal to epithelial transformation occurs in the somite, what happens?
|
Epithelial tissues become arranged around a central cavity called the Somitocoel
|
|
|
What kind of tissue forms from the ventromedial part of the somite? Dorsolateral part?
|
- Ventromedial - cartilage and bone precursors --> aggregate of mesenchyme (Scleratome)
- Dorsolateral - skeletal muscle and connective tissue precursors --> epithelial initially (Dermomyotome) |
|
|
What is the precursor tissue for the vertebrae development?
|
Scleratome Mesenchyme of somites (ventromedial) beginning with somite number 5-6
|
|
|
What happens to the first 4-5 somites?
|
Termed Occipital Somites - contributes to formation of basal portion of skull
|
|
|
What causes the somite differentiation into Scleratome?
|
Cells in ventromedial portion of somite are influenced by signals (Shh and noggin) originating from notochord and floor plate of neural tube
|
|
|
What happens after the ventromedial part of the somite is exposed to Shh and Noggin?
|
- Expresses transcription factors Pax1 and Pax9
- Causes proliferation - Epithelium to Mesenchyme Transformation = Scleratome |
|
|
What happens to the Scleratome cells after the epithelial to mesenchymal transformation?
|
Scleratome cells are displaced or migrate medially to surround the notochord and neural tube
|
|
|
How are the scleratome cells packed around the notochord and neural tube? Impact?
|
- Cranial half are loosely arranged
- Caudal half are condensed / tightly packed - This influences the outgrowth of migrating neural crest cells and spinal nerve axons (permitted to migrate over cranial half but inhibited from crossing caudal half) |
|
|
What happens to the scleratome subdivisions before forming vertebrae?
|
Resegmentation:
- Cranial half of one somite merges w/ caudal half of next adjacent somite - Vertebrae become INTERsegmental w/ respect to original somite segmental pattern |
|
|
What is the impact of having the resegmentation of scleratome subdivisions?
|
- Now muscles derived from dermatomes can span adjacent vertebrae
- Intersegmental arteries now pass across the body of a vertebrae and spinal nerves lie near the intervertebral discs |
|
|
What are the scleratome subdomains / compartments? What do they become?
|
- Central --> pedicle, proximal rib
- Ventral --> vertebral body (centrum), intervertebral disc - Dorsal --> dorsal part of neural arch, spinous process - Lateral --> distal rib - Somitocoel cells --> vertebral joints, intervertebral disc, proximal ribs - Medial --> meninges and blood vessels of spinal cord - Cells along lateral edge of central compartment (syndrome) --> tendons for epaxial muscles that attach to vertebrae |
|
|
What do the vertebral pedicle and proximal rib form from?
|
Central Scleratome
|
|
|
What do the veretebral body (centrum) and intervertebral disc form from?
|
Ventral Scleratome
|
|
|
What do the dorsal part of neural arch and spinous process form from?
|
Dorsal Scleratome
|
|
|
What does the distal rib form from?
|
Lateral Scleratome
|
|
|
What do the vertebral joints, intervertebral disc, and proximal ribs form from?
|
Somitocoel cells
|
|
|
What do the meninges and blood vessels of the spinal cord form from?
|
Medial Scleratome
|
|
|
What do the tendons for the expaxial muscles that attach to vertebrae form from?
|
Cells along the lateral edge of the central compartment (the syndrome)
|
|
|
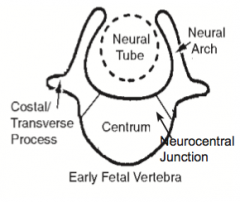
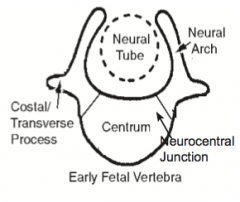
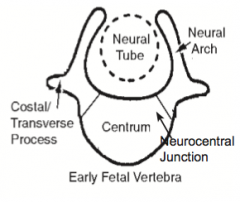
What extends from the neural arches of the vertebrae?
|
Costal and transverse processes
|
|
|
What structure is in between the base of the neural arch and the centrum? Function?
|
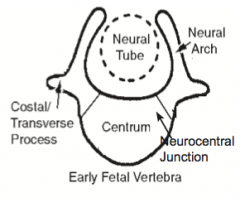
- Neurocentral Junction (synchondrosis) - a thin layer of cartilage
- Allows for growth of the vertebra |
|
|
What allows the vertebra to grow?
|
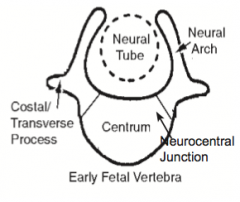
Neurocentral junction - thin layer of cartilage that remains between the base of the neural arch and the centrum
|
|
When does ossification of the Neurocentral Junction occur?
|
Prior to age 10 (or may remain intact until adolescence)
|
|
What happens when ossification unites the centrum and neural arch?
|
Portion at the base of the primitive neural arch becomes part of the body of the definitive vertebra
|
|
|
What does the intervertebral disc develop from?
|
At the intersegmental boundary from cells of the posterior scleratome and somitocoel cells
|
|
|
At the level of the discs, what does the notochord remain as?
|
Nucleus Pulposus
|
|
|
What is regionalization of the spine mediated by?
|
- Nested expression of Hox genes along the cranial-caudal axis of the embryo
- Hox gene expression is mediated by retinoic acid |
|
|
What happens if there are null mutations of Hox gene expression? Gain-of-function mutations?
|
- Null - tends to cranialize vertebral segments
- G.o.F. - tends to caudalize vertebral segments |
|
|
What is an example of regional variation in the spine?
|
Costal processes - each type of vertebra has a costal process, normally ribs grow from costal processes in thoracic region, in other regions, the costal processes become part of the transverse process
|
|
|
How do vertebrae form?
|
- Begin as cartilage models
- Ossify by endochondral ossification - 3-4 primary ossification centers form in cartilage model of each vertebra - Two formed in centrum may fuse, each arch has one center - Secondary ossification centers form at puberty on cranial and caudal surface of body of vertebra and on tips of spinous and transverse processes |
|
|
What are some types of abnormal development of the vertebral column?
|
Defects related to abnormal regionalization:
- Klippel-Feil sequence - Sacralized and lumbarized vertebrae Dysraphism Defects of formation |
|
|
What typically causes defects related to abnormal regionalization?
|
Abnormal signaling (e.g., retinoic acid) that leads to a shift in the nested pattern of Hox gene expression
|
|
|
What are the symptoms of Klippel-Feil sequence / Brevicollis?
|
- Presence of several fused cervical vertebrae
- Neck is shortened - Low nuchal hair line - Limited cervical spine mobility - 20-30% have undescended scapula, cervical rib, and some have scoliosis (60%) |
|
|
How common is Klippel-Feil sequence / Brevicollis - fused cervical vertebrae? How is it inherited?
|
- 1/40,000
- Recessive disorder |
|
|
What happens in Sacralized and Lumbarized Vertebrae?
|
- Number of vertebrae in a region of spine may vary
- Sacralization - 5th lumbar vertebrae is incorporated into sacrum - Lumbarization - 1st sacral vertebrae is not included in sacrum - Total number of vertebrae in spine remains unchanged |
|
|
What is Dysraphism?
|
Failure of fusion of neural arches of vertebrae
|
|
|
What is Rachischisis?
|
Condition where many or all vertebrae have unfused spinous processes
|
|
|
What is Spina Bifida? Mildest form?
|
- Term used to designate a series of conditions where one or a few adjacent vertebrae have unfused spinous processes
- Spina Bifida Occulta is the mildest form (20%) and is usually asymptomatic |
|
|
What are some examples of defects of formation of vertebrae?
|
- Hemivertebrae
- Wedge-shaped vertebrae - Unsegmetned vertebral bars |
|
|
What happens in a Hemivertebrae?
|
- Remainder of the vertebra that did not form completely
- Malformed vertebrae can create asymmetry in spine leading to abnormal curvatures such as scoliosis (lateral curvature) |
|
|
What causes the congenital form of Scoliosis?
|
Hemivertebrae, but in 80% of cases it is idiopathic (unknown)
|
|
|
What causes Kyphosis and Lordosis (exaggerations of primary curvatures of spine)?
|
- Congenital d/t vertebral malformation
- Acquired |
|
|
How do ribs form?
|
- Expansion laterally of costal processes from thoracic vertebrae
- Proximal portion from cells of central scleratome and somitocoel - Distal portion from cells of lateral scleratome - Primary ossification centers form in fetal period and secondary ossification centers during puberty |
|
|
How does the sternum form? What does it originate from?
|
- Independently as cartilage bars on either side of midline (during formation of ventral body wall in thorax)
- Bars fuse once embryo folding is complete in transverse plane - Secondary segmentation occurs forming several sternebrae - Primary ossification occurs in sternebrae during 5th motnh except for xiphoid process which ossifies during childhood - Sternal primordia derived from somatic mesoderm |
|
|
What happens to the sternebrae (formed from secondary segmentation)?
|
- Refusion of several sternebrae forms the body of the sternum
- Cranial most sternebrae remains unfused as the manubrium - Caudal most sternebrae remains unfused as the xiphoid process |
|
|
What are some anomalies of the ribs and sternum?
|
Ribs:
- Accessory ribs - Fused and forked ribs Sternum and Costal Cartilage: - Pectus Excavatum - Pectus Carniatum |
|
|
Where do accessory ribs form (anomaly)? How common and who is most likely to get them?
|
May occur in lumbar and cervical regions (0.2-8%) - males more by 3:1
|
|
|
How do fused and forked ribs affect a person?
|
Often asymptomatic
|
|
|
What happens in Pectus Excavatum?
|

- Posterior depression of sternum (hollow)
- May press heart against the spine and cause it to deviate left - Surgery may be necessary to reduce expression - Often an isolated anomaly |
|
|
What happens in Pectus Carniatum?
|

- Ventral protrusion of sternum (keel-shaped)
- Often isolated anomaly w/ prevalence in males of 4:1 |
|
|
What subdivides the limb into compartments?
|
Fibrous connective tissue
|
|
|
Like organs and other specialized structures, the limbs form within what structure?
|
Developmental fields - finite areas of embryo that develop into multiple and related structures
|
|
|
What are the phases of limb development?
|
1. Establishment of limb "field"
2. Budding (appearance) 3. Elongation of the limb 4. Tissue formation and organization |
|
|
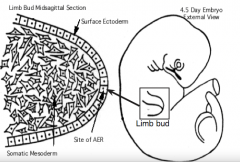
What are the limb precursor tissues?
|
- Somatic mesoderm - located on each side (flank region) of embryo at specific axial levels
- Covered by surface ectoderm - Somitic mesoderm (somite derived) - skeletal muscles - Neural crest - Schwann cells and spinal nerves |
|
|
What transcription factors are important for developing the upper limb?
|
Tbx5
|
|
|
What transcription factors are important for developing the lower limb?
|
Tbx4 and Pitx-1
|
|
|
How does the timing of the upper limb development compare to that of the lower limb development?
|
Upper limb is ahead of lower limb by about 1-2 days
|
|
|
What happens during the first step of limb development?
|
Establishment of limb "field"
- Areas of somatic mesoderm on each flank - Axial positioning is regulated by Hox genes - Specific transcription factors are expressed in each limb field: upper limb (Tbx5) and lower limb (Tbx4 and Pitx-1) |
|
|
What happens during the second step of limb development, after establishment of the limb fields?
|
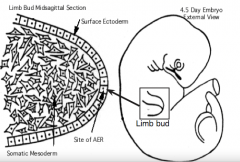
Budding (appearance)
- Small elevations appear on the side of the embryo at specific axial levels = Limb Buds - Production of Fgf-10 by mesenchyme cells causes surface ectoderm to form a thickened ridge of ectoderm = Apical Ectodermal Ridge (AER) |
|
|
What is the Apical Ectodermal Ridge (AER)?
|
Ectoderm thickening at dorsal / ventral surface interface
|
|
|
What happens during the third step of limb development, after budding?
|
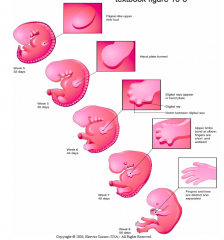
Elongation of the limb
- Limb bud elongates and changes shape from initial conical bud - Flat paddle-shaped hand or foot plate develops at distal end - Constriction separates plate from remainder of forming limb - Digital rays (future fingers and toes) begin to appear in hand and foot plates - UL digits completely separate, LL digits remain partially separated - Limbs rotate |
|
|
What happens during the fourth step of limb development, after elongation of the limb?
|
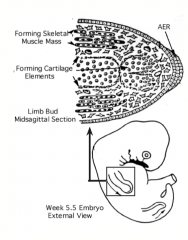
Tissue Formation and Organization
- Begins in proximal limb segment and continues distally - Centrally, somatic mesoderm condenses into cartilage models of limb bones - Somite-derived mesoderm cells migrate into limb to form skeletal muscles - Motor axons of spinal nerves enter limb - Guidance cues for muscle and nerve development are received from somatic mesoderm cells at base of limb bud |
|
|
What tissues form the cartilage models for limb bones? What tissues form the skeletal muscles?
|
- Cartilage models from somatic mesoderm
- Skeletal muscles from somite-derived mesoderm |
|
|
Where do the guidance cues for the muscle and nerve development come from?
|
Received from somatic mesoderm cells at the base of the limb bud
|
|
|
What axes does limb development occur along?
|

3 sets of linear axes simultaneously:
- Proximal-distal: limb outgrowth and elongation - Anterior-posterior: digits develop; limb develops cranial (preaxial) and caudal (postaxial) borders - Dorsal-ventral: muscles and neurovascular structures form and subdivided into compartments |
|
|
What is necessary for the development of a limb along the proximal distal axis?
|
Inductive interactions between the AER (apical ectodermal ridge) and the underlying somatic mesoderm
|
|
|
What happens if the AER (apical ectodermal ridge) is removed during limb formation?
|
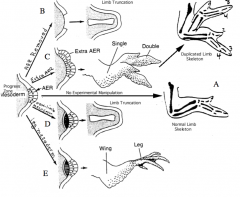
Development is stopped or truncated at that point (B)
|
|
|
What happens if an additional AER (apical ectodermal ridge) is grafted onto the limb?
|
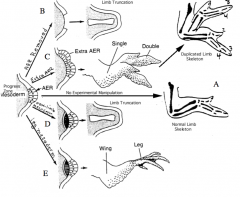
- There is an additional signaling center
- Leads to duplication of the limb structure from the time the graft is put in place (C) |
|
|
What happens if mesoderm other than limb bud mesoderm is placed adjacent to the Apical Ectodermal Ridge (AER)?
|
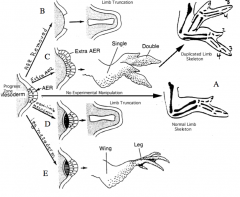
Limb development is truncated suggesting that ONLY limb mesoderm is competent to respond to signals from AER (D)
|
|
|
What happens if mesoderm from the lower limb bud is placed adjacent to the AER in the wing bud?
|
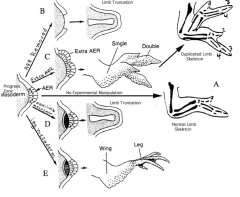
- Lower limb structures derived from mesoderm form, beginning from the time of graft placement (E)
- Limb bud mesoderm is programmed as to the axial level at which it is located |
|
|
What signal does the somatic mesoderm of the limb bud produce first? What does this do?
|
Produces Fgf-10 --> induces formation of AER
|
|
|
What signal does the AER (apical ectoderm ridge) produce? What does this do?
|
AER produces Fgf 8, 4, and 2 --> maintains Fgf-10 production in somatic mesoderm adjacent to AER --> promotes mesenchyme proliferation while inhibiting cell differentiation
|
|
|
What are the implications of AER (apical ectodermal ridge) producing Fgf 8, 4, and 2, besides that it maintains procution of Fgf-10 from somatic mesoderm?
|
- Promotes mesenchyme cell proliferation while inhibiting cell differentiation
- Results in limb bud elongation and segment formation |
|
|
Is the somatic mesoderm capable of producing the limb bud independently?
|
Yes - the somatic mesoderm can produce the limb bud independently of influence from the ectoderm, but it cannot sustain limb development further without AER-mesoderm interaction
|
|
|
What does the ZPA mesoderm do?
|
Produces Shh which maintains Fgf-8 secretion by AER until all segments of limb are formed
|
|
|
What is the fate of the mesenchyme adjacent to the AER (Apical Ectodermal Ridge)?
|
- Mesenchyme underlying AER is of somatic mesoderm origin
- 1st hypothesis: AER-derived signals inform mesenchyme where they should be in limb, depending on how long they are by signals determines fate (leave earlier = proximal; leave later = distal) - 2nd hypothesis: limb bud mesoderm fate is already predetermined and signaling from AER is necessary to expand and develop - Limb bud mesoderm forms cartilage model, fibrous CT to surround muscles and subdivide into compartments, and become superficial fascia, and dermis of skin |
|
|
The limb bud mesoderm turns into what structures?
|
- Cartilage models of limb and girdle bones
- Fibrous CT to surround muscles and subdivide limb into compartments - Superficial fascia - Dermis of skin |
|
|
What is the Zone of Polarizing Activity (ZPA)? Function?
|
- Group of somatic mesoderm-derived mesenchymal cells along posterior border of the limb
- Signaling center that secretes Shh and Retinoic Acid (RA) - Influences patterning along anterior-posterior axis of limb |
|
|
How was it determined that the Zone of Polarizing Activity (ZPA) had an influence on anterior-posterior patterning?
|
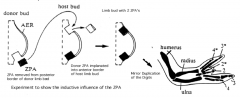
- Grafted a second ZPA into anterior border of limb bud
- Result is a mirror image duplication of digits in distal segment of limb |
|
|
What happens if beads soaked in Retinoic Acid and Shh are implanted into the anterior border of the limb bud?
|
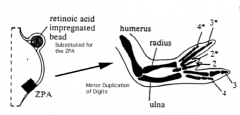
- Mimics action of Zone of Polarizing Activity (ZPA) - influences patterning along anterior-posterior axis of limb
- Induces asymmetric, nested expression of Hox genes that mediate the pattern for digit location along ant-post axis of limb bud |
|
|
On what border does the large digit (thumb/big toe) develop? On which border does the small digit (pinky) develop?
|
- Large digit = Cranial / Preaxial Border
- Small digit = Caudal / Postaxial Border |
|
|
What is the role of apoptosis in limb development?
|
- Separation of digits
- Absence of distal phalanx of large digit |
|
|
How do the digital rays (fingers / toes) separate?
|

- Apoptosis causes breakdown of the AER in the interdigital region
- AER remains intact at the tips of each digit until the correct length and number of phalanges is achieved - Then it disappears |
|
|
What is an example of patterning of the limb along the dorsal-ventral axia?
|
- Location of palm-sole, dorsum of hand-foot
- Influences skeletal muscles, neural and vascular structures, limb compartmentalizatoin |
|
|
What signals are used to mediate the dorsal-ventral axis patterning?
|
- Antagonism between gradients of dorsalizing and ventralizing signals
- Wnts and radical fringe expressed in dorsal ectoderm cause Lmx-1 expression in dorsal mesenchyme - Engrailed-1 expressed in ventral ectoderm prevents Lmx-1 expression in ventral mesenchyme - Dorsal ectoderm signals also maintain Shh production by ZPA and limit AER to distal tip of limb bud |
|
|
Skeletal muscles within the limb bud as well as associated with the pectoral and pelvic girdles are derived from what tissue?
|
Somitic (somite) mesoderm (ventrolateral part of myotome)
|
|
|
What axial levels are associated with the upper limb? lower limb?
|
- Upper limb: C5-T1
- Lower limb: L4-S3 |
|
|
What signals the myoblasts to migrate into the limb bud? Effect?
|
- Signals from mesenchyme at base of limb bud
- Myoblasts migrate into bud - Myoblasts organize into dorsal and ventral premuscle masses |
|
|
Where do the muscle patterning signals come from?
|
Believed to be derived from somatic mesoderm that forms the fibrous CT that will be associated w/ the various muscle groups
|
|
|
What might influence the splitting of the muscle masses into specific muscles?
|
Influenced by signals directing blood vessel patterning
|
|
|
What helps direct the neural structures / spinal nerves to their destination?
|
Guidance cues from mesenchyme cells at base of limb buds
|
|
|
Do sensory or motor fibers enter limb bud first?
|
Sensory fibers enter limb bud AFTER motor fibers
|
|
|
What happens to neural crest cells that enter the lib bud?
|
Form Schwann cells and melanoblasts
|
|
|
How do vascular structures develop in the limbs?
|
- Sprouts from intersegmental arteries enter limb buds and form a vascular plexus of endothelial-lined tubs
- Certain channels enlarge while others disappear - Extensive remodeling of plexus during limb formation leads to final vascular pattern - Marginal venous channels form along pre- and post-axial borders that will become components of superficial venous plexus |
|
|
What forms the cephalic vein in upper limb and greater saphenous vein in lower limb?
|
Venous channels on preaxial border
|
|
|
The venous channels on the preaxial border form what in the upper limb? lower limb?
|
- Upper limb = cephalic vein
- Lower limb = greater saphenous vein |
|
|
What forms under the ectoderm of the distal limb segment until all digits have formed?
|
A peripheral avascular zone
|
|
|
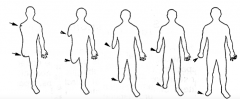
On what axis do the limbs rotate?
|
Proximal-Distal axis
|
|
|
What is the outcome of the limb rotation?
|
- Upper limb rotates laterally around the proximal-distal axis so that the thumb is lateral
- Lower limb rotates medially around axis so the large toe is medial |
|
|
What is the original position during development of the palm? After rotation?
|
- Devo (before rotation): medial
- Anatomical (after rotation): anterior |
|
|
What is the original position during development of the sole? After rotation?
|
- Devo (before rotation): medial
- Anatomical (after rotation): inferior |
|
|
What is the original position during development of the thumb? After rotation?
|
- Devo (before rotation): superior
- Anatomical (after rotation): lateral |
|
|
What is the original position during development of the big toe? After rotation?
|
- Devo (before rotation): superior
- Anatomical (after rotation): medial |
|
|
What is the original direction of movement of elbow flexion? After rotation?
|
- Devo (before rotation): medial
- Anatomical (after rotation): ventral (elbows facing dorsally) |
|
|
What is the original direction of movement of knee flexion? After rotation?
|
- Devo (before rotation): medial
- Anatomical (after rotation): dorsal (knees face ventrally) |
|
|
What is the original direction of movement of flexors? After rotation?
|
- Devo (before rotation): Ventral
- Anatomical (after rotation): Ventral (upper) or Dorsal (lower) |
|
|
What is the original direction of movement of extensors? After rotation?
|
- Devo (before rotation): dorsal
- Anatomical (after rotation): dorsal (upper) or ventral (lower) |
|
|
What are the types of limb malformations?
|
- Failure of formation of limb parts
- Failure of differentiation - Duplication of limb parts - Overgrowth (gigantism) of limb part - Undergrowth (hypoplasia) of limb part - Congenital constriction band syndrome - Generalized skeletal abnormalities |
|
|
What is it called when all of a limb is missing? part of a limb?
|
- Amelia = all of limb missing
- Meromelia = part of limb missing |
|
|
What are some possible Meromelias (absence of limb parts)?
|
- Missing preaxial or anterior structures (e.g., radius + digits 1, 2 and 3)
- Missing postaxial or posterior structures (e.g., Ulna + digits 4, 5 - Absence of limb structures in median portion of distal limb segment (e.g., digit 2, 3, or 4) = Oligodactyly |
|
|
What is Oligodactyly?
|

- AKA lobster claw deformity
- Can affect the hand or foot |
|
|
What happens in Phocomelia or seal limb?
|
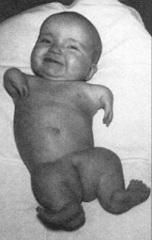
- Distal segment of limb is attached to a more proximal segment w/ intervening segment missing or directly attached to shoulder girdle
- Common in children born to mothers w/ take drug Thaladomide during pregnancy (anti-nausea) |
|
|
What happened to mothers who took Thaladomide during pregnancy?
|
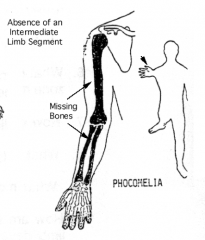
Babies were at high risk for Phocomelia (or seal limb) where distal segment of limb is attached to a more proximal segment w/ intervening segment missing or directly attached to girdle
|
|
|
What happens in "Syndactyly"?
|

- Complete or partial fusion of one or more digits
- 1/2200 live births - May be due to failure of interdigital apoptosis |
|
|
What happens in "Sirenomelia"?
|

- More severe and very rare birth defect
- Fused limb fields or abnormal development of tailbud - 1/25,000 - 50,000 |
|
|
What happens in "Polydactyly"?
|

- Duplication of limb parts, especially digits
- Inherited (autosomal dominant or recessive) - Usually bilateral |
|
|
What happens in "Diplopodia"?
|

- Duplication of portion of limb occurs, usually distal segment
- May involve formation of extra digits that are arranged in a mirror image to other digits present - May result from duplication of AER signals during limb elongation |
|
|
What is an example of overgrowth (gigantism) of a limb part?
|

- Very rarely some parts of limb become hypertrophied
- Macrodactyly or large digit - Usually not bilateral |
|
|
What is an example of undergrowth (hyperplasia) of a limb part?
|

Brachydactyly - digit is shortened due to lack of certain joints
|
|
|
What happens in Congenital Constriction Band Syndrome?
|
- Pieces of amnion break away as bands of tissue
- Wraps around forming limb or a portion of it causing an amputation - Deformation of development rather than a defect |
|
|
What is Arachnodactyly? What condition is this a part of?
|
- Long thin digits
- Part of Marfan syndrome |
|
|
What are some anomalies related to the lower limb?
|
- Clubfoot
- Developmental dysplasia of the foot |
|
|
What kind of anomaly is "clubfoot"?
|
* Any foot-ankle defect involving the Talas bone
- Multifactorial inheritance - Deformation, due to uterine pressure when foot placement is abnormal, may be involved when it is easily corrected after birth - Increased incidence associated w/ smoking |
|
|
What is the most common type of Clubfoot?
|
Talipes Equinovarus (1/1000)
- Varus = limb is bent inward toward midline - Foot is plantar-flexed, inverted, and adducted - Navicular, calcaneus, and cuboid bones are displaced around talus - More common in boys 2:1 |
|
|
What is it called when the hip joint is easily dislocated, usually after birth?
|
Developmental Dysplasia of the Hip
|
|
|
What happens in Developmental Dysplasia of the HIp?
|
- Hip joint is easily dislocated
- Underdevelopment of femoral head and/or hip socket - Often accompanied by general joint laxity and breech births (child born feet first) |
|
|
What makes Developmental Dysplasia of the hip more likey?
|
- Breech births
- Maternal hormones that soften CT - Positioning in uterus - Hereditary component sometimes |
|
|
What are some examples of intrauterine compression syndromes?
|
- Developmental dysplasia of the hip
- Congenital idiopathic club foot - Torticollis (head turned to one side) - Congenital constriction band syndrome |
|
|
What is the cause of intrauterine compression syndromes? What is the outcome?
|
- Abnormal pressures that impact the growing fetus while still in the uterus
- Some are mild and easily treated, while others are severe |
|
|
What happens in Cleidocranial Dysplasia?
|

- Hypoplasia (decreased size) or Aplasia (absence) of clavicles
- Usually bilateral - Large head, small face, long neck, drooping shoulders, short narrow chest |
|

What other anomalies are associated w/ Cleidocranial Dysplasia?
|
- Delayed fontanelle closure
- Incomplete pubic development - Short fingers - Dental problems |
|

What is a possible cause of Cleidocranial Dysplasia?
|
- Autosomal dominant inheritance
- Can be from new mutation - Only known gene affect is Runx-2 gene |
|
|
What is the name of the deformity when the scapula is undescended?
|
Sprengel Deformity
|
|
|
What happens in Sprengel Deformity?
|
- Undescended scapula (C4-T2 instead of T2-T7)
- Dysplastic scapula - Usually left scapula is affect, but can be bilateral - Muscles associated with scapula are hypoplastic or atrophic - limits shoulder movement and causes disfigurement |
|
|
What is the most common defect affecting the shoulder?
|
Sprengel Deformity - undescended scapula
|
|
What other anomalies are associated w/ Sprengel Deformity?
|
- Vertebral anomalies
- Absent or fused ribs - Klipple-Fiel sequence - Scoliosis |

