![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
|
What is the most common form of hospitalized AKI?
and how serious is it? |
Ischemic acute tubular necrosis - 50% hospitalizations
50% mortality in ICU patients 3 fold higher mortality in patients in a non-ICU setting |
|
|
What are some exogenous and endogenous toxins causing acute tubular necrosis?
|
Exogenous: radiocontrast IV dye, lead, mercury, chemoptherapy, herbal meds, gentamicin
Endogenous: multiple myeloma, hemoglobinuria, uric acid crystals. |
|
|
In ATN, what are some histologic changes you would see in the tubules?
|
Loss of brush cell borders
Flattened epithelium Loss of polarity Loss of tight junctions Decrease in capillary bed area (post ischema) Apoptosis (distal tubule) |
|
|
What would be found in a urinalysis in ATN?
|
Muddy brown casts (pathognomonic)
Early: epithelial cell casts Late: granular casts " |
|
|
"With ATN, would you expect an FeNa <1% or >2%?
Why is water wasting seen? (UOsm <350 mOsmol/kg)" |
High urine sodium, so expect FeNa >2%
The urine concentration defect is due to: i) no hypertonic medullary gradient ii) Loss of aquaporin 2 expression, which is the site of ADH |
|
|
What would you see clinically in each of the 3 stages of acute tubular necrosis?
|
1. Initiation: abrupt rise in urea, serum creatinine and decreased urine output
Maintenance: sustained low GFR. Increased urea and creatinine 2. Diuretic: (careful replacement of fluid & lytes) 3. Recovery: Gradual fall in creatinine and urea |
|
|
What is going on at the level of the tubules at each of the stages of ATN?
|
1. Initiation: tubular injury
Maintenance: Tubular injury. Activation of tubulo-glomerular feedback, which leads to afferent arteriole vasoconstriction 2. Diuretic -phagocytosis of debris; regeneration of undifferentiated tubules 3. Recovery -differentiated tubular epithelial cells & normal tubular function |
|
|
How do you treat ATN?
|
trea pre-renal AKI, and/or underlying cause early (rhabdomyolysis, hemolysis, avoid nephrotoxins, sepsis)
hold ACEi, ARB |
|
|
What are some agents that cause allergic interstitial nephritis?
|
antibiotics: beta lactams, sulfa, fluoroquinolones
PPIs diuretics Phenytoin NSAIDs Phosphate fleet enemas |
|
|
other causes of acute interstitial nephritis?
|
Malignant infiltration (lymphoma, leukemia, plasma cells in myelona
glomerulonephritis pyelonephritis AI disorders (lupus, scleroderma) |
|
|
What are some clinical signs suggesting allergic interstital nephritis?
|
Maculopapular rash
Fever arthralgias icnreased IgE hepatitis Delayed creatinine rise (up to 2 weeks post exposure) |
|
|
What could urinalysis of someone with allergic interstitial nephritis have? kidneys?
|
WBC, WBC casts
Mild proteinuria Microscopic hematuria Kidneys can be normal or enlarged |
|

What effect will afferent arteriole vasoconstrictors have on GFR? What are some agents/conditions causing vasoconstriction of the afferent arterioles?
|
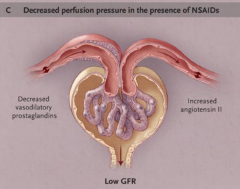
Decrease GFR.
NSAIDs, cyclosporin, tacrolimus, hypercalcemia, sepsis Loss of vasodilatory prostaglandins increases afferent resistance; this causes the glomerular capillary pressure to drop below normal values and the GFR to decrease. |
|

What is the effect on GFR and serum creatinine with efferent arteriole vasodilation? What are agents that will cause this?
|
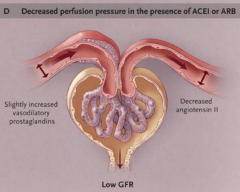
Decreased GFR & increased serum creatinine
ARB & ACEi Loss of angiotensin II action reduces efferent resistance; this causes the glomerular capillary pressure to drop below normal values and the GFR to decrease. |
|
|
What condition causes the classic triad of: AKI, eosinophilia & livedo reticularis?
|
Cholesterol emboli, a type of vascular intrarenal AKI
|
|
|
What are some extra renal manifestations of cholesterol emboli? What are risk factors for this disease?
|
Hollenhorst plaques (cholesterol emboli
CNS ischemic signs & symptoms Acute respiratory distress Abdominal pain, GI bleed Skin gangrene, cyanosis, ulcers, blue toe syndrome Risk factors: vascular disease, thrombolytics, anti-coagulation |
|
|
Which of the following situations would you NOT use a renal biopsy?
unknown cause of AKI hydronephrosis acute tubular necrosis treatment guidance Prognosis Cholesterol emboli Rapidly progressing glomerular nephritis nephrotic syndrome Churg-Straus |
"- acute tubular necrosis, cholesterol emboli, Churg Straus, hydronephrosis
Also use it for: Select cases of isolated proteinuria or hematuria (eg unusual clinical course), suspected genetic disease" |
|
|
List some contraindications for renal biopsy.
|
multiple, bilateral cysts
one kidney (transplanted one ok) atrophic <8-9cm, hyperechoic hypdronephrosis uncontrolled HTN renal tumor renal infection or on overlying skin uncooperative patient/difficult positioning |
|
|
What are some metabolic consequences of AKI?
|
Hyperphosphatemia
hyperkalemia acidosis uremia & uremic complications drug intoxication volume overload |

