![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
What percentage of our total body weight is water? How is this water distributed (compartment-wise)?
|

60% (males), 50% (females)
40% - intracelluar fluid (or 2/3 of water) 20% - extracellular fluid (or 1/3 of water) only force at play at the cell membrane is osmotic gradient |
|
|
What are the divisions of fluid in the ECF?
And the main force? |
Interstitial fluid (3/4 of ECF)
Plasma (1/4 ECF) movement across the capillary wall depends on water gradients and hydrostatic gradients |
|
|
What is the main cation in the extracellular fluid (ECF) compartment? The intracellular fluid (ICF) compartment?
|
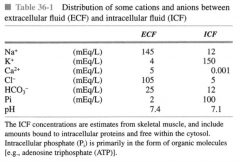
ECF: Sodium - Na+
ICF: Potassium (K+) |
|
|
Can you change the amount of ICF Na?
|
No. The Na/K pump regulates this
|
|
|
"What is the formula for osmotic concentration?
Ex: What is the osmotic concentration of 100 M NaCl?" |
!["Osmotic concentration = {# of dissociated particles} x [solute]
Ex: 200 M - because NaCl dissociates into 2 particles"](https://images.cram.com/images/upload-flashcards/61/90/61/2619061_m.png)
Osmotic concentration = {# of dissociated particles} x [solute]
Ex: 200 M - because NaCl dissociates into 2 particles |
|

What will happen to a cell in a solution of 290 mOsm/L? In a solution of 360 mOsm/L? In a solution of 200 mOsm/L?
|
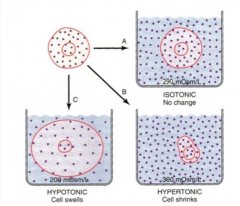
This is based on normal sodium concentration of 145 mEq/L.
A) No change (isotonic solution) B) Cell shrinks, exodus of water (hypertonic solution) C) Cell expands, influx of water (hypotonic solution) |
|
How is water lost to maintain water balance?
(Fill in the arrows above) |
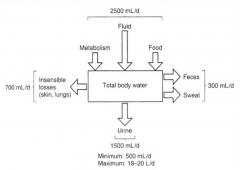
"1) Insensible losses (i.e. losses we can't regulate) - evaporation, respiration
2) Sweat and feces 3) Urine (primary source of water loss)" |
|
|
What is meant by the "minimum urine volume"?
|
"The minimum amount of urine the kidneys have to produce in order to remove all the waste products. If you go below the minimum output, you are considered to be in renal failure.
In lecture, he gave an example of 500 mL." |
|
|
What occurs physiologically when there is an increase in plasma osmolality (ex. during dehydration)? Where are the sensors located?
|

1) The thirst centre will be triggered
2) ADH release, triggering water reabsorption The osmoreceptors are located within the hypothalamus. |
|
|
Where is ADH produced and how is its release regulated?
|
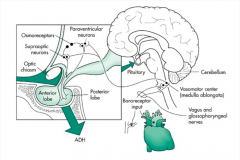
Two clusters of neurons (supraoptic and paraventricular) in the hypothalamus are responsible for the production of ADH.
Their axons terminate within the posterior pituitary, where they are released. Its release is regulated by osmoreceptors and in part by baroreceptors. ADH is released at 280 normal osmolarity is 290, so there is always circulating ADH |
|
|
What has to happen for baroreceptors to stimulate the release of ADH?
|
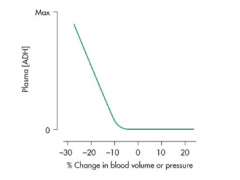
There must be a decrease in circulating volume (drop in blood pressure) to stimulate ADH release to restore circulating volume.
|
|
|
What sets up the osmotic gradient in the distal tubule (i.e. the cortex) that allows ADH to stimulate water reabsorption?
|
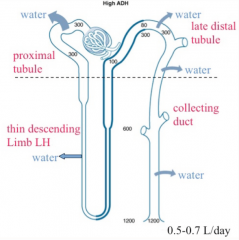
The sodium reabsorption in the ascending loop of Henle and the early distal tubule (both water impermeable) results in a concentrated area in the interstitial environment
Once ADH is present and water channels open, there is an osmotic gradient present and water reabsorption follows. |
|
|
What sets up the osmotic gradient in the collecting duct (i.e. the medulla) that allows ADH to stimulate water reabsorption?
|
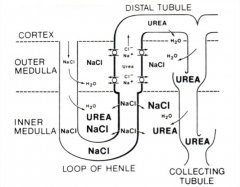
1) The sodium transport that occured in the loop of Henle, increasing the osmolarity of the interstitial environment.
2) The addition of urea by the inner medullary collecting duct. These both create a large concentration gradient, allowing water to be reabsorbed in the presence of ADH. |
|
|
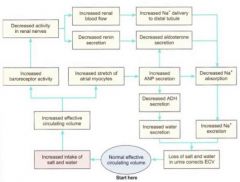
what are the responses to dehydration and excess hydration
|
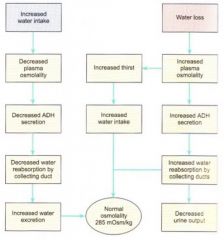
|
|
|
How would any acute increases in sodium intake affect the kidney?
|
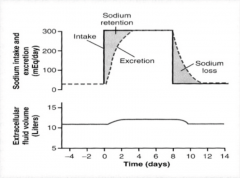
There would be an increase in sodium excretion by the kidneys, but the response would be much more sluggish (days) than that of a water-ADH repsonse.
ECF volume would increase, along with body weight. |
|
|
Describe edema in terms of changes in ECF
|
There is not an actual change in the overall amount of ECF instead there is only a change in the ratio of volume from the vascular compartment to the interstitial compartment
|
|
|
How does the kidney know when to increase or decreases sodium excretion?
|

Based on baroreceptors sensing circulating volume located in cardiovascular organs. The baroreceptors stimulate the SNS, which has a direct effect on the level of sodium excretion within the kidneys. Effects are to increase reabsorption of Na at the PCT
The SNS also stimulates the renin - angiotensin - aldosterone system. |
|
|
Describe the production of angiotensin II.
|

1) Low blood volume stimulates renin release from the kidney.
2) Circulating angiotensinogen from the liver is converted to angiotensin I by renin. Angiotensin I has no physiological function. 3) Angiotensin I is converted by angiotensin converting enzyme (ACE) in capillary networks (primarily in the lungs) to angiotensin II |
|
|
What are the physiological effects of angiotensin II?
|

1) Vasoconstriction targeting blood vessels to increased blood pressure.
2) Acts on the hypothalamus to increase thirst and through ADH release, stimulating water reabsorption. 3) Acts on the proximal tubules of the kidney directly to stimulate the reabsorption of sodium. NA/H pump 4) Acts on the adrenal cortex to release aldosterone and increase sodium reabsorption by the late distal tubule and collecting duct. |
|
|
What are four means at which the body maintains appropriate renin levels?
|
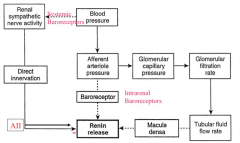
1) Systemic baroreceptors within blood vessels. which will adapt and therefore lose effect over time
2) Intrarenal baroreceptors within the kidney. Don't adapt 3) NaCl levels within the tubular fluid of the macula densa in the distal tubule. 4) Product inhibition of circulating angiotensin II (negative feedback) |
|
|
What are two pharmacological means of regulating circulating angiotensin II levels?
|
1) ACE inhibitors - target the converting enzyme
2) AT1 receptor blockers - block receptors on the proximal tubule cells, reducing the effects of circulating angiotensin II levels. |
|
|
What hormone allows the kidney to get rid of excess fluid?
|
Atrial natriuretic peptide (ANP) - released by the muscle cells within the atria of the heart.
|
|
|
How does atrial natiuretic peptide work?
|
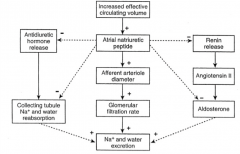
1) It is a powerful vasodilator, targeting the afferent arteriole, leading to an increased GFR and sodium and water excretion.
2) It targets sodium transport, inhibiting sodium reabsorption in the distal tubule and collecting duct. 3) It blocks ADH and renin release and interferes with aldosterone release, hormones that normally increase sodium and water retention. |
|
|
overview of response to volume depletion
|

|
|
|
Overview of response to volume expansion
|
|

