![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
The normal kidney is located
- in the peritoneum/retroperitoneally? - hundreds/thousands/millions of nephrons? |
The normal kidney is located retroperitoneally
Has millions of nephrons |
|
|
On U/S you can examine...
|
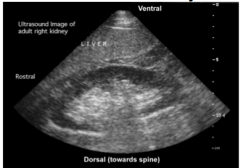
- size 9-11cm
- appearance (cortex and medulla) - evidence of hydronephrosis (obstructions) |
|
|
3 Components of the kidney
|
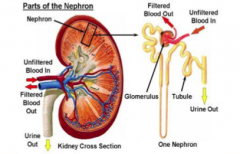
1) Glomerulus
2) Tubulointerstitium 3) Blood vessels |
|
|
Methods to determine/estimate the GFR
|
1) Creatinine based calculations
2) Creatinine clearance (urine [Cr], plasma [Cr] and urine volume) 3) eGFR formulas 4) nuclear medicine GFR scans Normal GFR for adults should be 180L/day --100 -125mL/min |
|
|
Causes of Increased Serum Creatinine (4)
Caused of decreased serum creatinine (3) Ranges in adult males, females and children/infants |
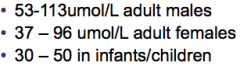
Increased
- low GFR - increased muscle mass - skeletal muscle damage - high meat or creatine intake Drecreased - high GFR - decreased muscle mass - advanced age (related to muscle mass) |
|
|
Creatine clearance formula
|
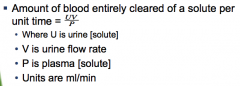
|
|
|
Cockcroft-Gault formula of creatine clearance
|
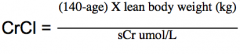
- it can estimate GFR
- remember to multiply by 1.2 if male |
|
|
Why CrCl does not = GFR
|
- creatinine is secreted from the tubules as well as filtered at the glomerulous
- normally this is 10% but as GFR decreases, this proportion increases up to 40% - as renal function declines, creatinine overestimates GFR |
|
|
eGFR
|
Similar to Cockcroft-Gault but use MDRD equaltion that uses creatinine, age, gender and black vs white in the calculation
|
|
|
What things are routinely noted/grossly measured on urinalysis?
|
"Noted
- appearance - sediment - Culture and cytology Measured by dipstick - pH - protein - blood - glucose other things too but I don't care |
|
|
What can be the components of urine sediment? (6)
|
RBCs
WBCs Casts crystals oval fat bodies other cells (epithelial) |
|
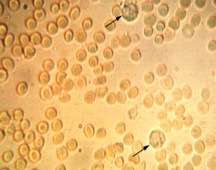
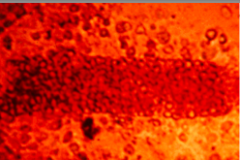
Identify this urine sample
|
hematuria
- normally would have 0-3 RBC/field the big guys are dysmorphic RBCs |
|
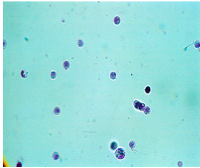
What is in this urine
|
White blood cells
|
|
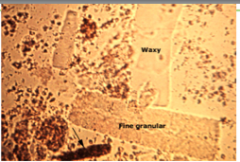
What is in this urine?
|
Granular casts
- can form in any proteinuric condition - may be stages of degenration of cellular casts - may indicate chronic renal disase but may also be non-pathologic (eg after exercise) |
|
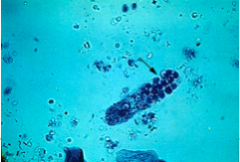
What is this in the urine?
|
Red blood cell cast
- pathologic - virtually diagnostic of some form of glomerulonephritis or vasculitis - absence does not eliminate glomerular disease |
|
What is this in the urine?
|
WBC cast
- pathologic - indicative of infection or inflammation at some site in the urinary tract - can localize the lesion to the kidney in pyelonephritis |
|
|
Features of Hematuria
|
1) Macro vs microscopic
- differentiate "red" blood from hematuria. Red can be from beets, drug metabolites, uric crystals - macroscopic visually red vs microscopic determined by dipstick. - need to visually confirm dipstick + hematuria as + dipstick can be from RBC, heme, myoglobin 2) Sources - anywhere from the kidney to the urethra Extra-renal sources: tumours, vascular malformations, cystitis, trauma, stone Renal: glomerular (glomerularnephritis), tubulointerstitial disease, pyelonephritis, polycystic kidney disease, stones |
|
|
You are a GP and find hematuria on dipstick in a patient, before you refer to a nephrologist you must
|
1) repeat the urinalysis to ensure it is persistent - if it's a lady make sure 2wks post LMP
2) rule out extrarenal sources - Hx, imaging (U/S, cystoscopy) ex) if you have a 40 year old make smoker with persistent hematuria, send him to the urologist as he is more likely to have a tumour |
|
|
Say you are a nephrologist with a referral for persistent hematuria from a GP, what are the next things you would do?
|
1) Try to differentiate b/w glomerular and non-glomerular disease
- glomerular would have more dysmorphic RBCs, RBC casts, significant proteinuria 2) consider renal biopsy |
|
|
What is proteinuria made of?
How much protein in the urine is normal? |
- made up of albumin and/or mucoprotein (made by tubular cells)
- normal is <150mg/day **know this** - pathologic if >300mg/day |
|
|
What is the screening test for proteinuria?
What is the diagnostic test for proteinuria? What is an estimate of proteinuria quantitation? |
Screening test = dipstick. Only detects albumin
Diagnosis/quanitation = 24hr urine collection |
|
|
I am a GP, I have a patient with a positive urine dipstick for protein, what do I do before referring to the nephrologist?
|
repeat urinalysis - need + on 2/3 collections for referral
|
|
|
What are the 2 main classifications of proteinuria?
|
Benign vs Pathologic
|
|
|
2 main classifications of benign proteinuria and investigations warranted
|
A) Transient/fucntional
- caused by fever, exercise, stress, cold - normal renal function and BP - lasts a few hrs to days - no further investigations needed b) Orthostatic - intermittent, only occurs durring the day when the person is upright - asymptomatic, normal renal function and BP - investigate by doing a split urine collection (day vs night) - excellent prognosis |
|
|
3 classifications of pathologic proteinuria
- cause - range of proteinuria |
1) Glomerular aka glomerulonephritis
- main cause of proteinuria once benign is ruled out - caused by increased permeabilty of the Glomerular BM - 300mg - 40g/day 2) Tubular - tubulointerstitial disease impairs the ability of prox tubule to reabsorb small MW proteins that are normally filtered - 300mg - 1g/day (max 2g/day) 3) Overflow - increased serum levels of small MW proteins that overwhelm tubular reabsorption (ex multiple myeloma) - 300mg to >10g/day |
|
|
8 ways kidney disease can manifest
|
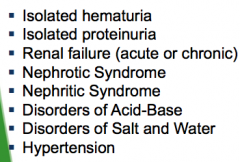
|

