![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
124 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Septic bursitis Causative agent |
S. Aureus |
|
|
|
Osteoarthritis Definition |
Chronic joint disorder, progressive softening and disintegration od articular cartilage, formation of new cartilage and bone, and capsular fibrosis |
|
|
|
Osteoporosis Causes |
Disparity between stress applied to articular cartilage and ability of cartilage to withstand that stress |
|
|
|
Osteoporosis Process |
1. Weakening of articular cartilage (deficiency of collagen type II or enzymatic activity) 2. Increased mechanical stress (excessive impact loading or reduction in articular contact area) |
|
|
|
Osteoarthritis Pathology |
1. Progressive loss of articular cartilage thickness 2. Remodeling of bone and osteophyte formation 3. Subarticular cyst formation and sclerosis 4. Capsular fibrosis 5. Synovial irritation |
|
|
|
Osteoarthritis Capsular fibrosis |
In late stages, may account for joint stiffness |
|
|
|
Osteoarthritis Cause of pain |
Capsular fibrosis (stretching) And vascular congestion causing an increase in intra-oseous pressure |
|
|
|
Osteoarthritis Risk factors |
1. Joint dysplasia 2. Trauma 3. Occupation 4. Family history |
|
|
|
Osteoarthritis Joint dysplasia |
1. Congenital acetabular dysplasia 2. Perthes disease 3. Slipped upper femoral epiphysis |
|
|
|
Osteoarthritis Trauma |
Fractures involving articular surfaces, it may caues joint instability |
|
|
|
Osteoarthritis Clinical features |
1. After middle age (if younger there is hx of joint injury or disorder) 2. One or two large joints 3. Insideous and increasing pain, intermittent, increased by exertion and decreased by rest 4. Stiffness, swelling, deformity, tenderness, crepitus,loss of mobility, and muscle wasting 5. No systematic manifestations |
|
|
|
Osteoarthritis X-Ray |
1. Narrowing of joint space 2. Subarticular cyst formation and sclerosis 3. Osteophyte formation |
|
|
|
Osteoarthritis Clinical variants |
1. Mono- an pauci-articular 2. Polyarticular (most common, middle aged women, distal finger joints) 3. Unusual sites (shoulders, elbow, wrist, ank ankle. Suspect previous abnormality) |
|
|
|
Osteoarthritis Early treatment |
1. Relieve pain (analgesics and NSAIDs) 2. Increase movement 3. Load reduction (walking stick, soft-soled shoes) |
|
|
|
Osteoarthritis Late treatment: surgical |
1. Joint replacement (total, partial, or excisional fibroblasty) 2. Arthrodesis (best choice in wrist, ankle, interphalangeal joints, and spine) 3. Arthroplasty (best in elbow joint destruction, in metacarpophalangeal joints for cosmetic aim) |
|
|
|
Osteochondrosis Definition |
Group of conditions where there is compression, fragmentation, or seperation of small segment of bone at bone end at articular surfaces |
|
|
|
Osteochondrosis Characteristics |
Interruption of blood supply, followed by necrosis and regrowth of bone later on Features of ischemic necrosis (increasing vascularity and reactive sclerosis) |
|
|
|
Osteochondrosis Pathophysiology |
Impact injury on subarticular bone, edema and bleeding, compression on capillaries and thrombosis, this leads to ischemia and necrosis |
|
|
|
Osteochondrosis Clinical features |
Usually in adolescents and young adults (osteochondrosis dissecans) Intermittent pain, swelling and small effusion Locking of joint or 'giving-way' (if necrotic part is completely detached) |
|
|
|
Osteochondrosis Panner's disease |
Humeral capitellum |
|
|
|
Osteochondrosis Freiberg's disease |
Head of second metatarsal |
|
|
|
Osteochondrosis Keinbock's disease |
Carpal lunate Causes considerable swelling |
|
|
|
Osteochondrosis Legg-Calve-Perthes disease |
Involves hip and causes a limp |
|
|
|
Osteochondrosis Schuermann's disease |
Involves spine and may cause kyphosis giving a 'hunchback' appearance |
|
|
|
Osteochondrosis Imaging |
Early changes: MRI Late: X-ray, radiolucent line line or demarcation |
|
|
|
Osteochondrosis Treatment |
Early stages: load reduction and restriction of activity Complete healing in young people (may take up to 2 years) |
|
|
|
Osteochondrosis Surgical treatment |
For large joints Partially detached fragments are pinned back in place after roughing up the surface Completely detached fragments are pinned back only if completely preserved |
|
|
|
Osteonecrosis Definition |
Avascular necrosis or bone infarction Death of bone tissue due to interruption of blood supply |
|
|
|
Osteonecrosis Clinical features |
Early: no symptoms Gradually: joint pain and limited mobility of joint, joint stiffness, local tenderness 30-50-year-olds Males>Females |
|
|
|
Osteonecrosis Risk factors |
1. Bone fractures 2. Joint dislocation 3. Alcoholism 4. Use of high dose steroids |
|
|
|
Osteonecrosis Most common sites |
1. Femur head and condyles 2. Head of humerus 3. Proximal talus and scaphoid |
|
|
|
Osteonecrosis Cells affected |
Hematopoeitic stem cells are first to die, within 12 hrs Bone cells die after 12-48 hrs Bone marrow fat cells die after 5 days |
|
|
|
Traumatic osteonecrosis Hip |
In fractures and dislocations of hip: reticular vessels supplying head of femur are easily torn, also damage and thrombosis of ligamentum teres |
|
|
|
Traumatic osteonecrosis Wrist and ankle |
In fractures of scaphoid and talus: proximal fragments are affected (supply from distal to proximal) |
|
|
|
Non-traumatic osteonecrosis |
1. Bone infections 2. Perthes' disease 3. SCD, Gaucher's disease, hemoglobinopathies 4. Corticosteroid administrations and alcohol abuse 5. Caisson disease 6. Ionizing radiation |
|
|
|
Non-traumatic osteonecrosis Corticosteroid administration |
1. High-doses: immunosuppression 2. Low-doses with other risk factors 3. Combinations: with azathioprine or previous alcohol abuse |
|
|
|
Osteonecrosis Imaging X-ray |
Changes appear after months Distinctive feature: subarticular increased bone density (due to reactive bone formation in surrounding tissue) Later changes: fractures and collapse Joint space is normal (no destruction to articular cartilage) |
|
|
|
Osteonecrosis Imaging Radioscintigraphy |
May reveal avascular segment (cold area signifying diminished activity) More often, increased activity, reflecting hyperemia and new bone formation |
|
|
|
Osteonecrosis Imaging MRI |
Only reliable method of picking up early signs of osteonecrosis |
|
|
|
Osteonecrosis Treatment |
Medication, not walking on affected leg, stretching, And surgery (core decompression, osteotomy, bane grafts, and joint replacement: total or partial) |
|
|
|
Osteomyelitis Definition |
Infection of bone marrow It is more common in children than adults |
|
|
|
Osteomyelitis Risk factors |
1. Diabetes 2. IV drug use 3. Splenectomy 4. Trauma |
|
|
|
Osteomyelitis Most common sites of infection |
Children: long bones of arms and legs especially around the knee (distal femur and proximal tibia) (metaphysis has high blood flow with low velocity, bacterial loading, risk of infection) Adults: vetebrae, then feet and hip |
|
|
|
Osteomyelitis Most common causative organism |
Usually bacterial, rarely fungal *neonates: part of neonatal sepsis *<1 year: klebsiella, listeria, E. coli, S. aureus, Group B streptococci *1-4yrs: S. aureus, H. influenzae, pneumococcus *>4yrs: S. aureus *SCD: S. aureus then Slamonella |
|
|
|
Osteomyelitis Salmonella osteomyelitis is most common in |
Sickle Cell Disease |
|
|
|
Acute OM History |
Previous URTI (or any infection), previous surgery, trauma, or open fractures 50% have history of trauma |
|
|
|
Osteomyitis Acute OM Physical exam |
Swelling, redness, warmth, and a very tender limb, decreased range of motion |
|
|
|
Acute OM Symptoms |
*pediatrics: failure to thrive, irritable, refuse feeding, tender, decreased range of motion *adults: back pain mainly, throbbing pain, due to pus accumulation and increased intra-oseous pressure) |
|
|
|
Acute OM Routes of infection |
1. Hematogenous 2. Direct inoculation 3. Direct spread |
|
|
|
Acute OM Routes of Infection: Hematogenous |
After infection, bacteria spread by blood reaching blood vessels supplying metaphysis, velocity reaches zero, stagnation of blood, increased risk of infection In vertebrea: valveless veins, stagnation and lodging of bacteria |
|
|
|
Acute OM Routes of Infection: direct inoculation |
Open fractures, or post surgical |
|
|
|
Acute OM Routes of Infection: direct spread |
Diabetic foot, or pressure sores |
|
|
|
Acute OM Pathophysiology |
Infection, inflammation, vasodilation leads to: 1. Increased IOP and decreased perfusion pressure 2. Decrease blood supply, and ischemia 3. Thrombosis from pus formation, digests vessel wall in addition to stasis from its accumulation 4. All lead to elevation of periosteum and further decrease of blood supply |
|
|
|
Osteomyelitis Cloaca definition |
Opening in involucrum allowing drainage of exudate and necrotic material out of dead bone Sign of chronic OM |
|
|
|
Osteomyelitis vs septic arthritis |
1. OM is a gradual process (Acute OM takes 12-24 hrs), less acute than septic arthritis 2. OM there is limited ROM, but septic arthrritis no ROM 3. If OM spreads to a bone it can cause 2°ry septic arthritis |
|
|
|
Osteomyelitis Differential diagnosis |
Cellulitis where the most common causative organism is S. Pyogen |
|
|
|
Osteomyelitis X-ray findings |
Sequestrum (dead bone) appears a bit whiter than normal bone Involucrum (formation of new bone, also called periosteal reaction) is the first sign that appears on x-ray, appears after 2 weeks (already became chronic OM) |
|
|
|
Subacute OM Brodies abscess definition |
Conversion as a draining abscess estending from tibia out through the shin, contained to a localized area and walled off by fibrosis and granulation tissue |
|
|
|
Subacute OM Most common microorganism |
S. Aureus |
|
|
|
Subacute OM Most frequent sites |
Metaphysis of long bones Distal or proximal tibia, distal femur, proximal or distal fibula, and distal radius |
|
|
|
Subacute OM Treatment |
Surgical approach If small cavity, surgical evacuation and curettage under antibiotic cover
If large cavity, the after evaciaton, packing with cancellous bone chips |
|
|
|
Subacute OM Differentials on imaging |
Sclerotic margin with radiolucent center Osteosarcoma: <1cm Brodie's abscess: >1cm Best visualized by CT scan |
|
|
|
Chronic OM Most common causative organism |
Mixed bacteria In 50% of cases S. Aureus is isolated Have to do biopsy and culture |
|
|
|
Chronic OM Treatment |
Surgery followed by antibiotics for 6 weeks after taking culture |
|
|
|
Septic arthritis Differential diagnosis |
1. Gout (needle like crystals) and pseudogout (rod or rhomboid like crystals), excluded by polarized microscopy 2. Irritable joint (transient synovitis) |
|
|
|
Septic arthritis Adult septic hip is common in |
Heroin injections |
|
|
|
Septic arthritis Joint aspiration |
1. WBCs: >50,000 is diagnostic, >25,000 is suggestive, <25,000 with clumps is suggestive 2. Differential: >90% neutrophils is diagnostic, >85% is suggestive 3. Glucose (decrease) and protein (increase) is suggestive 4. Single bacteria in gram stain is diagnostic 5. Positive culture is pathognomonic |
(similar to CSF analysis) |
|
|
Septic arthritis Treatment |
Drainage and antibiotics <2-years-old: give 3rd gen cephalosporines (ceftriaxone) Augmentin is a good choice for all age groups |
|
|
|
Septic arthritis Complications |
1. Dislocation 2. Tom-Smith dislocation (epiphysial destruction) 3. Growth disturbance 4. Ankylosis (late complication) |
|
|
|
Transient synovitis Definition |
Inflammation of synovium due to a cross reaction with antibodies produced by a remote infection (usually viral) |
|
|
|
Transient Synovitis Kocher criteria |
1. Inability to bear weight (most important one) 2. Fever >38°C 3. WBCs >12K 4. ESR >40, CRP >20
Have 4: 99% septic arthritis, 3: 93%, 2: 40%, 1: 30% |
|
|
|
Septic bursitis (prepatellar or housemaid buritis) Causative agent |
S. Aureus |
|
|
|
Gibbus deformity |
Form of structural kyphosis, where one or more vertebrae become wedged in shape. Can be due to advanced skeletal TB, and cause collapse of vertebral bodies, leadind to cord compression and paraplegia |
|
|
|
Highest bone growth rate |
In lower limb around knee (high blood supply, most common site for bone tumor and infection |
|
|
|
Most common site of cancer metastasis |
Vertebra (valveless veins) |
|
|
|
Septic bursitis Treatment |
Drainage and IV antibiotics |
|
|
|
Metabolic bone disorders |
Depletion of bone tissue 1. Osteoporosis 2. Ostemalacia 3. Osteitis fibrosa |
|
|
|
Measurement of bone mass |
DEXA scan (dual energy x-ray absorptiometry) |
|
|
|
Indications of DEXA scan |
1. Assess degree of bone loss in patients of metabolic bone diseases 2. Screening for perimenopausal women with multiple risk factors for osteoporotic fractures |
|
|
|
Osteoporosis |
Abnormally low bone mass and defects in bone structure, a combination that renders the bone unusually fragile and highr risk of fracturs Bone density decreases with age, so more people become osteoporotic with older age |
|
|
|
Osteoporosis Diagnosis |
DEXA scan is the gold standard for diagnosing osteoporosis, when bone mineral density is less than or equal to 2.5 standard deviations below that of a 30-40-year-old healthy adult woman |
|
|
|
Osteoporosis T-score interpretation |
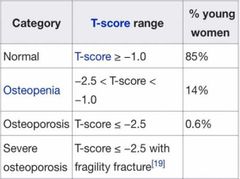
|
|
|
|
Post-menopausal Osteoporosis Definition |
Exagerrated form of physiological bone depletion that normally accompanies aging and loss of gonadal acivity |
|
|
|
Post-menopausal Osteoporosis Pathophysiology |
Withdrawal of estrogen which restraints osteoclastic activity, this increased bone resorption Genetic facrors |
|
|
|
Post-menopausal Osteoporosis Clinical features |
Woman near or at menopause Back pain/ thoracic kyphosis/ fractures (ankle, Colles', femoral neck) Vertebral body compression on X-ray |
|
|
|
Post-menopausal Osteoporosis Prevention |
1. Adequate levels of Ca+ and vit D 2. Walk 30 minutes each day 3. Avoid smoking and excessive alcohol |
|
|
|
Post-menopausal Osteoporosis Treatment |
1. Bisphosphonates (alendronate oral once weekly, or pamidronate IV every 3 months) 2. Ca+ and vit D supplements 3. Treat fractures |
|
|
|
Post-climacteric Osteoporosis Definition |
Same changes as post-menopausal osteoporosis but 15 years later |
|
|
|
Post-climacteric Osteoporosis Causes |
Hormonal depletion: hypogonadism, anti-gonadal hormonal therapy for prostate cancer Other causes: metastatic bone disease, liver disease, alcohol abuse, malabsorption, malnutrition, multiple myeloma, or glucocorticoids |
|
|
|
Post-climacteric Osteoporosis Treatment |
1. Bisphosphonates (alendronate oral once weekly, or pamidronate IV every 3 months) 2. Ca+ and vit D supplements3. Treat fractures |
Same as post-menopausal osteoporosis |
|
|
Secondary Osteoporosis |
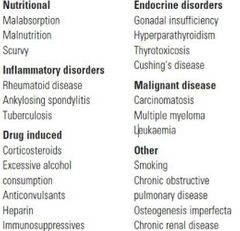
|
|
|
|
Rickets and Osteomalacia Definition |
Different expression of same disease Inadequate mineralization of bone |
|
|
|
Rickets and Osteomalacia Causes (vit. D deficiency causes) |
1. Malnutrition 2. Intestinal malabsorption 3. Under exposure to sunlight 4. Decreased 25-hydroxylation (liver disease or anticonvulsants) 5. Decreased 1-alpha-hydroxylation (nephrectomy, CKD, 1-alpha-hydroxylase deficiency) Other: calcium deficiency, hypophosphatemia |
Defects along metabolic pathway of vitamin D |
|
|
Vitamin D Deficiency Rickets Risk factors |
1. Dietary lack 2. Under-exposure to sunlight |
|
|
|
Vitamin D Deficiency Rickets Clinical Presentation |
1. Tetany and convulsions (in infants) 2. Failure to thrive, muscle flaccidity 3. Early changes (craniotabes, and thickening of knees, ankles, and wrists) 4. Rickety rosary, Harrison's sulcus 6. Distal bowing of tibia (from sitting cross-legged) 7. Lower limb deformities and stunting of growth (once they stand) 8. Severe cases (spinal curvature, coxa vara, and bending/fractures of long bones |
|
|
|
Vitamin D Deficiency Rickets Investigations |
1. Serum calcium and phosphate 2. 25-HCC (deminished) 3. Alkaline phosphatase (increased) 4. Urinary calcium (decreased) |
|
|
|
Vitamin D Deficiency Rickets Treatment |
Vitamin D administration in form of calciferol 400-1000 IU daily with calcium supplements |
|
|
|
Osteomalacia Clinical features |
Insidious, symptoms over years 1. Bone pain 2. Backache 3. Muscle weakness 4. Vit. D deficiency & risk factors |
|
|
|
Osteomalacia X-ray findings |
1. Generalized rarefaction 2. Signs of previous fractures in ribs, vertebrae, pubic rami, or long bones 3. Poorly healing stress fractures (transverse rarefaction in cortex: Looser zone) (Pathognomonic) |
|
|
|
Osteomalacia Investigations |
1. Serum calcium and phosphate (low) 2. Alkaline phospatase (high) 3. Low 25-HCC, 1,25-DHCC (more significant) 4. Biopsy: high amounts of unmineralized osteoid |
|
|
|
Ostemalacia Treatment |
Vitamin D and Calcium Supplements |
|
|
|
Familial Hypophosphatemic Rickets (vit. D resistant rickets) |
Defective bone mineralization but normal serum calcium levels |
|
|
|
Familial Hypophosphatemic Rickets Mode of inheritence |
X-linked dominant |
|
|
|
Familial Hypophosphatemic Rickets Clinical manifestations |
Starts in infancy or soon after Progressive bone deformities: below normal height, and deformities such as genu varum and genu vulgum as soon as they walk No myopathy |
|
|
|
Familial Hypophosphatemic Rickets Investigations and X-ray |
X-ray: vit D deficiency signs but more marked Normal serum calcium levels, but low phosphate |
|
|
|
Familial Hypophosphatemic Rickets Treatment |
1. Large doses vit D (50,000 or more) 2. Inorganic phosphate up to 4g/day (with monitoring to prevent overdose) 3. Bracing or osteotomy (for deformities) Treat continuously until growth ceases |
|
|
|
Post-op OM Most common agent |
S. Epidermidis (it has specail affinity to metals (plates and even patients on dialysis) |
|
|
|
Post-op OM Duration |
If acutely afet surgery, then cause is S. Aureaus If a year after surgery then it is S. Epidermidis |
|
|
|
Post-op OM Treatment |
Only management is removal of plates and metal, bevause S. Epidermidis causes coating and adherence to the metal called biofilm |
|
|
|
Post-op OM Risk after surgery |
7% |
|
|
|
Post-traumatic OM Most common organism |
S. Aureus is most common cause of infection in open fractures |
|
|
|
Gustilo classification of open fractures |
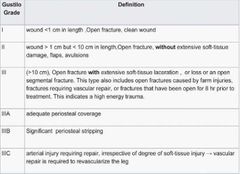
|
|
|
|
Post-traumatic OM Management |
1. Irrigation 2. Splinting and dressing 3. Analgesia and Antibiotics 4. Tetanus prophylaxis |
|
|
|
Post-traumatic OM Management: irrigation |
by normal saline, ringer lactate and glucose saline are contraindicated 3L in type 1, 6L in type 2, 9L in type 3 |
|
|
|
Post-traumatic OM Management: Antibiotics |
Augmentin in class I, II, III Augmentin and Gentamicin in class IIIA, IIIB |
|
|
|
Septic arthritis Most common causative organism and route of infection |
S. Aureus and spread is hematogenous |
|
|
|
Septic Arthritis Most common sites involved |
In pediatrics it is knee In adults it is the hip Most common sites regardless of age is the hip |
|
|
|
Septic arthritis Definition |
Invasion of a joint by an infectious agents, causing joint inflammation and acute synovitis |
|
|
|
Septic arthritis Top Medical Emergency |
Needs operation within 8 hrs, the time needed for cartilage to be destructed by lytic enzymes released from dead neutrophils and macrophages in the pus |
|
|
|
Septic Arthritis Clinical Presentation |
Fever, decreased feeding or activity, no ROM actively, swelling, redness, and hotness at joint |
|
|
|
Septic arthritis Relieving positions |
Hip: flexion, external rotation and slight abduction Knee: flexion Shoulder: adduction |
Hip Knee Shoulder |
|
|
Septic arthritis Invesrigations |
1. X-ray 2. MRI 3. Ultrasound 4. Joint aspiration |
|
|
|
Septic arthritis X-ray |
no early signs late sign is widening of joint space due to swelling, Even later is narrowing of joint space due to destruction of cartilage |
|
|
|
Septic arthritis MRI |
Used to exlude osteomyelitis |
|

