![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
Muscle attachments of supraspinatus
|
Scapula --> greater tuberosity of humerus
|
|
|
Muscle attachments of infraspinatus
|
Scapula --> greater tuberosity of humerus
|
|
|
Muscle attachments of teres minor
|
Scapula --> greater tuberosity of humerus
|
|
|
Muscle attachments of subscapularis
|
Scapula --> Lesser tuberosity of humerus
|
|
|
Nerve supply of supraspinatus
|
Suprascapular nerve
|
|
|
Nerve supply of infraspinatus
|
Suprascapular nerve
|
|
|
Nerve supply of teres minor
|
Axillary nerve
|
|
|
Nerve supply of subscapularis?
|
Subscapular nerve
|
|
|
Muscle function of supraspinatus
|
Abduction
|
|
|
Muscle function of infraspinatus
|
External rotation
|
|
|
Muscle function of teres minor
|
External rotation
|
|
|
Muscle function of subscapularis
|
Internal rotation and adduction
|
|
|
Clinical features of rotator cuff disease
|
Night pain and difficulty sleeping on affected side, pain worse with active motion, weakness and loss of ROM, especially between 90-130 (e.g., trouble with overhead activities), tenderness to palpation over greater tuberosity
|
|
|
Which tests can rule out/differentiate biceps tendinosis from rotator cuff disease?
|
Speed and Yergason's tests; SLAP lesion: O'Brien's test
|
|
|
Describe the Jobe's test for supraspinatus tear
|

Place the shoulder in 90 of abduction and 30 of forward flexion and internally rotate the arm so that the thumb is pointing toward the floor; weakness with active resistance suggests a supraspinatus tear
|
|
|
Describe the Lift-off test
|

Internally rotate arm so dorsal surface of hands rests on lower back. Patient instructed to actively lift hand away from back against examiner resistance; inability to lift hand away from back suggest a subscapularis tear
|
|
|
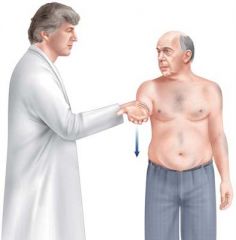
Describe the posterior-cuff test
|
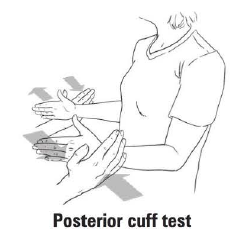
Arm positioned at patient's side in 90 degrees of flexion. Patient instructed to externally rotate arm against the resistance of the examiner; weakness with active resistance suggests posterior cuff tear (infraspinatus and teres minor)
|
|
|
Describe the Neer's test
|

Passive shoulder flexion; pain elicited between 130-170 degrees suggests rotator cuff impingement
|
|
|
Describe the Hawkins-Kennedy test
|

Shoulder flexion to 90 degrees and passive internal rotation; pain with internal rotation suggests rotator cuff impingement
|
|
|
Describe the painful arc test
|
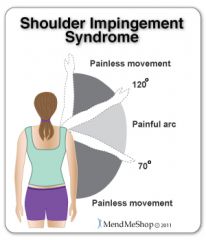
Patient instructed to actively abduct the shoulder; pain with abduction greater than 90 degrees suggests tendinopathy
|
|
|
Investigations for rotator cuff disease
|
X-rays, MRI, and arthrogram (see full thickness tear, difficult to assess partial thickness tear)
|
|
|
X-ray findings in rotator cuff disease
|
AP view may show high riding humerus relative to glenoid, evidence of chronic tendonitis
|
|
|
MRI findings in rotator cuff tear
|
Coronal/sagittal oblique and axial orientations are useful for assessing full/partial thickness tears and tendinopathy +/- arthrogram: geysir sign (injected dye leaks out of joint through the tear)
|
|
|
Treatment of mild rotator cuff disease
|
Non-operative, i.e., physiotherapy and NSAIDs
|
|
|
Treatment of moderate ("tear") rotator cuff disease
|
Non-operative treatment +/- steroid injection
|
|
|
Treatment of severe ("repair") rotator cuff disease
|
Impingement that is refractory to 2-3 months physio and 1-2 injections: may require arthroscopic or surgical repair, i.e., acromioplasty, rotator cuff repair
|
|
|
Ruling out rotator cuff tears
|
98% probability of rotator cuff tear if all 3 of the following are present: supraspinatus weakness, external rotation weakness, and positive impingement signs
|
|
|
Which ligaments attach the clavicle to scapula?
|
AC and CC ligaments
|
|
|
Mechanism of acromioclavicular joint pathology
|
Fall onto shoulder with adducted arm (fall onto tip of shoulder)
|
|
|
Clinical features of AC joint pathology
|
Pain with adduction of shoulder and/or palpation over AC joint; palpate step deformity between distal clavicle and acromion (with dislocation); limited ROM
|
|
|
Investigations for AC joint pathology
|
X-rays: AP, Zanca view (10-15 degree cephalic tilt), axillary +/- stress views (10lb weight in patient's hand)
|
|
|
Non-operative treatment of AC joint pathology
|
Non-operative (most common): sling for 1-3 weeks, ice, and analgesia
|
|
|
Indications for operative treatment of AC joint pathology
|
AC and CC ligaments are both torn and/or clavicle displaced posteriorly
|
|
|
Operative treatment procedure of AC joint pathology
|
Excision of lateral clavicle with AC/CC ligament reconstruction
|
|
|
Incidence of different types of clavicle fractures
|
Proximal - 5%, middle - 80%, or distal third - 15%
|
|
|
In whom are clavicle fractures most common?
|
Children (unites rapidly without complications)
|
|
|
Mechanism of clavicle fracture
|
Fall on shoulder (87%), direct trauma (7%), and FOOSH (6%)
|
|
|
Potential complications of AC joint dislocation
|
Pneumothorax or pulmonary contusion
|
|
|
Clinical features of clavicle fracture
|
Pain and tenting of skin; arm is clasped to chest to splint shoulder and prevent movement
|
|
|
First step in management of clavicle fracture
|
Evaluate neurovascular status of entire upper limb
|
|
|
Treatment of proximal and middle-third clavicle fractures
|
Figure-of-eight sling for 1-2 weeks, early ROM and strengthening once pain subsides, if ends overlap >2cm, consider open reduction and internal fixation (ORIF)
|
|
|
Treatment of distal one-third clavicle fracture
|
Undisplaced (with ligaments intact) - sling for 1-2 weeks, displaced (CC ligament injury) - open reduction and internal fixation (ORIF)
|
|
|
Associated injuries with clavicle fractures?
|
Up to 9% of clavicle fractures are associated with other fractures, most commonly rib fractures. Majority of brachial plexus injuries are associated with proximal third fractures
|
|
|
Specific complications of clavicle fracture
|
Cosmetic bump usually only complication; shoulder stiffness, and weakness with repetitive activity; pneumothorax, brachial plexus injuries and subclavian vessel (all very rare)
|
|
|
What is frozen shoulder (adhesive capsulitis)?
|
Disorder characterized by progressive pain and stiffness of the shoulder usually resolving spontaneously after 18 months
|
|
|
Characteristics of primary adhesive capsulitis?
|
Idiopathic, usually associated with diabetes melitus; may resolve spontaneously in 9-18 months
|
|
|
Causes of secondary adhesive capsulitis
|
Prolonged immobilization, shoulder-hand syndrome, following MIs, stroke, shoulder trauma; poorer outcome
|
|
|
Clinical features of adhesive capsulitis
|
Gradual onset (weeks to months) of diffuse shoulder pain with: 1) decreased active and passive ROM, 2) pain worse at night and often prevents sleeping on affected side, and 3) increased stiffness as pain subsides: continues for 6-12 months after pain has disappeared
|
|
|
Investigations for frozen shoulder (adhesive capsulitis)
|
X-rays may be normal, or may show demineralization from disease
|
|
|
Treatment of frozen shoulder (adhesive capsulitis) (4)
|
Active and passive ROM (physiotherapy), NSAIDs and steroid injections if limited by pain, manipulation under anesthesia and early physiotherapy; arthroscopy for debridement/decompression
|
|
|
Ten conditions associated with an increased incidence of frozen shoulder
|
Prolonged immobilization (most significant), female, age >49, diabetes melitus (5x), cervical disk disease, hyperthyroidism, stroke, MIs, trauma and surgery
|
|
|
When is there a danger of AVN with humerus fractures?
|
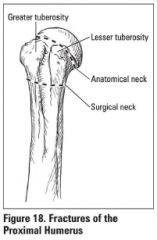
Anatomic neck fractures; disrupt blood supply to the humeral head and AVN may ensue
|
|
|
Mechanism of proximal humeral fracture
|
Young: high energy trauma (MVC); elderly: FOOSH from standing height in osteoporotic individuals
|
|
|
Clinical features of proximal humeral fracture
|
Proximal humeral tenderness,
|
|
|
Specific complications of proximal humeral fracture
|
AVN, axillary nerve palsy, malunion, and post-traumatic arthritis
|

