![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back
|
What causes Neonatal Respiratory Distress Syndrome? |
Surfactant deficiency → ↑ surface tension → alveolar collapse |
|
|
What can predict whether a neonate will have neonatal respiratory distress syndrome? |
Lecithin:Sphingomyelin ratio <1.5 in amniotic fluid |
|
|
What is a potential complication of neonatal respiratory distress syndrome? |
- Persistently low O2 tension → risk of PDA |
|
|
What are the risk factors for neonatal respiratory distress syndrome? |
- Prematurity |
|
|
How do you treat a neonate at risk for neonatal respiratory distress syndrome? |
Give mother steroids before birth to stimulate surfactant production |
|
|
How do you treat an infant with neonatal respiratory distress syndrome? |
Artificial Surfactant |
|
|
What can cause acute respiratory distress syndrome? |
- Trauma |
|
|
What changes occur in acute respiratory distress syndrome? |
- Diffuse alveolar damage → ↑ alveolar capillary permeability → protein-rich leakage into alveoli and non-cardiogenic pulmonary edema (normal PCWP) |
|

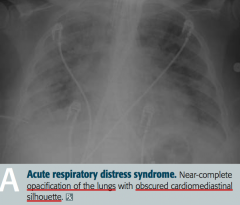
What does this x-ray show? |
Acute Respiratory Distress Syndrome |
|
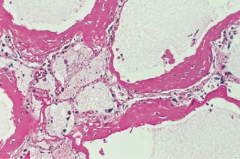
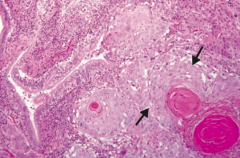
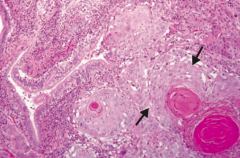
What does this histology show? |
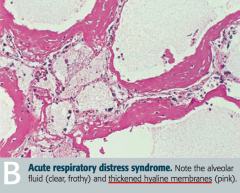
Acute Respiratory Distress Syndrome |
|
|
What causes the initial damage in acute respiratory distress syndrome? |
- Release of neutrophilic substances toxic to alveolar wall |
|
|
What is the normal FEV1/FVC ratio? |
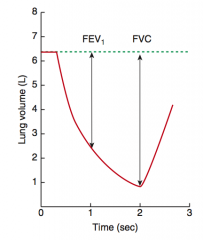
80% |
|
|
What is the FEV1/FVC ratio in obstructive lung disease? |
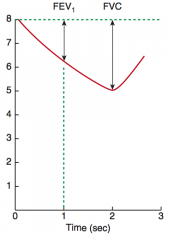
< 80% |
|
|
What is the FEV1/FVC ratio in restrictive lung disease? |
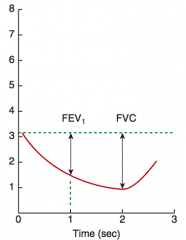
≥ 80% |
|
|
Which lung disease has increased lung volumes (↑ TLC, ↑ FRC, and ↑ RV)? |
Obstructive lung disease |
|
|
Which lung disease has decreased lung volumes (↓ TLC, ↓ FRC, and ↓ RV)? |
Restrictive lung disease |
|
|
How does the change in FEV1 and FVC compare in obstructive vs restrictive lung disease? |
In both obstructive and restrictive disease, FEV1 and FVC are reduced |
|
|
What is the normal pulmonary artery pressure? |
10-14 mmHg |
|
|
What is the definition of pulmonary hypertension? |
≥ 25 mmHg at rest |
|
|
What are the consequences of pulmonary hypertension? |
- Arteriosclerosis |
|
|
What causes Primary Pulmonary Hypertension? Prognosis? |
- Inactivating mutation in BMPR2 gene (normally functions to inhibit vascular smooth muscle proliferation) |
|
|
What causes Secondary Pulmonary Hypertension? Prognosis? |
- COPD |
|
|
How does COPD affect the pressure in the pulmonary circulation? |
Destroys lung parenchyma → 2° pulmonary hypertension |
|
|
Which valvular problem can affect the pressure in the pulmonary circulation? How? |
Mitral Stenosis → ↑ Resistance → ↑ Pressure → 2° pulmonary hypertension |
|
|
How do thromboemboli affect the pressure in the pulmonary circulation? |
Recurrent thromboemboli → ↓ cross-sectional area of pulmonary vascular bed → 2° pulmonary hypertension |
|
|
Which auto-immune diseases affect the pressure in the pulmonary circulation? Implications? |
Systemic Sclerosis |
|
|
What type of cardiac shunt can affect the pressure in the pulmonary circulation? Implications? |
Left-to-Right Shunt → ↑ shear stress → endothelial injury → 2° pulmonary hypertension |
|
|
How does sleep apnea affect the pressure in the pulmonary circulation? |
Hypoxic vasoconstriction → 2° pulmonary hypertension |
|
|
How does living at a high altitude affect the pressure in the pulmonary circulation? |
Hypoxic vasoconstriction → 2° pulmonary hypertension |
|
|
What is the course of having pulmonary hypertension? |
Pulmonary hypertension → severe respiratory distress → cyanosis and RVH → death from decompensated cor pulmonale |
|
|
What happens in sleep apnea? Consequences? |
Repeated cessation of breathing >10 seconds during sleep → disrupts sleep → daytime somnolence |
|
|
What happens to the PaO2 during the day and night in a patient with sleep apnea? |
- Normal PaO2 during day |
|
|
What are the complications of sleep apnea? |
Nocturnal hypoxia → systemic / pulmonary HTN, arrhythmias (atrial fibrillation / flutter), and sudden death |
|
|
What are the types of sleep apnea? How do they differ? |
- Central sleep apnea: no respiratory effort |
|
|
How do you treat sleep apnea? |
- Weight loss |
|
|
How does sleep apnea affect erythropoiesis? |
Hypoxia → ↑ EPO release → ↑ erythropoiesis |
|
|
What variation of sleep apnea is seen in obese patients? |
Obesity Hypoventilation Syndrome: |
|
|
In what lung pathology are there the following findings: |
Pleural Effusion |
|
|
In what lung pathology are there the following findings: |
Atelectasis (bronchial obstruction) |
|
|
In what lung pathology are there the following findings: |
Spontaneous pneumothorax |
|
|
In what lung pathology are there the following findings: |
Tension pneumothorax |
|
|
In what lung pathology are there the following findings: |
Consolidation (lobar pneumonia, pulmonary edema) |
|
|
In what lung pathologies are there decreased breath sounds? |
- Pleural effusion |
|
|
In what lung pathologies are there bronchial breath sounds and late inspiratory crackles? |
Consolidation (lobar pneumonia or pulmonary edema) |
|
|
In what lung pathologies are the lungs dull to percussion? |
- Pleural effusion |
|
|
In what lung pathologies are the lungs hyperresonant to percussion? |
- Spontaneous pneumothorax |
|
|
In what lung pathologies do the lungs have decreased fremitus? |
- Pleural effusion |
|
|
In what lung pathologies do the lungs have increased fremitus? |
Consolidation (lobar pneumonia or pulmonary edema) |
|
|
In what lung pathologies is there a tracheal deviation toward the side of the lesion? |
Atelectasis (bronchial obstruction) |
|
|
In what lung pathologies is there a tracheal deviation away the side of the lesion? |
Tension pneumothorax |
|
|
What is the leading cause of cancer death? |
Lung cancer |
|
|
What is the classic presentation of lung cancer? |
- Cough |
|
|
What finding on x-ray is characteristic of lung cancer? |
Pneumonic "coin" lesion |
|
|
What finding on CT is characteristic of lung cancer? |
Non-calcified nodule |
|
|
What is more common: primary neoplasms or metastases to the lungs? |
In the lung, metastases (usually multiple lesions) are more common than 1° lesions |
|
|
What are the most common sites that metastasize to the lungs? |
Cancer of: |
|
|
What are the most common sites of metastases from the lungs? |
- Adrenals |
|
|
What are the types of lung cancer? |
- Adenocarcinoma |
|
|
What types of lung cancer are located peripherally? |
- Adenocarcinoma |
|
|
What types of lung cancer are located centrally? |
- Squamous cell carcinoma |
|
|
What is the most common type of lung cancer (except for metastases)? |
Adenocarcinoma |
|
|
What is the most common type of lung cancer in non-smokers? |
Adenocarcinoma |
|
|
What genetic changes are associated with Lung Adenocarcinoma? |
Activating mutations: |
|
|
What is a specific physical sign of Lung Adenocarcinoma? |
Hypertrophic osteoarthropathy (clubbing) |
|
|
Which subtype of lung adenocarcinoma is associated with hazy infiltrates on CXR (similar to pneumonia)? Why this appearance? Prognosis? |
Bronchioloalveolar Subtype of Adenocarcinoma: |
|
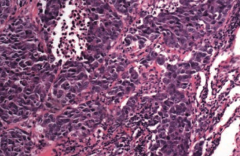
What type of cancer does this show? What are the characteristics of it that tell you that? |
Squamous Cell Carcinoma |
|
|
What is the location of lung Squamous Cell Carcinoma? Other characteristics indicative of it? |
- Central location |
|
|
What type of lung cancer is associated with hypercalcemia? How? |
Squamous Cell Carcinoma |
|
What type of cancer does this show? What are the characteristics of it that tell you that? |
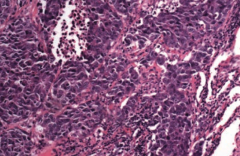
Small Cell (Oat Cell) Carcinoma |
|
|
What type of lung cancer is known for producing certain substances that can cause seemingly unrelated symptoms? What substances? |
Small Cell (Oat Cell) Carcinoma: |
|
|
What genetic change is sometimes associated with Small Cell (Oat Cell) Carcinoma? |
Ampification of myc oncogenes common |
|
|
What is the prognosis of Small Cell (Oat Cell) Carcinoma? How do you treat it? |
- Undifferentiated → very aggressive |
|
|
Which type of lung cancer is associated with pleomorphic giant cells? |
Large Cell Carcinoma |
|
|
What are the characteristics of a Large Cell Carcinoma of the lung? Location? |
- Peripheral locatoin |
|
|
What is the prognosis for Large Cell Carcinoma? How do you treat? |
- Poor prognosis |
|
|
What type of lung cancer is composed of nests of neuroendocrine cells and is chromogranin A positive? |
Bronchial Carcinoid Tumor |
|
|
What is the prognosis for Bronchial Carcinoid Tumor? Symptoms? |
- Excellent prognosis, metastasis rare |
|
|
What type of lung cancer is associated with Carcinoid Syndrome? What does that mean? |
Bronchial Carcinoid Tumor |
|
|
Which types of lung cancer have a good prognosis? |
- Bronchioalveolar subtype of Adenocarcinoma |
|
|
What is the name of the malignancy of the pleura? What is it associated with? |
Mesothelioma |
|
|
What are the complications of a Mesothelioma? |
Results in hemorrhagic pleural effusion and pleural thickening |
|
|
What are the histologic signs of Mesothelioma? |
Psamomma bodies |

