![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
133 Cards in this Set
- Front
- Back
|
What diagnosis should you consider in a patient presenting with unilateral flank tenderness, colicky pain radiating to groin, and hematuria? Treatment/Prevention?
|
Kidney Stones
- Treat and prevent by encouraging fluid intake |
|
|
What are the potential complications of kidney stones?
|
- Hydronephrosis
- Pyelonephritis |
|
|
What are the types of kidney stones based on content? How common?
|
- Calcium (80%)
- Ammonium magnesium phosphate (15%) - Uric acid (5%) - Cystine (1%) |
|
|
What kind of kidney stones precipitate with ↑ pH?
|
- Calcium phosphate
- Ammonium magnesium phosphate |
|
|
What kind of kidney stones precipitate with ↓ pH?
|
- Calcium oxalate
- Uric acid - Cystine |
|
|
What kind of kidney stones appear radiopaque on x-ray?
|
- Calcium phosphate and calcium oxalate
- Ammonium magnesium phosphate - Cystine |
|
|
What kind of kidney stones appear radiolucent on x-ray?
|
Uric Acid (think radiol"U"cent for "U"ric acid)
|
|

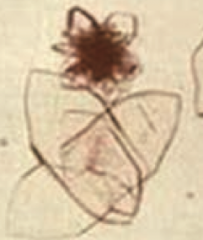
If your patient presents with unilateral flank tenderness, colicky pain radiating to groin, and hematuria, and the following urine crystals are identified, what should you diagnose?
|

Calcium kidney stones
- This is the "envelope" type of calcium urine crystal - There is also a dumbbell shaped urine crystal |
|

If your patient presents with unilateral flank tenderness, colicky pain radiating to groin, and hematuria, and the following urine crystals are identified, what should you diagnose?
|

Ammonium magnesium phosphate kidney stones
- This is the "coffin lid" type of urine crystal |
|
If your patient presents with unilateral flank tenderness, colicky pain radiating to groin, and hematuria, and the following urine crystals are identified, what should you diagnose?
|

Uric Acid kidney stones
- Rhomboid or rosettes appearing urine crystals |
|
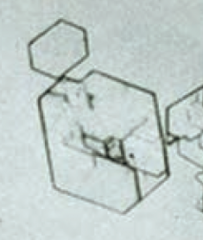
If your patient presents with unilateral flank tenderness, colicky pain radiating to groin, and hematuria, and the following urine crystals are identified, what should you diagnose?
|
Cystine kidney stones
- Hexagonal appearing urine crystals |
|
|
What is the most common kidney stone presentation?
|
Calcium oxalate stone in a patient with hypercalciuria and normalcalcemia
|
|
|
Calcium kidney stones can be composed of what? What promotes their formation?
|
- Content: calcium oxalate, calcium phosphate, or both
- Promoted by hypercalciuria: idiopathic or 2° to conditions that cause hypercalcemia such as cancer or ↑ PTH) |
|
|
What can cause calcium oxalate crystals to form?
|
- Ethylene glycol (anti-freeze)
- Vitamin C abuse - Crohn disease |
|
|
How do you treat patients with recurrent calcium kidney stones?
|
- Thiazide diuretics
- Citrate |
|
|
What type of renal pathology is also known as "struvite"?
|
Ammonium Magnesium Phosphate kidney stones
|
|
|
What causes Ammonium Magnesium Phosphate kidney stones / Struvite?
|
Infection with urease (+) bugs:
- Proteus mirabilis - Staphylococcus - Klebsiella These bugs hydrolyze urea to ammonia → urine alkalinization |
|
|
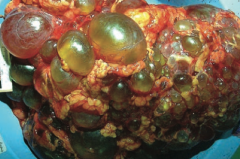
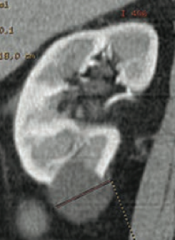
What are potential complications of Ammonium Magnesium Phosphate kidney stones / Struvite?
|

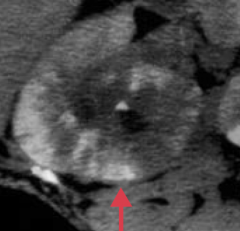
Staghorn calculi (picture) → can be a nidus for UTIs
|
|
|
How do you treat Ammonium Magnesium Phosphate kidney stones / Struvite?
|
- Eradicate underlying infection (Proteus mirabilis, Staphylococcus, or Klebsiella)
- Surgical removal of stone |
|
|
What type of kidney stone is likely to form in a patient with ↓ urine volume, acidic pH, and arid climate?
|
Uric Acid
|
|
|
How can you identify a Uric Acid kidney stone?
|
- Visible on CT and Ultrasound, but not on x-ray (radiolucent)
- Strongly associated with hyperuricemia (eg, gout) |
|
|
What are Uric Acid kidney stones associated with?
|
- Hyperuricemia (eg, Gout)
- Diseaes with ↑ cell turnover, such as leukemia |
|
|
How do you treat patients with Uric Acid kidney stones?
|
Alkalinization of urine
|
|
|
Who is more likely to get Cystine kidney stones? What is the most common cause?
|
- Mostly seen in children
- Secondary to cystinuria |
|
|
How can you diagnose a patient with having Cystine kidney stones?
|
- Sodium nitroprusside test is positive
- Look at crystals (hexagonal) |
|
|
What are the potential complications of Cystine kidney stones?
|

Can form staghorn calculi
|
|
|
How do you treat a patient with Cystine kidney stones?
|
- Alkalinization of urine
- Hydration |
|
|
What is the term for the distention / dilation of the renal pelvis and calyces?
|
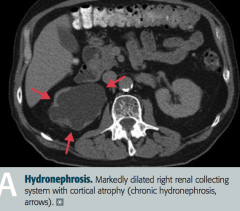
Hydronephrosis
|
|
|
What are the most common causes of Hydronephrosis?
|
- Urinary tract obstruction: eg, renal stones, BPH, cervical cancer, injury to ureter
- Retroperitoneal fibrosis - Vesicoureteral reflux |
|
|
What findings occur in Hydronephrosis? Complications?
|
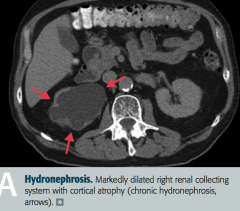
- Distention / dilation of renal pelvis and calyces proximal to site of pathology
- Only impairs renal function if bilateral or patient only has one kidney - Leads to compression atrophy of renal cortex and medulla |
|
|
What is the most common primary renal malignancy? Origin?
|
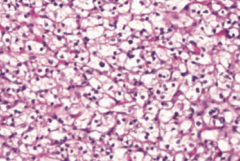
Renal Cell Carcinoma
- Originates from proximal tubule cells → polygonal clear cells (picture) filled with lipids and carbohydrates |
|
|
In whom is Renal Cell Carcinoma most common?
|
- Most common in men 50-70 years old
- ↑ incidence in patients who smoke and are obese |
|
|
What diagnosis should you consider in a patient with hematuria, a palpable mass, 2° polycythemia, flank pain, fever, and weight loss?
|

Renal Cell Carcinoma
|
|
|
What are the most common locations for Renal Cell Carcinoma to spread to? Significance?
|
- Invades renal vein then IVC to spread hematogenously
- Metastasizes to lung and bone - "Silent" cancer because it commonly presents as a metastatic neoplasm |
|
|
What genetic change is associated with Renal Cell Carcinoma?
|
Gene deletion on chromosome 3 (sporadic or inherited as von Hippel-Lindau syndrome)
RCC = 3 letters = chromosome 3 |
|
|
What is Renal Cell Carcinoma associated with?
|
Paraneoplastic syndromes:
- Ectopic EPO - Ectopic ACTH - Ectopic PTHrP |
|
|
How do you treat Renal Cell Carcinoma?
|
- Resection if localized disease
- Immunotherapy or targeted therapy for advanced / metastatic disease - Resistant to chemotherapy and radiation therapy |
|
|
What is the typical presentation of Renal Cell Carcinoma?
|
- Commonly silent because it often only presents once it has metastasized
- Hematuria - Palpable mass - 2° polycythemia - Flank pain - Fever - Weight loss |
|
Which type of renal tumor presents as a well-circumscribed mass with a central scar? Benign or malignant? Source?
|
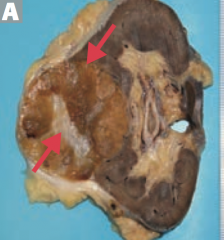
Renal oncocytoma
- Benign epithelial cell tumor |
|
|
What is the histologic appearance of a Renal Oncocytoma?
|
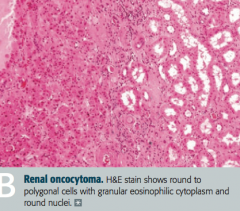
Large eosinophilic cells with abundant mitochondria without perinuclear clearing
|
|
|
What diagnosois should you consider in a patient who presents with painless hematuria, flank pain, and an abdominal mass? How should you treat?
|
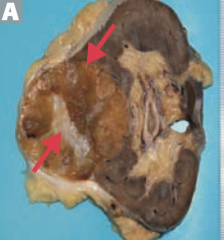
Renal Oncocytoma
- Treat with nephrectomy |
|
|
What is the most common renal malignancy of early childhood (ages 2-4)?
|
Wilms Tumor (Nephroblastoma)
|
|
|
What kind of structures are in a Wilms Tumor (Nephroblastoma)?
|
Embryonic glomerular structures
|
|
|
What is the typical presentation of a Wilms Tumor (Nephroblastoma)?
|
- Child aged 2-4
- Huge, palpable flank mass - Hematuria |
|
|
What genetic change is associated with Wilms Tumor (Nephroblastoma)?
|
Loss of function mutations of tumor suppressor genes WT1 and WT2 on chromosome 11
|
|
|
If your patient with a Wilms tumor also has Aniridia (absence or iris), a genitourinary malformation, and mental retardation / intellectual disability, what diagnosis should you consider?
|
Beckwith-Wiedemann Syndrome or WAGR complex:
- Wilms tumor - Aniridia - Genitourinary malformation - mental Retardation (intellectual disability) |
|
|
What are the findings in the Beckwith-Wiedemann Syndrome?
|
WAGR complex:
- Wilms tumor - Aniridia - Genitourinary malformation - mental Retardation (intellectual disability) |
|
|
What is the most common tumor of the urinary tract system? Where can it occur specifically?
|
Transitional Cell Carcinoma
- Renal calyces - Renal pelvis - Ureters - Bladder |
|
|
A patient presents with painless hematuria without casts, what is the most likely diagnosis?
|
Bladder cancer (Transitional Cell Carcinoma)
|
|
|
What are the associated exposures in patients with Transitional Cell Carcinoma?
|
Problems in your Pee SAC:
- Phenacetin (pain-relieving and fever-reducing drug, banned in 80s) - Smoking - Aniline dyes - Cyclophosphamide |
|
|
What is the histologic appearance of Transitional Cell Carcinoma?
|
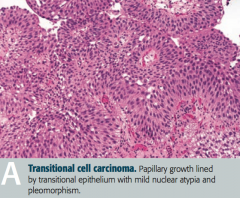
Papillary growth lined by transitional epithelium with mild nuclear atypica and pleomorphism
|
|
|
What types of cancer can occur in the bladder?
|
- Transitional cell carcinoma
- Squamous cell carcinoma of the bladder |
|
|
What causes squamous cell carcinoma of the bladder?
|
Chronic irritation of urinary bladder → squamous metaplasia → dysplasia and squamous cell carcinoma
|
|
|
What are the risk factors for squamous cell carcinoma of the bladder?
|
- Schistosoma haematobium infection (Middle East)
- Chronic cystitis - Smoking - Chronic nephrolithiasis |
|
|
If your patient from the Middle East presents with painless hematuria what diagnosis / cause should you consider?
|
Schistosoma haemotobium infection → chronic irritation of urinary bladder → squamous metaplasia → dysplasia and Squamous Cell Carcinoma of bladder
|
|
|
What diagnosis should you consider in a patient presenting with suprapubic pain, dysuria, urinary frequency, and urgency?
|
Acute infectious cystitis (bladder infection)
|
|
|
What are the risk factors for acute infectious cystitis?
|
- Female gender (short urethra)
- Sexual intercourse ("honeymoon cystitis") - Indwelling catheters |
|
|
What are the most common causes of acute infectious cystitis?
|
- E. coli (most common)
- Staphylococcus saprophyticus (sexually active young women - although E. coli still more common) - Klebsiella - Proteus mirabilis (urine has ammonia scent) - Adenovirus (hemorrhagic cystitis) |
|
|
What are the most common causes of acute infectious cystitis in young sexually active women?
|
- E. coli (most common)
- Staphylococcus saprophyticus |
|
|
Which cause of acute infectious cystitis is associated with an ammonia scent to the urine?
|
Proteus mirabilis
|
|
|
What infection causes hemorrhagic cystitis?
|
Adenovirus
|
|
|
What are the typical lab findings in acute infectious cystitis?
|
- Leukocyte esterase (+)
- Nitrites appear for G- organisms (especially E. coli) - Sterile pyruia with (-) urine cultures suggests urethritis (N. gonorrhoeae or Chlamydia trachomatis) |
|
|
What diagnosis should you consider in a patient with sterile pyuria and negative urine cultures?
|
Urethritis by Neisseria gonorrhoeae or Chlamydia trachomatis
|
|
|
What diagnosis should you consider in a patient presenting with dysuria, fever, costovertebral angle tenderness, nausea, and vomiting?
|
Acute Pyelonephritis
|
|
|
What are the most common causes of Acute Pyelonephritis?
|
- Ascending UTI (E. coli most common)
- Vesicoureteral reflux - Hematogenous spread of infection to kidney |
|
|
What lab / imaging findings are associated with Acute Pyelonephritis?
|
- White cell casts in urine
- CT: striated parenchymal enhancement |
|
|
What are the risk factors for Acute Pyelonephritis?
|
- Indwelling urinary catheter
- Urinary tract obstruction - Diabetes mellitus (sugar in urine = food for infection) - Pregnancy |
|
|
What are the possible complications of Acute Pyelonephritis?
|
- Chronic pyelonephritis
- Renal papillary necrosis - Perinephric abscess |
|
|
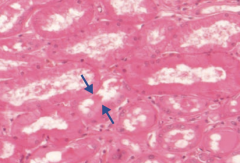
What is the histologic appearance of Acute Pyelonephritis?
|
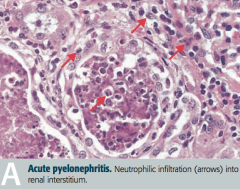
Neutrophilic infiltration (arrows) into renal interstitium
|
|
|
How do you treat Acute Pyelonephritis?
|
Antibiotics appropriate for cause
|
|
|
What is the cause of Chronic Pyelonephritis?
|
- Recurrent episodes of acute pyelonephritis
- Typically requires predisposition to infection such as vesicoureteral reflux or chronically obstructing kidney stones |
|
|
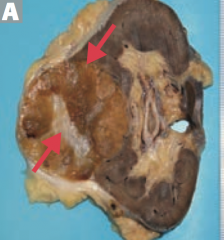
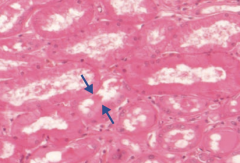
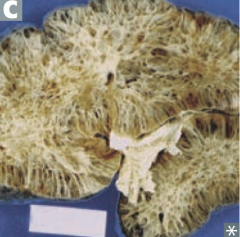
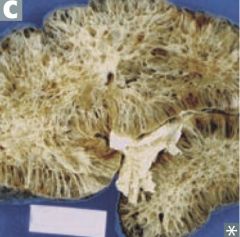
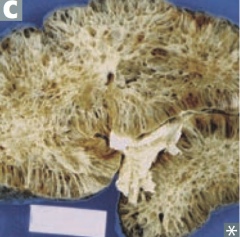
What is the histologic appearance of Chronic Pyelonephritis?
|
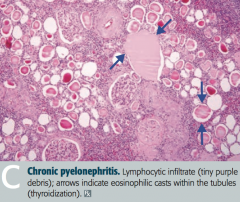
- Coarse, asymmetric corticomedullary scarring
- Blunted calyx - Tubules can contain eosinophilic casts that resemble thyroid tissue (thyroidization of kidney) = picture |
|
|
In what renal pathology is there "thyroidization of the kidney"?
|
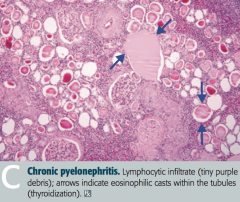
Chronic Pyelonephritis
- Tubules can contain eosinophilic casts that resemble thyroid tissue |
|
|
What diagnosis should you consider in a patient with fever, rash, hematuria, and costovertebral angle tenderness in a patient who has been taking a new drug for 1-2 weeks? What drugs are most likely to cause this?
|
Drug-Induced Interstitial Nephritis (Tubulointerstitial Nephritis)
- Diuretics - Penicillin derivatives - Sulfonamides - Rifampin - Can occur months after taking NSAIDs |
|
|
What changes occur in Drug-Induced Interstitial Nephritis (Tubulointerstitial Nephritis)?
|
- Acute interstitial renal inflammation
- Pyuria (classically eosinophils) - Azotemia (abnormally high levels of nitrogen-containing compounds in blood) |
|
|
How do drugs cause Drug-Induced Interstitial Nephritis (Tubulointerstitial Nephritis)?
|
Drugs act as "haptens" (elicit an immune response only when attached to a large carrier such as a protein), inducing hypersensitivity
|
|
|
What renal pathology is associated with obstetric catastrophes (eg, abruptio placentae)? Cause?
|
Diffuse Cortical Necrosis
- Acute generalized cortical infarction of both kidneys - Likely due to a combination of vasospasm and DIC |
|
|
What renal pathology is associated with septic shock? Cause?
|
Diffuse Cortical Necrosis
- Acute generalized cortical infarction of both kidneys - Likely due to a combination of vasospasm and DIC |
|
|
What causes Diffuse Cortical Necrosis?
|
- Acute generalized cortical infarction of both kidneys
- Likely due to a combination of vasospasm and DIC - Associated with obstetric catastrophes (eg, abruptio placentae) and septic shock |
|
|
What is the most common cause of intrinsic renal failure?
|
Acute Tubular Necrosis
|
|
|
What is the prognosis for Acute Tubular Necrosis?
|
- Self-reversible in some cases
- Can be fatal if left untreated - Death most often occurs during the initial "oliguric" phase |
|
|
What is the key identifying feature of Acute Tubular Necrosis?
|
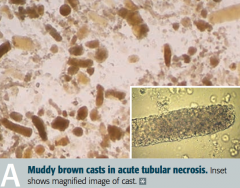
Granular "muddy brown" casts
|
|
|
What are the three stages of Acute Tubular Necrosis?
|
1. Inciting event
2. Maintenance phase - oliguric (small production of urine) 3. Recovery phase - polyuric (increased production of dilute urine) |
|
|
What is the first stage of Acute Tubular Necrosis?
|
Inciting event
- Ischemic injury - Nephrotoxic injury |
|
|
What is the second stage of Acute Tubular Necrosis, after the inciting event? Length? Characteristics?
|
Maintenance phase
- Oliguria (production of a small amount of urine) - Lasts 1-3 weeks - Risk of hyperkalemia and metabolic acidosis |
|
|
What is the third stage of Acute Tubular Necrosis, after the maintenance phase / oliguria? Characteristics?
|
Recovery phase
- Polyuria (production of large amounts of dilute urine) - BUN and serum creatinine fall - Risk of hypokalemia |
|
|
What can cause Acute Tubular Necrosis?
|
- Ischemic injury
- Nephrotoxic injury |
|
|
What can be responsible for an ischemic injury leading to Acute Tubular Necrosis? What does this lead to?
|
- 2° to ↓ renal blood flow (eg, hypotension, shock, sepsis, hemorrhage, CHF)
- Results in death of tubular cells that may slough into tubular lumen (proximal tubule and thick ascending limb are highly susceptible to injury) |
|
|
Which parts of the kidney are particularly susceptible to injury by ischemia?
|
- Proximal tubule
- Thick ascending limb of loop of Henle |
|
|
What can be responsible for a nephrotoxic injury leading to Acute Tubular Necrosis? What does this lead to?
|
- 2° to injury resulting from toxic substances (eg, aminoglycosides, radiocontrast agents, lead, cisplatin)
- Or 2° to crush injury (myoglobinuria) or hemoglobinuria - Proximal tubule is particularly susceptible to injury |
|
|
Which toxic substances can cause a nephrotoxic injury leading to Acute Tubular Necrosis?
|
- Aminoglycosides
- Radiocontrast agents - Lead - Cisplatin |
|
|
Which part of the kidney is particularly susceptible to nephrotoxic injury?
|
Proximal Tubule
|
|
|
What can cause gross hematuria and proteinuria?
|
Renal Papillary Necrosis
- Sloughing of renal papillae - May be triggered by a recent infection or immune stimulus |
|
|
What is Renal Papillary Necrosis associated with?
|
- Diabetes Mellitus
- Acute pyelonephritis - Chronic phenacetin use (acetaminophen is a phenacetin derivative) - Sickle cell anemia and trait |
|
|
What is the definition of Acute Kidney Injury (acute renal failure)?
|
- Abrupt decline in renal function
- ↑ Creatinine and ↑ BUN - Occurs over a period of several days |
|
|
What happens to BUN and creatinine in a normal nephron? Why?
|
- BUN is reabsorbed for countercurrent multiplication
- Creatinine is not reabsorbed |
|
|
What are the forms of acute kidney injury / acute renal failure?
|
- Pre-renal Azotemia
- Intrinsic Renal Failure - Post-renal Azotemia |
|
|
What happens to the kidney in Pre-Renal Azotemia? Why?
|
- ↓ GFR due to ↓ RBF (eg, hypotension)
- Na+, H2O, and urea are retained by the kidney in an attempt to conserve volume - ↑ BUN/creatinine ratio |
|
|
What happens to the kidney in Intrinsic Renal Failure? Why?
|
- Generally due to acute tubular necrosis or ischemia / toxins
- Less commonly due to acute glomerulonephritis (eg, RPGN) - Patchy necrosis leads to debris obstructing tubule and fluid backflow across necrotic tubule → ↓ GFR - Urine has epithelial / granular casts - BUN reabsorption is impaired → ↓ BUN/creatinine ratio |
|
|
What happens to the kidney in Post-Renal Azotemia? Why?
|
- Due to outflow obstruction (eg, stones, BPH, neoplasia, congenital anomalies)
- Develops only with bilateral obstruction |
|
|
Which type of acute kidney injury causes:
- Urine osmolality: >500 mOsm/kg - Urine Na+: <20 mEq/L - FENa: <1% (fractional Na+ excretion) - Serum BUN/Cr ratio: >20 Causes? |
Pre-Renal Azotemia
- As a result of ↓ RBF, eg, hypotension |
|
|
Which type of acute kidney injury causes:
- Urine osmolality: <350 mOsm/kg - Urine Na+: >40 mEq/L - FENa: >2% (fractional Na+ excretion) - Serum BUN/Cr ratio: <15 Causes? |
Intrinsic Renal Failure
- Generally due to acute tubular necrosis or ischemia/toxins - Less commonly due to glomerulonephritis (eg, RPGN) |
|
|
Which type of acute kidney injury causes:
- Urine osmolality: <350 mOsm/kg - Urine Na+: >40 mEq/L - FENa: >1% if mild, >2% if severe (fractional Na+ excretion) - Serum BUN/Cr ratio: >15 Causes? |
Post-Renal Azotemia
- Due to outflow obstruction (eg, stones, BPH, neoplasia, congenital anomalies |
|
|
What is the urine osmolality in Pre-Renal Azotemia vs Intrinsic Renal Failure vs Post-Renal Azotemia?
|
- Pre-Renal Azotemia: >500
- Intrinsic Renal Failure: <350 - Post-Renal Azotemia: <350 (in mOsm/kg) |
|
|
What is the urine Na+ in Pre-Renal Azotemia vs Intrinsic Renal Failure vs Post-Renal Azotemia?
|
- Pre-Renal Azotemia: <20
- Intrinsic Renal Failure: >40 - Post-Renal Azotemia: >40 (in mEq/L) |
|
|
What is the FENa (fractional sodium excretion) in Pre-Renal Azotemia vs Intrinsic Renal Failure vs Post-Renal Azotemia?
|
- Pre-Renal Azotemia: <1%
- Intrinsic Renal Failure: >2% - Post-Renal Azotemia: >1% (mild), >2% (severe) |
|
|
What is the serum BUN/creatinine ratio in Pre-Renal Azotemia vs Intrinsic Renal Failure vs Post-Renal Azotemia?
|
- Pre-Renal Azotemia: >20
- Intrinsic Renal Failure: <15 - Post-Renal Azotemia: >15 |
|
|
What are the consequences of renal failure?
|
MAD HUNGER:
- Metabolic Acidosis - Dyslipidemia (esp. ↑ TGs) - Hyperkalemia - Uremia - Na+/H2O retention - Growth retardation and developmental delay - Erythropoietin failure (anemia) - Renal osteodystrophy |
|
|
What are the two forms of renal failure? Causes?
|
- Acute: pre-renal azotemia, acute tubular necrosis, post-renal azotemia
- Chronic: hypertension, diabetes, congenital anomalies |
|
|
What is there an inability to do in renal failure?
|
Inability to:
- Make urine - Excrete nitrogenous wastes |
|
|
What acid/base disturbance is associated with renal failure?
|
Metabolic Acidosis
MAd hunger |
|
|
What lipid disturbance is associated with renal failure?
|
Dyslipidemia: especially ↑ TGs
maD hunger |
|
|
What electrolyte disturbance is associated with renal failure?
|
- Hyperkalemia
- Uremia - Na+/H2O retention mad HUNger |
|
|
What disturbances are there in children with with renal failure?
|
Growth retardation and developmental delay
mad hunGer |
|
|
What blood disturbance is associated with renal failure?
|
anemia due to Erythropoietin failure
(and platelet dysfunction due to uremia) mad hungEr |
|
|
What bone disturbance is associated with renal failure?
|
Renal osteodystrophy - causes subperiosteal thinning of bones
mad hungeR |
|
|
What are the characteristics of Uremia in renal failure?
|
↑ BUN and ↑ Creatinine, leads to:
- Nausea and anorexia - Pericarditis - Asterixis - Encephalopathy - Platelet dysfunction |
|
|
What causes renal osteodystrophy?
|
- Failure of vitamin D hydroxylation → ↓ 1,25-(OH)2-Vitamin D → ↓ intestinal Ca2+ absorption
- Hypocalcemia - Hyperphosphatemia also independently ↓ serum Ca2+ by causing tissue calcifications |
|
|
What happens in renal osteodystrophy due to the failure of vitamin D hydroxylation, hypocalcemia, and hyperphosphatemia?
|
- Subperiosteal thinning of bones
- 2° Hyperparathyroidism |
|
|
What are the types of renal cyst disorders?
|
- Autosomal Dominant Polycystic Kidney Disease (ADPKD)
- Autosomal Recessive Polycystic Kidney Disease (ARPKD) - Medullary Cystic Disease - Simple vs Complex Renal Cysts |
|
|
Which type of renal cyst disorder occurs more often in adults? Appearance of kidneys?
|
Autosomal Dominant Polycystic Kidney Disease (ADPKD)
- Innumerable cysts - Bilateral enlarged kidneys - Destroys kidney parenchyma |
|
|
What are the symptoms of a patient with Autosomal Dominant Polycystic Kidney Disease (ADPKD)?
|
- Flank pain
- Hematuria - Hypertension - Urinary infection - Progressive renal failure |
|
|
What is the cause of Autosomal Dominant Polycystic Kidney Disease (ADPKD)?
|
- 85% of cases: mutation in PKD1 on chromosome 16
- 15% of cases: mutation in PKD2 on chromosome 4 Autosomal dominant inheritance |
|
|
What are the complications and prognosis in patients with Autosomal Dominant Polycystic Kidney Disease (ADPKD)?
|
- Death from complications of chronic kidney disease or hypertension (caused by ↑ renin production)
- Associated with Berry aneurysms, mitral valve prolapse, and benign hepatic cysts |
|
|
Which type of renal cyst disorder occurs more often in infants? Appearance of kidneys?
|
Autosomal Recessive Polycystic Kidney Disease (ARPKD)
- Cysts in parenchyma |
|
|
What is Autosomal Recessive Polycystic Kidney Disease (ARPKD) associated with?
|
- Congenital hepatic fibrosis
- Potter sequence (if significant renal failure in utero) - Beyond neonatal period: hypertension, portal hypertension, progressive renal insufficiency |
|
|
What is the appearance of the kidneys in Medullary Cystic Disease?
|
- Medullary cysts usually not visualized
- Kidneys appear shrunken on ultrasound |
|
|
What damage occurs in Medullary Cystic Disease? Prognosis?
|
- Tubulointerstitial fibrosis
- Progressive renal insufficiency - Inability to concentrate urine - Poor prognosis |
|
|
What diagnosis should you consider in a patient with difficulty concentrating urine and shrunken kidneys on ultrasound?
|
Medullary Cystic Disease
|
|
|
What is responsible for the majority of all renal masses? Location?
|
Simple Renal Cysts - found in outer cortex
|
|
|
What are the findings of simple renal cysts?
|
- Found in outer cortex
- Filled with ultrafiltrate - Found incidentally and typically asymptomatic |
|
|
What kind of renal cyst increases the risk of renal cell carcinoma?
|
Complex Renal Cysts
|
|
|
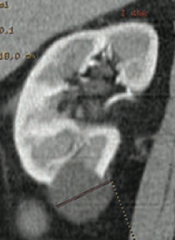
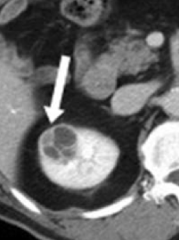
What is the appearance of Complex Renal Cysts? How should they be treated?
|
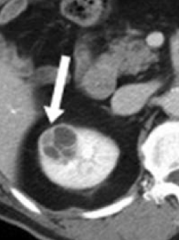
- Can be septated, enhanced, or have solid components, as seen on CT
- Require follow-up or removal due to risk of renal cell carcinoma |

