![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
|
What is the term for the obstruction of sinus drainage into the nasal cavity, leading to inflammation and pain over the affected area? What is the most likely affected area? |
Rhinosinusitis |
|
|
What happens in Rhinosinusitis? What is the most common cause? |
- Obstruction of sinus drainage into the nasal cavity, leading to inflammation and pain over the affected area (usually maxillary sinuses in adults) |
|
|
What is the most common acute cause of rhinosinusitis? |
Viral URI |
|
|
What are the most common causes of superimposed bacterial infection on rhinosinusitis? |
- S. pneumoniae |
|
|
What predisposes to a deep venous thrombosis? |
Virchow's Triad: |
|
|
What can cause hypercoagulability? What is this a component of? |
- Eg, defect in coagulation cascade proteins, most commonly Factor V Leiden |
|
|
What are the characteristics of endothelial damage that is a component of Virchow's triad? |
Exposed collagen triggers clotting cascade |
|
|
What is the most likely location for pulmonary emboli to arise from? |
Deep leg veins |
|
|
What is the Homan sign? |
Dorsiflexion of the foot → calf pain |
|
|
What drug can be used to prevent deep vein thrombosis? |
Heparin |
|
|
What drug can be used for acute management of deep vein thrombosis? |
Heparin |
|
|
What drug can be used for long-term prevention of deep vein thrombosis recurrence? |
Warfarin |
|
|
What are the signs / symptoms of Pulmonary Embolism? |
- V/Q mismatch → hypoxemia → respiratory alkalosis |
|
|
What are the types of Pulmonary Emboli? |
"An embolus moves like a FAT BAT" |
|
|
What are fat pulmonary emboli associated with? |
Associated with long bone fractures and liposuction |
|
|
What is the classic triad of fat emboli? |
- Hypoxemia |
|
|
What can an amniotic fluid emboli lead to? |
Can lead to DIC, especially post-partum |
|
|
Who is likely to get gas emboli? How do you treat them? |
Nitrogen bubbles can precipitate in ascending divers; treat with hyperbaric oxygen |
|
|
What is the best way to image a patient you think has a pulmonary embolism? What do you look for? |

CT pulmonary angiography (look for filling defects) |
|
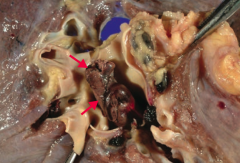
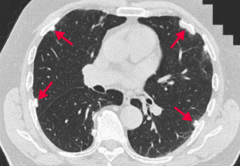
What is this gross image of? |
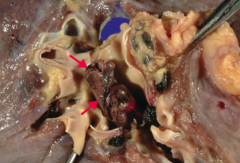
Pulmonary Embolism |
|
What does this image show? |
Pulmonary Thromboembolus |
|
|
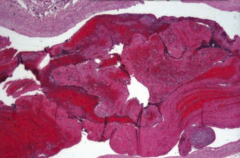
What can you look for to determine whether a thrombus formed pre-mortem or post-mortem? |
Lines of Zahn are interdigitating areas of pink (platelets, fibrin) and red (RBCs) found only in thrombi formed BEFORE death |
|
|
What are the consequences of obstructive lung diseases? |
- Leads to air trapping in the lungs |
|
|
What can chronic, hypoxic pulmonary vasoconstriction lead to? |
Cor Pulmonale |
|
|
What are the types of obstructive lung diseases? |
- Chronic Bronchitis ("blue bloater") |
|
|
What happens to the pulmonary function tests in patients with obstructive lung disease? |
- ↓↓ FEV1 |
|
|
What are the types of COPD? |
- Chronic Bronchitis |
|
|
What happens pathologically in patients with Chronic Bronchitis? |
Hyperplasia of mucus-secreting glands in the bronchi → Reid index >50% |
|
|
What is the Reid Index? Utility? |
Ratio of thickness of gland layer / total thickness of bronchial wall |
|
|
What are the diagnostic criteria for Chronic Bronchitis? |
Productive cough for >3 months / year (not necessarily consecutive) for >2 years |
|
|
Chronic bronchitis is a disease of what airways? |
Small airways |
|
|
What signs and symptoms does a patient with Chronic Bronchitis have? |
- Wheezing |
|
|
What happens pathologically in patients with Emphysema? |
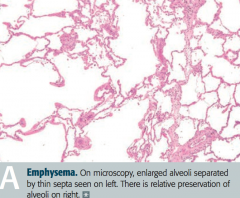
- Enlargement of air spaces |
|
|
What are the types of emphysema? What is each associated with? |
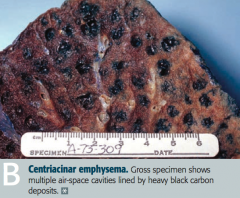
- Centriacinar: associated with smoking |
|
|
What causes increased lung compliance in patients with emphysema? |
↑ Elastase activity → loss of elastic fibers → ↑ lung compliance |
|
|
How do patients with emphysema breathe? |
Exhale through pursed lips to increase airway pressure and prevent airway collapse during respiration |
|
|
What is the pathology responsible for asthma? |
Bronchial hyperresponsiveness causes reversible bronchoconstriction |
|
|
What are the histologic findings of asthma? |
- Smooth muscle hypertrophy |
|
|
What is the term for shed epithelium that forms mucus plugs? What pathology is it a sign of? |
Curschman Spirals - sign of asthma |
|
|
What is the term for the crystals formed by the breakdown of eosinophils in the sputum? What pathology is it a sign of? |
Charcot-Leyden crystals - sign of asthma |
|
|
What can trigger asthma? |
- Viral URIs |
|
|
What test can you use to diagnose asthma? |
Methacholine challenge |
|
|
What are the findings of asthma? |
- Cough |
|
|
What pathology is seen in Bronchiectasis? |
Chronic necrotizing infection of bronchi → permanently dilated airways, purulent sputum, recurrent infections, and hemoptysis |
|
|
What part of the respiratory tract is affected by bronchiectasis? How is it affected? |
Bronchi: chronic necrotizing infection |
|
|
What is bronchiectasis associated with? |
- Bronchial obstruction |
|
|
What are the characteristics of all restrictive lung diseases? |
Restricted lung expansion causes: |
|
|
What are the types of restrictive lung disease? |
- Restrictive lung disease due to poor breathing mechanics |
|
|
What are the characteristics of restrictive lung diseases due to poor breathing mechanics? Causes? |
- Extrapulmonary, peripheral hypoventilation, normal A-a gradient |
|
|
What are the characteristics of interstitial lung diseases? |
- Pulmonary ↓ diffusing capacity |
|
|
What are the types of interstitial lung diseases? |
- Acute Respiratory Distress Syndrome (ARDS) |
|
|
What histologic finding is characteristic of neonatal respiratory distress syndrome? |
Hyaline membrane (disease) |
|
|
What are the findings in Sarcoidosis that affects the lungs? |
Restrictive lung disease |
|
|
What are the characteristics of idiopathic pulmonary fibrosis? |
Restrictive lung disease |
|
|
What kind of granulomas occur in Langerhans Cell Histiocytosis? |
Eosinophilic Granulomas |
|
|
What drugs can cause restrictive lung disease? |
- Bleomycin |
|
|
What type of reaction causes hypersensitivity pneumonitis? |
Mixed type III/IV hypersensitivity reaction to environmental antigens |
|
|
Which symptoms occur in hypersensitivity pneumonitis? |
- Dyspnea |
|
|
Who is most likely to get hypersensitivity pneumonitis? |
- Farmers |
|
|
What are the types of pneumoconioses? |
- Asbestosis |
|
|
What do Coal Workers' Pneumoconiosis, Silicosis, and Asbestosis increase the risk for? |
- Cor pulmonale |
|
|
What is Caplan Syndrome? |
Rheumatoid Arthritis and Pneumonconioses with Intrapulmonary Nodules |
|
|
What lung pathology is associated with shipbuilding, roofing, and plumbing? |
Asbestosis |
|
|
What are the characteristic findings on imaging of asbestosis? |

"Ivory white" calcified pleural plaques are pathognomonic of asbestos exposure, but they are not precancerous |
|
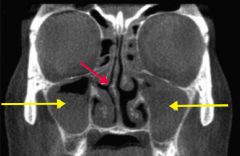
What are these findings associated with? |

Asbestosis: |
|
|
What part of the lungs are affected by asbestosis? |
Affects lower lungs: |
|
|
What is the appearance of asbestos histologically? |
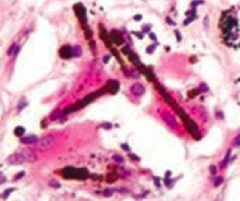
Asbestos (ferruginous) bodies are golden-brown fusiform rods resembling dumbbells |
|
|
What part of the lungs are affected by silicosis? |
Affects upper lobes: |
|
|
What part of the lungs are affected by coal? |
Affects upper lobes: |
|
|
What is the other name for "black lung disease"? |
Coal Workers' Pneumoconiosis |
|
|
What happens if someone has prolonged exposure to coal dust? |
Macrophages become laden with carbon → inflammation and fibrosis → Coal Workers' Pneumoconiosis |
|
|
What condition is found in many urban dwellers exposed to sooty air? Symptoms? |
Anthracosis - asymptomatic |
|
|
What is associated with foundries, sandblasting, and mines? |
Silicosis |
|
|
What happens if someone has exposure to silica? |
- Macrophages respond to silica and release fibrogenic factors → fibrosis → Silicosis |
|
|
What is there increased risk of in patients with Silicosis? |
- Increased susceptibility to TB |
|
|
What is the characteristic appearance of silicosis? |
"Eggshell" calcification of hilar lymph nodes |

