![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
35 Cards in this Set
- Front
- Back
|
What are the potential complications of ulcers?
|
- Hemorrhage
- Perforation |
|
|
Which ulcer complication is more common in gastric ulcers?
|
Hemorrhage
|
|
|
Which ulcer complication is more common in duodenal ulcers?
|
- Perforation (anterior > posterior) |
|
|
If a patient with a gastric ulcer hemorrhages, what is the most likely source of the bleed?
|
Most likely from lesser curvature → bleeding from L gastric artery
|
|
|
If a patient with a duodenal ulcer hemorrhages, what is the most likely source of the bleed?
|
Most likely from posterior wall of duodenum → bleeding from gastroduodenal artery
|
|
|
Perforation as a consequence of a duodenal ulcer is most likely to occur where? Symptoms?
|
- Anterior wall > Posterior wall
- May see free air under diaphragm on CXR - Referred pain to shoulder |
|
What does this CXR show?
|
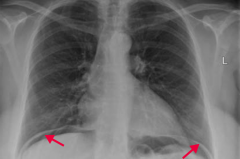
Perforation of duodenal ulcer (anterior wall > posterior wall)
- Leads to free air under the diaphragm - May cause referred pain to shoulder |
|
|
What are the potential consequences of malabsorption syndromes?
|
- Diarrhea
- Steatorrhea - Weight loss - Weakness - Vitamin and mineral deficiencies |
|
|
If your patient presents with diarrhea, steattorhea, weight loss, weakness, and vitamin/mineral deficiencies, what should you consider?
|
Malabsorption Syndromes: "These Will Cause Devastating Absorption Problems"
- Tropical sprue - Whipple disease - Celiac sprue - Disaccharidase deficiency - Abetalipoproteinemia - Pancreatic insufficiency |
|
|
Which malabsorption syndrome should you consider in a patient who recently visited the tropics? Cause? How should they be treated?
|
Tropical Sprue
- Similar to celiac sprue (affects small bowel) - Responds to antibiotics (cause is unknown) |
|
|
Which malabsorption syndrome should you consider in an older man who also presents with cardiac symptoms, arthralgias, and neurologic symptoms? Cause? Other?
|
Whipple Disease
- Infection with Tropheryma whipplei (G+, PAS stain + for foamy macrophages in intestinal lamina propria and mesenteric nodes) *Foamy Whipped cream in a CAN: cardiac sx, arthralgias, neuro sx) |
|
|
Which malabsorption syndrome should you consider in a patient of northern European descent? Cause? How should they be treated?
|
Celiac sprue
- Autoimmune-mediated intolerance of gliadin (wheat) → malabsorption and steatorrhea - Associated with HLA-DQ2 and HLA-DQ8 - Treat with gluten-free diet |
|
|
Which malabsorption syndrome should you consider in a patient intolerant of milk? Symptoms?
|
Disaccharidase deficiency (lactase)
- Osmotic diarrhea - May be self-limited follow an acute injury (eg, viral diarrhea) |
|
|
Which malabsorption syndrome should you consider in a young child with failure to thrive, steatorrhea, acanthocytosis, ataxia, and night blindness? Cause?
|
Abetalipoproteinemia
- ↓ Synthesis of apolipoprotein B → inability to generate chylomicrons → ↓ secretion of cholesterol, VLDL into bloodstream → fat accumulation in enterocytes |
|
|
Which malabsorption syndrome should you consider in a patient with cystic fibrosis?
|
Pancreatic insufficiency
- Causes malabsorption of fat and fat-soluble vitamins (A, D, E, and K) |
|
|
Which malabsorption syndrome should you consider in a patient with obstructing cancer?
|
Pancreatic insufficiency
- Causes malabsorption of fat and fat-soluble vitamins (A, D, E, and K) |
|
|
Which malabsorption syndrome should you consider in a patient with chronic pancreatitis?
|
Pancreatic insufficiency
- Causes malabsorption of fat and fat-soluble vitamins (A, D, E, and K) |
|
|
What are the signs/symptoms of malabsorption syndromes?
|
- Diarrhea
- Steatorrhea - Weight loss - Weakness - Vitamin and mineral deficiencies |
|
|
What are the characteristics of Tropical Sprue?
|
Malabsorption syndrome
- Similar findings as celiac sprue (affects small bowel) - Responds to antibiotics - Cause is unknown, but seen in residents of or recent visitors to tropics |
|
|
What are the characteristics of Whipple disease?
|
Malabsorption syndrome |
|
|
What are the characteristics of Celiac Sprue?
|
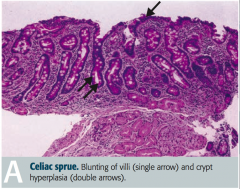
Malabsorption syndrome:
- Auto-immune mediated intolerance of gliadin (wheat) → malabsorption and steatorrhea - Associated with HLA-DQ2, HLA-DQ8, and northern European descent - Antibodies: anti-endomysial, anti-tissue transglutaminase, and anti-gliadin antibodies - Blunting of villi and lymphocytes in lamina propria (picture) - ↓ Mucosal absorption, primarily affects distal duodenum and/or proximal jejunum - Diagnosis: serum levels of tissue transglutaminase antibodies - Associated with dermatitis herpetiformis - Moderately ↑ risk of malignancy (eg, T-cell lymphoma) - Treat: gluten-free diet |
|
|
What are the characteristics of Disaccharidase Deficiency?
|
Malabsorption syndrome:
- Most common is lactase deficiency → milk intolerance - Normal-appearing villi - Osmotic diarrhea - Since lactase is located at tips of intestinal villi, self-limited lactase deficiency can occur following injury (eg, viral diarrhea) - Diagnosis: lactose tolerance test (+) if administration of lactose produces symptoms and glucose rises <20 mg/dL |
|
|
What are the characteristics of abetalipoproteinemia?
|
Malabsorption Syndrome: |
|
|
What are the characteristics of Pancreatic Insufficiency?
|
Malabsorption Syndrome
- Due to cystic fibrosis, obstructing cancer, and chronic pancreatitis - Causes malabsorption of fat and fat-soluble vitamins (A, D, E, and K) - ↑ Neutral fat in stool - Diagnosis: D-xylose absorption test - normal urinary excretion in pancreatic insufficiency; ↓ excretion with intestinal mucosa defects or bacterial overgrowth |
|
|
Which type of malabsorption syndrome is caused by infection?
|
- Tropical Sprue (treat with antibiotics) - cause is unknown
- Whipple Disease - infection with Tropheryma whipplei (G+) - Self-limited lactase deficiency - following viral diarrhea |
|
|
Which type of malabsorption syndrome is characterized by foamy macrophages?
|
Whipple Disease
|
|
|
What is Celiac Sprue associated with?
|
- HLA-DQ2, HLA-DQ8
- Northern European descent - Dermatitis Herpetiformis (watery blisters, not caused by herpes) - Increased risk of malignancy (eg, T-cell lymphoma) |
|
|
What antibodies cause Celiac Sprue?
|
- Anti-endomysial antibody
- Anti-tissue transglutaminase antibody - Anti-gliadin antibody |
|
|
What are the histologic findings in Celiac Sprue?
|
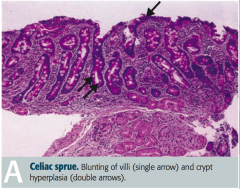
- Blunting of villi
- Lymphocytes in lamina propria |
|
|
Which part of the GI tract has malabsorption in Celiac Sprue?
|
Decreased mucosal absorption primarily affects distal duodenum and / or proximal jejunum
|
|
|
How do you diagnose Celiac Disease?
|
Presence of tissue transglutaminase antibodies in serum |
|
|
What kind of diarrhea occurs in disaccharidase deficiency (eg, lactase deficiency)? |
Osmotic diarrhea (too much water is drawn into the bowels)
|
|
|
How do you diagnose a disacharidase deficiency (eg, lactase deficiency)?
|
Lactose Tolerance Test is (+) for lactase deficiency, if: |
|
|
What are the implications of a decreased ability to synthesize apolipoprotein B?
|
Inability to generate chylomicrons → ↓ secretion of cholesterol, VLDL into bloodstream → fat accumulates in enterocytes
Abetalipoproteinemia (type of malabsorption disorder) |
|
|
How do you diagnose pancreatic insufficiency (malabsorption syndrome)?
|
D-xylose absorption test:
- Normal urinary excretion in pancreatic insufficiency - ↓ excretion with intestinal mucosa defects or bacterial overgrowth |

