![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back
|
Who is most likely to get colorectal cancer? |
- Most patients >50 years
- 25% have a family history |
|
|
What genetic syndromes can contribute to Colorectal Cancer?
|
- Familial Adenomatous Polyposis (FAP)
- Gardner Syndrome - Turcot Syndrome - Hereditary Non-Polyposis Colorectal Cancer (HNPCC / Lynch Syndrome) |
|
|
How are the different genetic syndromes that can cause Colorectal Cancer inherited?
|
All Autosomal Dominant
|
|
|
What mutation is responsible for Familial Adenomatous Polyposis (FAP)? Location?
|
Autosomal Dominant mutation of APC gene on chromosome 5q |
|
|
If you have 2 hits of the mutated APC gene on chromosome 5q, what do you have? What will it cause?
|
Familial Adenomatous Polyposis (FAP) |
|
|
What are the signs of Familial Adenomatous Polyposis (FAP)? |
- Thousands of polyps arise starting at a young age |
|
|
What is it called if you have Familial Adenomatous Polyposis (FAP) + osseous and soft tissue tumors, with congenital hypertrophy of retinal pigment epithelium?
|
Gardner Syndrome
|
|
|
What is it called if you have Familial Adenomatous Polyposis (FAP) + a malignant CNS tumor?
|
Turcot Syndrome (think TURban)
|
|
|
What mutation is responsible for Hereditary Non-Polyposis Colorectal Cancer (HNPCC / Lynch Syndrome)?
|
Autosomal dominant mutation of DNA mismatch repair genes
|
|
|
If you have a mutation of DNA mismatch repair genes, what do you have? What will it cause?
|
Hereditary Non-Polyposis Colorectal Cancer (HNPCC / Lynch Syndrome) |
|
|
Which part of the colon is affected by Hereditary Non-Polyposis Colorectal Cancer (HNPCC / Lynch Syndrome)?
|
Proximal colon is ALWAYS involved |
|
|
What mutations cause a predisposition for colorectal cancer?
|
- Mutation of APC gene on chromosome 5q → Familial Adenomatous Polyposis (FAP) → 100% progress to CRC
- Mutation of DNA mismatch repair genes → Hereditary Non-Polyposis Colorectal Cancer (HNPCC / Lynch Syndrome) → 80% progress to CRC |
|
|
What is Gardner Syndrome?
|
Familial Adenomatous Polyposis (FAP) + osseous and soft tissue tumors, congenital hypertrophy of retinal pigment epithelium
|
|
|
What is Turcot Syndrome?
|
Familial Adenomatous Polyposis (FAP) + malignant CNS tumor (TURcot = TURban)
|
|
|
What are the risk factors for Colorectal Cancer?
|
- Inflammatory Bowel Disease
- Tobacco use - Large villous adenomas (polyps) - Juvenile polyposis syndrome - Peutz-Jeghers Syndrome (hamatromatous polyps) |
|
|
What part of the colon is most commonly affected by Colorectal Cancer?
|
Rectosigmoid > Ascending > Descending
|
|
|
What are the characteristics of Colorectal Cancer in the ascending colon?
|
- Exophytic mass
- Iron deficiency anemia - Weight loss RIGHT SIDE BLEEDS, left side obstructs |
|
|
What are the characteristics of Colorectal Cancer in the descending colon?
|
- Infiltrating mass
- Partial obstruction - Colicky pain - Hematochezia Right side bleeds, LEFT SIDE OBSTRUCTS |
|
|
What is a rare presentation of Colorectal Cancer? |
Streptococcus bovis bacteremia
- S. bovis colonizes the gut - Can also cause subacute endocarditis Bovis in the Blood = Cancer in the Colon |
|
|
If you have a patient with iron deficiency anemia who is male or postmenopausal female, what must you rule out? |
Colorectal Cancer
|
|
|
How should patients be screened for Colorectal Cancer?
|
- Screen patients >50 years old |
|
|
What finding occurs in Colorectal Cancer on barium enema x-ray?
|

"Apple core" lesion
|
|

Your patient gets a barium enema x-ray, and this is the finding in the sigmoid colon, what do you think of?
|

Apple core lesion → think Colorectal Cancer
|
|
|
What tumor marker is good for monitoring recurrence of Colorectal Cancer? Can it be used for screening?
|
CEA tumor marker can be used to monitor for recurrence, but not useful for screening
|
|
|
What are the two molecular pathways that lead to Colorectal Cancer? How common?
|
- Microsatellite instability pathway (~15%)
- APC / β-catenin (chromosomal instability) pathway (~85%) |
|
|
What is wrong in the microsatellite instability pathway? What does it cause?
|
- DNA mismatch repair gene mutations → sporadic and HNPCC syndrome
- Mutations accumulate, but no defined morphologic correlates - Responsible for 15% of cases of CRC |
|
|
What is wrong in the APC/β-catenin pathway? What does it cause? |

- Chromosomal instability → sporadic cancer
- Responsible for 85% of cases of CRC - Normal colon → loss of APC gene → - Colon at risk → K-ras mutation → - Adenoma → Loss of tumor suppressor gene(s) (p53, DCC) → - Carcinoma |
|
|
What gene events occur in the APC/β-catenin pathway leading to colorectal cancer
|

Order of gene events: AK-53
- Normal colon → loss of APC gene (↓ intercellular adhesion and ↑ proliferation) → - Colon at risk → K-ras mutation (unregulated intracellular signal transduction) → - Adenoma → Loss of tumor suppressor gene(s) (p53, DCC) (increased tumorigenesis) → - Carcinoma |
|
|
What are the implications of the loss of the APC gene in the progression to colorectal cancer?
|

- Decreased intercellular adhesions
- Increased proliferations - Colon at risk |
|
|
What are the implications of the K-RAS mutation after loss of the APC gene in the progression to colorectal cancer?
|
- Unregulated intracellular signal transduction
- At risk colon → Adenoma |
|
|
What are the implications of the loss of tumor suppressor genes (p53, DCC), after the K-RAS mutation and loss of the APC gene in the progression to colorectal cancer?
|
- Increased tumorigenesis
- Adenoma → Carcinoma |
|
|
What are the signs of portal hypertension?
|
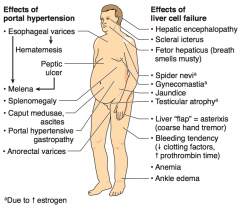
- Esophageal varices → hematemesis and melena
- Peptic ulcer → melena - Splenomegaly - Caput medusae, ascites - Portal hypertensive gastropathy - Anorectal varices |
|
|
What are the signs of liver cell failure?
|
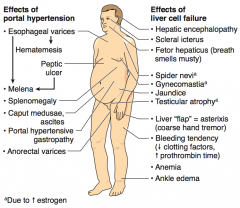
- Hepatic encephalopathy
- Scleral icterus - Fetor hepaticus (breath smells musty) - Spider nevi (d/t ↑ Estrogen) - Gynecomastia (d/t ↑ Estrogen) - Jaundice - Testicular atrophy (d/t ↑ Estrogen) - Liver "flap" = asterixis (coarse hand tremor) - Bleeding tendency (↓ clotting factors, ↑ prothrombin time) - Anemia - Ankle edema |
|
What is the term for the diffuse fibrosis and nodular regeneration that destroys the normal architecture of the liver? |
Cirrhosis
|
|
|
What are the characteristics of cirrhosis?
|
- Diffuse fibrosis
- Nodular regeneration - Destroys normal architecture of liver |
|
|
What does cirrhosis put you at risk for?
|
Increased risk for Hepatocellular Carcinoma (HCC)
|
|
|
What are the most common causes of cirrhosis?
|
- Alcohol (60-70%)
- Viral hepatitis - Biliary disease - Hemochromatosis |
|
|
What can alleviate portal hypertensino?
|
Portosystemic shunts:
- Esophageal varices - Caput medusae |
|
|
What are these signs indicative of?
- Esophageal varices - Hematemesis - Peptic ulcer - Melena - Splenomegaly - Caput medusae, ascites - Portal gastropathy - Anorectal varices |
Portal Hypertension
|
|
|
What are these signs indicative of? |
Liver cell failure
|
|
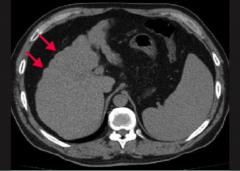
What does this CT show?
|
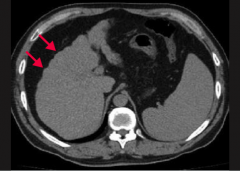
Nodularity (arrows) of the liver contour secondary to regenerating macronodules = Cirrhosis
|
|
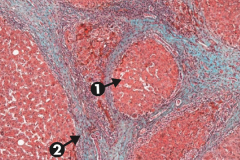
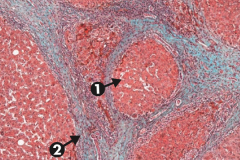
What does this slide show?
|
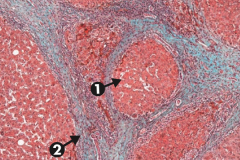
Cirrhosis, microscopic: typical regenerative nodules (arrow 1) and bridging fibrosis (arrow 2)
|
|
|
What are the serum markers of liver and pancreas pathology?
|
- Alkaline phosphatase (ALP)
- Aminotransferases (AST and ALT) - often called liver enzymes - Ceruloplasmin - γ-Glutamyl Transpeptidase (GGT) - Amylase - Lipase |
|
|
What is the major diagnostic use of Alkaline Phosphatase (ALP)?
|
- Obstructive hepatobiliary disease
- HCC - Bone disease |
|
|
What is the major diagnostic use of Aminotransferases (AST and ALT) - often called "liver enzymes"?
|
- Viral hepatitis (ALT > AST)
- Alcoholic hepatitis (AST > ALT) |
|
|
What is the major diagnostic use of Ceruloplasmin?
|
↓ in Wilson Disease
|
|
|
What is the major diagnostic use of γ-Glutamyl Transpeptidase (GGT)?
|
↑ in various liver and biliary diseases (just as ALP can), but not in bone disease; associated with alcohol use
|
|
|
What is the major diagnostic use of Amylase? |
- Acute pancreatitis |
|
|
What is the major diagnostic use of Lipase?
|
Acute Pancreatitis (most specific)
|
|
|
Which serum marker is most specific to acute pancreatitis?
|
Lipase
|
|
|
What can develop in children to take aspirin?
|
Reye Syndrome - rare, often fatal childhood hepatoencephalopathy
|
|
|
What are these findings associated with:
- Hepatoencephalopathy - Mitochondrial abnormalities - Fatty liver (microvesicular fatty change) - Hypoglycemia - Vomiting - Hepatomegaly - Coma Cause? |
Reye Syndrome - associated with viral infection (especially VZV and influenza B) that has been treated with aspirin |
|
|
What is the mechanism by which aspirin causes Reye Syndrome?
|
Aspirin metabolites ↓ β-oxidation by reversible inhibition of mitochondrial enzyme
|
|
|
What are the signs of Reye Syndrome?
|
- Hepatoencephalopathy (often fatal)
- Mitochondrial abnormalities - Fatty liver (microvesicular fatty change) - Hypoglycemia - Vomiting - Hepatomegaly - Coma |
|
|
What is the only exception for use of aspirin in children?
|
Kawasaki disease
|
|
|
What are the stages of alcoholic liver disease?
|
- Hepatic steatosis |

