![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
|
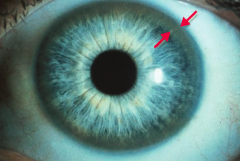
What is the mnemonic to remember the characteristics of Wilson Disease (hepatolenticular degeneration)? |
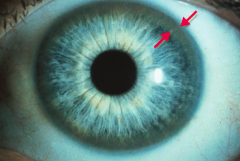
Copper is Hella BAD:
- C: ↓ Ceruloplasmin, Cirrhosis, Corneal deposits (Kayser-Fleischer rings), Copper accumulations, Carcinoma (hepatocellular) - H: Hemolytic anemia - B: Basal ganglia degeneration (parkinsonian symptoms) - A: Asterixis (tremor of the hand when the wrist is extended) - D: Dementia, Dyskinesia, Dysarthria |
|
|
What causes Wilson Disease?
|
Inadequate hepatic copper excretion and failure of copper to enter circulation as ceruloplasmin
|
|
|
What are the implications of inadequate hepatic copper excretion and failure of copper to enter circulation as ceruloplasmin? Where does it go?
|
Wilson Disease
- Leads to copper accumulation - Especially in liver, brain, cornea (Kayser-Fleischer ring), kidneys, and joints |
|
|
How do you treat Wilson Disease?
|
Penicillamine or Trientine
|
|
|
How do you get Wilson disease?
|
Autosomal recessive inheritance (chromsome 13 = 13 letters in Wilson disease)
- Copper is normally excreted into bile by hepatocyte copper transporting ATPase (ATP-7B gene) |
|
|
What is the mnemonic to remember the characteristics of Wilson Disease (hepatolenticular degeneration)?
|
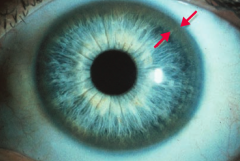
Copper is Hella BAD:
- C: ↓ Ceruloplasmin, Cirrhosis, Corneal deposits (Kayser-Fleischer rings), Copper accumulations, Carcinoma (hepatocellular) - H: Hemolytic anemia - B: Basal ganglia degeneration (parkinsonian symptoms) - A: Asterixis (tremor of the hand when the wrist is extended) - D: Dementia, Dyskinesia, Dysarthria |
|
|
What disease should you consider in a patient who is very tan with Diabetes Mellitus ("bronze Diabetes")? Cause?
|
Hemochromatosis
- Disease caused by deposition of hemosiderin (iron) |
|
|
What is the classic triad in Hemochromatosis?
|
- Micronodular Cirrhosis
- Diabetes mellitus - Skin pegmentation |
|
|
What are the potential consequences of Hemochromatosis?
|
- CHF
- Testicular atrophy - ↑ Risk of HCC |
|
|
What can cause Hemochromatosis?
|
- 1° - autosomal recessive C282Y or H63D mutation on HFE gene, associated with HLA-A3
- 2° - chronic transfusion therapy (eg, β-thalassemia major) |
|
|
What are the lab results in a patient with Hemochromatosis?
|
- ↑ Ferritin |
|
|
What mutation is responsible for hereditary hemochromatosis? What is it associated with?
|
- C282Y or H63D mutation on HFE gene (autosomal recessive)
- Associated with HLA-A3 |
|
|
Is hemochromatosis worse in young men or young women? Why?
|
Young men - in women, iron can be lost through menstruation which slows the progression
|
|
|
How do you treat hereditary hemochromatosis?
|
- Repeated phlebotomy
- Deferasirox - Deferoxamine |
|
|
What are the types of biliary tract diseases?
|
- Primary Biliary Cirrhosis
- Secondary Biliary Cirrhosis - Primary Sclerosing Cholangitis |
|
|
How do Primary Biliary Cirrhosis, Secondary Biliary Cirrhosis, and Primary Sclerosing Cholangitis present?
|
Same presentation
- Pruritus - Jaundice - Dark urine - Light stools - Hepatosplenomegaly |
|
|
What is the pathologic cause of Primary Biliary Cirrhosis (PBC)?
|
- Auto-immune reaction →
- Lymphocytic infiltrate + Granulomas → - Destruction of intralobular bile ducts |
|
|
What is the pathologic cause of Secondary Biliary Cirrhosis (SBC)?
|
- Extrahepatic biliary obstruction (gallstone, biliary stricture, chronic pancreatitis, carcinoma of pancreatic head) →
- ↑ Pressure in intrahepatic ducts → - Injury / fibrosis and bile stasis |
|
|
What is the pathologic cause of Primary Sclerosing Cholangitis (PSC)?
|
- Unknown cause of concentric "onion skin" bile duct fibrosis →
- Alternating strictures and dilation with "beading" of intra- and extra-hepatic bile ducts on ERCP |
|
|
Which biliary tract disease is complicated by ascending cholangitis?
|
Secondary Biliary Cirrhosis
|
|
|
Which biliary tract disease has ↑ serum mitochondrial antibodies, including IgM?
|
Primary Biliary Cirrhosis
|
|
|
Which biliary tract disease is associated with other auto-immune conditions? Which ones?
|
Primary Biliary Cirrhosis is associated with:
- CREST syndrome - Sjögren syndrome - Rheumatoid arthritis - Celiac disease |
|
|
Which biliary tract disease has hypergammaglobulinemia (IgM)?
|
Primary Sclerosing Cholangitis
|
|
|
Which biliary tract disease is associated with Ulcerative Colitis?
|
Primary Sclerosing Cholangitis
|
|
|
What can Primary Sclerosing Cholangitis progress to?
|
- 2° biliary cirrhosis |
|
|
Which biliary tract disease is associated with extrahepatic biliary obstruction (eg, gallstone, biliary stricture, chronic pancreatitis, or carcinoma of pancreatic head)? Presentation? Labs? Additional information?
|
Secondary Biliary Cirrhosis
- Presentation: pruritus, jaundice, dark urine, light stools, hepatosplenomegaly - Labs: ↑ conjugated bilirubin, ↑ cholesterol, ↑ ALP - Additional: ↑ pressure in intrahepatic ducts → injury/fibrosis and bile stasis; complicated by ascending cholangitis |
|
|
Which biliary tract disease is associated with an auto-immune reaction, leading to a lymphocytic infiltrate and granulomas? Presentation? Labs? Additional information?
|
Primary Biliary Cirrhosis
- Presentation: pruritus, jaundice, dark urine, light stools, hepatosplenomegaly - Labs: ↑ conjugated bilirubin, ↑ cholesterol, ↑ ALP - Additional: destruction of intralobular bile ducts; ↑ serum mitochondrial antibodies, including IgM; associated with other auto-immune conditions (eg, CREST, Sjögren syndrome, rheumatoid arthritis, and celiac disease) |
|
|
Which biliary tract disease is associated with "onion skin" bile duct fibrosis? Presentation? Labs? Additional information?
|
Primary Sclerosing Cholangitis
- Presentation: pruritus, jaundice, dark urine, light stools, hepatosplenomegaly - Labs: ↑ conjugated bilirubin, ↑ cholesterol, ↑ ALP - Additional: alternating strictures and dilation with "beading" of intra- and extra-hepatic bile ducts on ERCP; hypergammaglobulinemia (IgM); associated with ulcerative colitis; can lead to 2° biliary cirrhosis and cholangiocarcinoma |
|
|
What is the term for the presence of gallstones?
|
Cholelithiasis
|
|
|
What is Cholelithiasis? What can cause them?
|
Gallstones:
- ↑ cholesterol and/or bilirubin - ↓ bile salts - Gallbladder stasis |
|
|
What are the types of gallstones?
|
- Cholesterol stones (80%)
- Pigment stones |
|
|
What increases your risk for gallstones?
|
4 F's: |
|
|
What is associated with developing cholesterol stones?
|
- Obesity
- Crohn Disease - Advanced age - Clofibrate - Estrogen therapy - Multiparity - Rapid weight loss - Native American origin |
|
|
What is associated with developing pigment stones?
|
- Patients with chronic hemolysis
- Alcoholic cirrhosis - Advanced age - Biliary infection |
|
|
What is the appearance of cholesterol stones?
|
Radiolucent w/ 10-20% opaque due to calcifications
|
|
|
What is the appearance of pigment stones?
|
- Black: radiopaque, hemolysis
- Brown: radiolucent, infection |
|
|
What can gallstones cause?
|
- Cholecystitis (inflammation of gallbladder)
- Ascending cholangitis (infection of bile duct) - Acute pancreatitis - Bile stasis - Biliary colic - Fistula between gallbladder and small intestine - Gallstone ileus |
|
|
What is the term for neurohormonal activation (by CCK after a fatty meal) that triggers contraction of the gallbladder, forcing a stone into the cystic duct, which may present with pain (eg, in diabetics)?
|
Biliary Colic
|
|
|
What is Biliary Colic?
|
- Neurohormonal activation (by CCK after a fatty meal)
- Triggers contraction of the gallbladder - Forces a stone into the cystic duct - May present with pain (eg, in diabetics) |
|
|
In a patient with a history of gallstones, what may cause air in the biliary tree?
|
Fistula between gallbladder and small intestine
|
|
|
What causes gallstone ileus?
|
Gallstone obstruction of the ileocecal valve
|
|
|
How do you diagnose cholelithiasis? How do you treat?
|
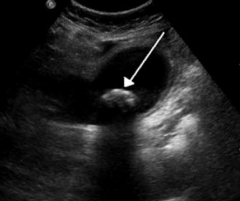
- Diagnose with ultrasound
- Treat with cholecystectomy if symptomatic |
|

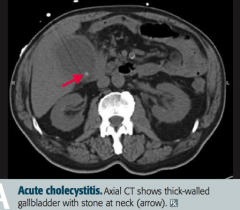
What does this ultrasound show?
|

Cholelithiasis (gallstones): distended gallbladder containing a large gallstone
|
|
|
What is the triad of symptoms seen in cholangitis (infection of bile duct)?
|
Charcot triad of cholangitis:
- Jaundice - Fever - RUQ pain |
|
|
What is the term for gallstones?
|
Cholelithiasis
|
|
|
What is the term for inflammation of the gallbladder?
|
Cholecystitis
|
|
|
What causes Cholecystitis?
|
Usually from cholelithiasis (gallstone)
- Most commonly blocking the cystic duct → 2° infection - Rarely ischemia or 1° infection (CMV) |
|
|
What physical exam test is present with Cholecystitis (inflammation of gallbladder)?
|
Murphy Sign: inspiratory arrest on RUQ palpation d/t pain
|
|
|
What is the Murphy Sign physical exam test? What does it indicate?
|
- RUQ palpation, if there is pain patient will have inspiratory arrest
- Diagnostic of Cholecystitis |
|
|
How do you diagnose Cholecystitis? |
- Ultrasound
- HIDA - Murphy's sign (+) |
|

When would you see a "porcelain" gallbladder? |
Chronic Cholecystitis (inflammation of gallbladder) - calcified gallbladder
|
|
|
How is "porcelain" gallbladder usually detected? How do you treat?
|
- Usually found incidentally on imaging
- Treat: prophylactic cholecystectomy d/t high rates of gallbladder carcinoma |

