![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
How can hormones be classified?
|
By their chemical nature
- Group 1: Steroids and Thyroid Hormones - Group 2: Peptides, Proteins, and Glycoproteins |
|
|
What are some of the Group 1 / steroid hormones?
|
- Cortisol
- Aldosterone - Testosterone (androgens) - Estrogens - Progestins - Calcitriol |
|
|
What are the Group 1 / thyroid hormones?
|
- Thyroxine (T4)
- Triiodothyronine (T3) |
|
|
What are some of the Group 2 / peptide hormones?
|
- Oxytocin
- Vasopressin (ADH) - Angiotensin - Somatostatin - Thyrotropin-Releasing Hormone (TRH) - Gonadotropin-Releasing Hormone (GnRH) - Gastrin |
|
|
What are some of the Group 2 / protein hormones?
|
- Insulin
- Glucagon - ACTH - Growth Hormone - Prolactin - CRH - GHRH - PTH - Calcitonin - CCK - Secretin |
|
|
What are some of the Group 2 / glycoprotein hormones?
|
- TSH
- Gonadotropins: FSH, LH, hCG |
|
|
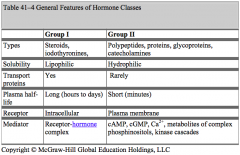
Group 1 Hormones:
- Types - Solubility - Transport proteins - Plasma half-life - Receptor location - Mediator |
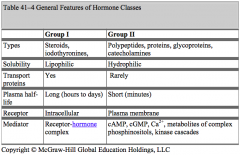
Group 1 Hormones:
- Types: steroids and thyroid hormones - Solubility: lipophilic - Transport proteins: yes - Plasma half-life: long (hours to days) - Receptor location: intracellular - Mediator: receptor-hormone complex |
|
|
Group 2 Hormones:
- Types - Solubility - Transport proteins - Plasma half-life - Receptor location - Mediator |
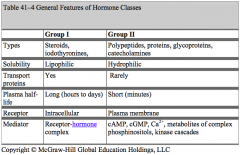
Group 2 Hormones:
- Types: peptides, proteins, glycoproteins, catecholamines - Solubility: hydrophilic - Transport proteins: rarely - Plasma half-life: short (minutes) - Receptor location: plasma membrane - Mediator: cAMP, cGMP, Ca2+, metabolites of complex phosphinositols, kinase cascades |
|
|
What are steroids all synthesized from?
|
Cholesterol
|
|
|
What do thyroid hormones contain?
|
Iodine
|
|
|
How do you distinguish between peptide hormones and protein hormones?
|
Peptides generally do not have tertiary structure, whereas proteins do have tertiary (folding) structure
|
|
|
What is similar about glycoproteins? How are they distinguished?
|
- Glycoproteins all have the same alpha subunit
- Their specificity is found in the beta subunit |
|
|
What are the two forms a hormone can be in the blood plasma?
|
- Protein bound
- Free |
|
|
What are the implications of a hormone being bound to protein or not being bound when traveling in the blood?
|
- With the bound hormone, only the free fraction is available for tissue uptake
- As the free fraction is depleted, additional hormone dissociates from the plasma-binding protein, making more available to distal portions of the tissue - All hormones that are not protein bound are quickly extracted in the proximal part of the tissue |
|
|
Which types of hormones are bound to plasma proteins? To which proteins? Implications?
|
Thyroid Hormones:
- >99.5% bound to TBG, Transthyretin, and Albumin - Plasma half-life is very long (4-6 days) and metabolic clearance is very slow Steroid Hormones: - 90-98% bound to plasma proteins (eg, cortisol to CBG and testosterone to SHBG) - Plasma half-life is 30-60 minutes (shorter than thyroid hormones but still longer than most peptides and proteins) |
|
|
Which types of hormones are NOT bound to plasma proteins? Implications?
|
Peptides and Protein hormones:
- Circulate only in free form - Plasma half-life is very short, <15 minutes and the clearance is very high - There are notable exceptions that will be covered in this unit |
|
|
What are the types of cell signaling?
|
- Endocrine
- Paracrine - Autocrine - Neurotransmitter - Neuroendocrine |
|
|
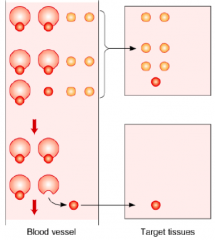
What type of hormones are secreted by endocrine signaling? Mechanism?
|
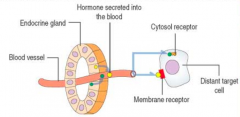
- Polypeptide (eg, thyrotrophic hormone) or steroid hormones (eg, estrogen)
- Secreted into blood vessels which are then carried to a target cell, which may be located at a considerable distance from the secreting cell |
|
|
What kind of signaling:
- Thyrotrophic Hormone is secreted by the Hypophysis and acts on the Thyroid Gland |
Polypeptide hormone - endocrine signaling
|
|
|
What kind of signaling:
- Estradiol is produced by the Ovaries and acts on the Endometrium |
Steroid hormone - endocrine signaling
|
|
|
What type of hormones are secreted by paracrine signaling? Mechanism?
|
- Hormones or growth factors (eg, glucagon and somatostatin)
- Act on an adjacent cell |
|
|
What type of signaling:
- Glucagon and somatostatin act on adjacent cells of the Islets of Langerhans that secrete insulin |
Paracrine Signaling
|
|
|
What type of hormones are secreted by autocrine signaling? Mechanism?
|

- Some hormones or growth factors (eg, prostaglandins and interleukins)
- Act on originating cell |
|
|
What type of signaling:
- Prostaglandins and interleukins are released from a cell and then act on that same cell |

Autocrine Signaling
|
|
|
What type of hormones are secreted by neurotransmitter signaling? Mechanism?
|
In response to a neural signal, neurons secrete neurotransmitters from the axon terminals to activate adjacent neurons
|
|
|
What kind of signaling:
- Neuron secretes a hormone from the axon terminals to activate adjacent neurons |
Neurotransmitter signaling
|
|
|
What type of hormones are secreted by neuroendocrine signaling? Mechanism?
|

- In response to a neural signal, neuroendocrine cells secrete a hormone into the blood to travel to a target organ
- Eg, norepinephrine acting on hepatocytes or adipocytes |
|
|
What kind of signaling:
- Norepinephrine is released from neuroendocrine cells in response to a signal to act on hepatocytes or adipocytes |

Neuroendocrine Signaling
|
|
|
Which hormones mainly act via nuclear receptors to increase transcription and translation? What is the speed of this process?
|

- Thyroid Hormones
- Estrogen (steroid hormone) - Slow |
|
|
Which hormones act via cytoplasmic receptors to increase transcription and translation?
|

Cortisol (steroid hormone)
|
|
|
Which hormones act on cell surface receptors and activate secondary messengers? What is the speed of this process?
|

Water-soluble hormones
- Peptide hormones - Catecholamines Rapid effect |
|
|
What determines a hormone or drugs mechanism of action?
|
Chemical nature (lipophilic or hydrophilic)
|
|
|
What determines the specificity of hormone action?
|
Expression of appropriate receptor in tissues determines which hormones will act on that tissue
|
|
|
What is the relationship between Thyroxine (T4) and Triiodothyronine (T3)?
|
- Thyroxine (T4) and Triiodothyronine (T3) readily diffuse through cell membrane
- Much of T4 is deiodinated / activated to form T3 which interacts with the Thyroid Hormone Receptor |
|
|
Which thyroid hormone has a greater binding affinity for the Thyroid Hormone Receptor? How does it get in this form? Action?
|
T3: Triiodothyronine
- Converted from T4 → T3 by Iodinase - T3 binds the Thyroid Hormone Receptor, bound as a heterodimer to Retinoid X receptor, which is part of the Thyroid Hormone Response Element of the gene - This either increases or decreases transcription of genes that lead to formation of proteins |
|
|
What is a way to block thyroid activity?
|
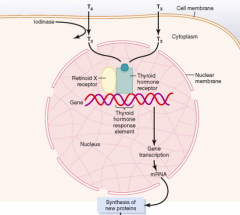
Block Iodinase which converts T4 → T3 (greater activity at thyroid hormone receptor)
|
|
|
What is the relationship between Testosterone and Dihydrotestosterone (DHT)?
|
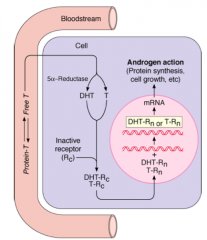
- T converted to DHT by 5α-Reductase in target tissue
- Both T and DHT can bind to the receptor, but DHT has greater activity at receptor - Both DHT-R and T-R can diffuse into nucleus and stimulate protein synthesis, cell growth, etc. |
|
|
How is Testosterone converted to Dihydrotestosterone (DHT)?
|
5α-Reductase
|
|
|
What is the relationship between androgens (eg, Androstenedione) and estrogens (eg, Estrone, E1, and Estradiol, E2)? Effects?
|
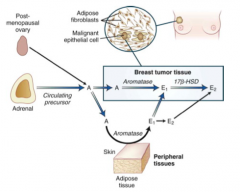
- Androgens can be converted to Estrogen by Aromatase in breast tumor tissue and adipose tissue
- Estrogens in breast tumor tissue will stimulate cancer growth - Also in fat men, the adipose tissue will stimulate conversion to estrogen, leading to feminization |
|
|
How do androgens get converted to estrogens? Where?
|
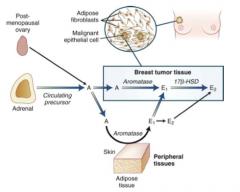
- Aromatase
- Breast tissue tumor or adipose tissue |
|
|
How can you block growth of a tumor in estrogen-sensitive breast cancer in post-menopausal women?
|
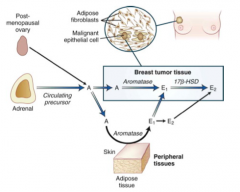
Aromatase inhibitors that inhibit conversion of Androgens (Androstenedione) to Estrogens (Estrone, E1, and Estradiol, E2), which stimulate the cancer growth
|
|
|
What is the action of Tamoxifen?
|
- Selective Estrogen Receptor Modulator (SERM)
- Useful for breast cancer by blocking estrogen receptors |
|
|
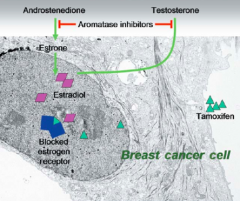
What happens in the simple feedback loop?
|
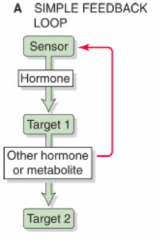
- Sensor detects some regulated variable (hormone/metabolite concentration)
- Sensor responds by modulating its secretion of a hormone - This hormone, in turn, acts on a target to modulate its production of another hormone or a metabolite - This may affect a second target - In addition, the other hormone or metabolite feeds back on the original sensor cell |
|
|
What is an example of a simple feedback loop?
|
![- Sensor (eg, β cell in a pancreatic islet) detects some regulated variable (e.g., plasma [glucose])
- Sensor responds by modulating its secretion of a hormone (e.g., insulin)
- This hormone, in turn, acts on a target (e.g., liver or muscle) t...](https://images.cram.com/images/upload-flashcards/85/25/91/3852591_m.png)
- Sensor (eg, β cell in a pancreatic islet) detects some regulated variable (e.g., plasma [glucose])
- Sensor responds by modulating its secretion of a hormone (e.g., insulin) - This hormone, in turn, acts on a target (e.g., liver or muscle) to modulate its production of another hormone or a metabolite (e.g., glucose) - This may affect a second target (e.g., making glucose available to the brain) - In addition, the other hormone or metabolite feeds back on the original sensor cell |
|
|
What is an example of the hierarchical control feedback "loop"?
|

- Under the influence of the cerebral cortex, the hypothalamus releases CRH
- CRH stimulates the anterior pituitary to release ACTH - ACTH stimulates the adrenal cortex to release cortisol - Cortisol acts on certain effector organs - In addition, the cortisol feeds back on both the anterior pituitary and the hypothalamus |
|
|
What is the most common type of feedback in the hypothalamic-pituitary-target gland axis? What happens?
|

Negative Feedback:
- The trophic hormones of the anterior pituitary gland has negative feedback effects on the hypothalamus - The target gland hormone has negative feedback effects on both hypothalamus and the anterior pituitary |
|
|
What is the type of feedback that occurs during late follicular and ovulatory phases of the menstrual cycle? What happens?
|

Positive Feedback:
- High levels of estradiol actually cause greater secretion of the hypothalamic releasing hormone and trophic hormones in that system - Results in a surge in pituitary hormone release that is responsible for ovulation at midcycle |
|
|
What is the type of feedback that occurs during childbirth? What happens?
|

Positive Feedback:
- Oxytocin is stimulated by distention of cervix toward the term of pregnancy and by contraction of the uterus during parturition - Signals are transmitted to the paraventricular (PVN) and supraoptic (SON) nuclei of the hypothalamus where they provide a POSITIVE feedback regulation of oxytocin release |
|
|
What allows for the positive feedback response of Oxytocin during childbirth?
|

- Increased number of oxytocin receptors
- Increased number of gap junctions between smooth muscle cells - Increased synthesis of prostaglandins, enhances the responsiveness of the uterine muscle |
|
|
What is the type of feedback that occurs during breastfeeding? What happens?
|

Positive Feedback:
- The suckling of the nipple of the lactating breast stimulates oxytocin release - The afferent sensory signals elicit an increase in oxytocin release into the circulation, which stimulates milk production and ejection |
|
|
What is the general term for too much production of the target gland hormone that exerts the systemic effect?
|

Primary Hyperfunction
|
|
|
What happens in Primary Hyperfunction?
|

- Too much production of the target gland hormone that exerts the important systemic effect
- Controlling hormone / factor is decreased |
|
|
What is the most common cause of Primary Hyperfunction?
|

Neoplasm (often benign adenoma) in gland of origin that has lost its normal control and now produces too much of its hormone in the absence of its normal stimulation (autonomous secretion)
|
|
|
What is the relative amount of the controlling hormone/factor in Primary Hyperfunction? Why?
|

Controlling hormone is decreased because of negative feedback
|
|
|
What are some examples of Primary Hyperfunction?
|
- Adrenal Cushing's Syndrome (primary hyperadrenocorticism)
- Graves' Disease (primary hyperthyroidism) |
|
|
What happens in Adrenal Cushing's Syndrome? What is it an example of?
|
- Cortisol overproduction from adrenal adenoma (usually) that suppresses ACTH release from the pituitary
- Diagnosis is made by measuring an increased cortisol and decreased ACTH - Aka ACTH-independent Cushing's Syndrome - Primary Hyperfunction |
|
|
What happens in Graves' Disease? What is it an example of?
|
- Excess thyroid hormone production independent of TSH
- Diagnosis is made by measured increased thyroid hormone and decreased TSH - Primary hyperthyroidism / hyperfunction |
|
|
What is the general term for too much production of the hormone that exerts the important systemic effect because it is being "told" to by overproduction of the stimulator of that hormone?
|

Secondary Hyperfunction
|
|
|
What happens in Secondary Hyperfunction?
|

- There is overproduction of the normal stimulator (this can be "within the reference range", however it should be suppressed, thus it is inappropriately not suppressed)
- This causes the hormone that exerts the important systemic effect to be overproduced |
|
|
What are some examples of Secondary Hyperfunction?
|
Cushing's Disease
|
|
|
What happens in Cushing's Disease? What is it an example of?
|
- Pituitary hypersecretion of ACTH causes ACTH-dependent Cushing's Syndrome
- Because cortisol is increased, pituitary secretion of ACTH should be suppressed, like in Adrenal Cushing's Syndrome - ACTH is not suppressed (although often in the reference range for ACTH) - inappropriately not suppressed maintains cortisol hypersecretion and adrenal hypertrophy |
|
|
What is the general term for loss of target gland function due to a pathophysiological process directly in the gland?
|

Primary Hypofunction
|
|
|
What happens in Primary Hypofunction?
|

- Target gland hormone will be low
- Normal stimulator of that hormone will be increased in an attempt to restore target gland function |
|
|
What can cause Primary Hypofunction?
|

Pathophysiological process directly in the gland:
- Auto-immune destruction - Surgical removal |
|
|
What are some examples of Primary Hypofunction?
|
- Primary Adrenal Insufficiency
- Primary Hypothyroidism (Hashimoto's Thyroiditis) - Menopause - Male Primary Hypogonadism |
|
|
What happens in Primary Adrenal Insufficiency? What is it an example of?
|
- Irreversible adrenal gland destruction (usually d/t auto-immune or infectious process)
- Cortisol secretion is low and ACTH secretion is high because the pituitary has been relieved of cortisol negative feedback - Example of Primary Hypofunction |
|
|
What happens in Hashimoto's Thyroiditis? What is it an example of?
|
- Thyroid has been partially or totally destroyed by an auto-immune process
- Thyroid hormone secretion is low and TSH secretion is high because pituitary has been relieved of thyroid hormone negative feedback - Example of Primary Hypofunction |
|
|
What happens in Menopause? What is it an example of?
|
- Ovarian steroid secretion has ceased
- Estrogen is low and FSH and LH are increased - Example of Primary Hypofunction |
|
|
What happens in Male Primary Hypogonadism? What is it an example of?
|
- Testicular function is lost (eg, d/t auto-immune process)
- Testosterone secretion is low and FSH and LH are increased - Example of Primary Hypofunction |
|
|
What is the general term for when a normal stimulator of a target gland is inadequate and the target gland does not produce a normal amount of its hormone (and often atrophies as a result)?
|

Secondary Hypofunction
|
|
|
What happens in Secondary Hypofunction?
|
- Normal stimulator of target gland is inadequate and target gland does not produce a normal amount of its hormone
- Target gland may atrophy as a result - The normal stimulator of the target gland is often "in the reference range" - thus it is "inappropriately not increased" |
|
|
What are some examples of Secondary Hypofunction?
|
Hypopituitarism
- Secondary Adrenal Insufficiency - Secondary Hypothyroidism - Secondary (Hypogonadotropic) Hypogonadism |
|
|
What is the term for a loss of anterior pituitary function? What can cause this?
|
Hypopituitarism - can be d/t auto-immune processes, trauma, and infarction
|
|
|
What are the implications of hypopituitarism?
|
- Secondary adrenal insufficiency
- Secondary hypothyroidism - Secondary (hypogonadotropic) hypogonadism |
|
|
What happens in Secondary Adrenal Insufficiency?
|
- Cortisol secretion is low
- Plasma ACTH is not elevated (although it is often "normal" but inadequate to restore adrenal function to normal) |
|
|
What happens in Secondary Hypothyroidism?
|
- Thyroid hormone secretion is low
- Plasma TSH is not elevated (although it is often "normal" but inadequate to restore thyroid function to normal) |
|
|
What happens in Secondary (Hypogonadotropic) Hypogonadism?
|
- Ovarian or testicular steroid secretion is low
- Plasma LH and FSH are not elevated (although it is often "normal" but inadequate to restore gonadal function to normal) |
|
|
Primary Hypofunction:
- Target gland function: ↑/↓/⟷ - Controlling hormone/factor: ↑/↓/⟷ |
- Target gland function: ↓ (cause of problem)
- Controlling hormone / factor: ↑ (loss of negative feedback) |
|
|
Secondary Hypofunction:
- Target gland function: ↑/↓/⟷ - Controlling hormone/factor: ↑/↓/⟷ |
- Target gland function: ↓ (result of problem)
- Controlling hormone / factor: ↓ or ⟷ (loss of negative feedback) |
|
|
Primary Hyperfunction:
- Target gland function: ↑/↓/⟷ - Controlling hormone/factor: ↑/↓/⟷ |
- Target gland function: ↑ (cause of problem)
- Controlling hormone / factor: ↓ (too much negative feedback) |
|
|
Secondary Hyperfunction:
- Target gland function: ↑/↓/⟷ - Controlling hormone/factor: ↑/↓/⟷ |
- Target gland function: ↑ (result of problem)
- Controlling hormone / factor: ↑ or ⟷ (too much negative feedback) |

