![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
5 Cards in this Set
- Front
- Back
- 3rd side (hint)

Examination of the thyroid gland With lymph nodes Face , eyes |
patient to sit comfortably at the edge of the bed or on a chair. •Stand back and observe, look specially at the face. • from the front look at the thyroid and thyroid scars indicating past surgery. • Ask wether there is pain or tenderness and then feel the thyroid from behind.Be gentle, because thyroid examination can be uncomfortable for patients. • Feel the isthmus, which overlies the thyroid cartilage, with your right middle and index fingers, and then feel the lobes. ~Note any diffuse goitre or ~area of focal nodularity. ~Note the gland’s size and texture. • Consider asking the patient to swallow a glass of water if you find a goitre, to see and feel whether it is readily mobile. • Feel for lymph nodes – ~supraclavicular, ~submandibular, ~postauricular, ~suboccipital. If there are palpable nodes, note if they are □separate and tender (reactive hyperplasia), □hard and clustered together (carcinoma), □soft and rubbery (lymphoma), □mobile or fixed.
• Auscultate the thyroid gland bilaterally for bruits.
• Examine the eyes for features of thyroid eye disease Proptosis Exopthslmos Lid retraction Impaired eye lid closure + corneal ulceration Lid lag Ophthalmoplegia Visual loss • Observe the face, skin and hair for signs of hyperthyroidism or hypothyroidism. • Feel the pulse. • Inspect the palms for erythema and feel for sweat. •Note any clubbing. Note any tremor with the arms outstretched. •Ask your patient to abduct their shoulders to assess for proximal muscle weakness. • Look at the legs for pretibial myxoedema. • Test the ankle reflexes. • You will probably discover early in the course of the examination if you are dealing with a thyroid lump, hyperthyroidism or hypothyroidism, directing your assessment accordingly. |

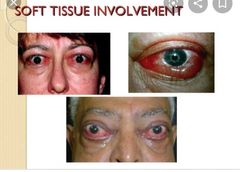
Swelling and redness of the eyelids, periorbital tissues and conjunctiva (chemosis refers to corneal oedema)
• Proptosis (anterior displacement of the globe, best seen from above, standing behind the patient) resulting in exophthalmos– • lower sclera visible between cornea and lower lid (lower or upper lid retraction refer to visible sclera between the cornea and the lid) • Impaired lid closure and corneal ulceration, especially if levator muscle affected. • Moving your finger downwards quite fast and asking the patient to follow it, while fixing their forehead with your other hand, will elicit lid lag • Note that lid retraction and lid lag are due to excess sympathetic activity and not specific to Graves’ disease • Ophthalmoplegia causing diplopia (often a complex ophthalmoplegia involving numerous ocular muscles) • Visual loss due to compression of the optic nerve at the orbital apex (exophthalmos is not always present in this sight-threatening situation and does not correlate well with disease severity; indeed, patients with minimal exophthalmos may be at higher risk of optic nerve compression because displacement of the eye forwards helps to decompress the optic nerve)
Common early symptoms of TED include altered appearance, eye surface symptoms (grittiness, photophobia, lacrimation), diplopia (especially at extremes of gaze), blurred vision (due to tear film abnormalities, refractive problems or subtle extraocular palsy – but blurred vision that does not improve with blinking,refraction / pinhole or by occluding either eye may be due to optic nerve compression) and retro-orbital ache. The natural history of TED comprises an initial progressive phase lasting a few months before reaching a peak before it improves spontaneously. These changeable phases can last 1–2 years until a chronic, ‘burnt-out’stage is reached when no further change is likely. Atypical features requiring orbital imaging include ■unilateral disease, ■no evidenceof thyroid disease, ■absence of upper lid retraction, ■divergent strabismus, ■diplopia alone and diplopia that is worse towards the end of the day.
The differential diagnosis includes ▪︎myasthenia gravis, ▪︎orbital myositis, ▪︎chronic progressive external ophthalmoplegia, ▪︎orbital tumours, ▪︎carotid–cavernous fistula and any ▪︎inflammatory orbitopathy (e.g. Wegener’s granulomatosis). |
|
|
Thyrotoxicosis and hyperthyroidism• Thyrotoxicosis is the clinical syndrome that arises fromexcessive circulating thyroid hormone levels and is usuallycaused by Graves’ disease or toxic nodular thyroid disease,both of which are forms of hyperthyroidism• Hyperthyroidism is the term for overactive tissue within thethyroid gland that causes an overproduction of thyroidhormones• Hyperthyroidism is thus a cause of thyrotoxicosis, buthyperthyroidism and thyrotoxicosis are not synonymous and, forinstance, thyrotoxicosis could be caused by ingestion ofexogenous thyroid hormone or destructive thyroiditis causingrelease of stored hormone
You are a 35-year-old woman admitted to the acute medical unit with tachycardia and tremor. Your general practitioner suspected an overactive thyroid and sent you in. You have also noticed weight loss and heat intolerance and experienced diarrhoea and generalised anxiety over the past few months. You have slight protrusion of the eyeballs with occasional redness. You are usually well. You are especially concerned because you have just discovered that you are pregnant. |

Focused history and examination Initial history 1.Ask about symptoms of hyperthyroidism or thyrotoxicosis Symptoms of thyrotoxicosis (of any cause) • Weight loss• Increased appetite • Heat intolerance • Preference for cold and sweating • Diarrhoea
• Tremor • Hyperactivity, irritability, insomnia or anxiety
• Depression (especially elderly) • Oligomenorrhoea and loss of libido
• Polyuria
• Weakness and fatigue
Initial examination • Look for one or more of the triad of groups of signs. 1. Hyperthyroidism ▪︎The hands are warm and sweaty with palmar erythema. ▪︎Tremor is often obvious (with the arms extended a piece of paper on the hands detects subtle fine tremors). ▪︎There is tachycardia at rest (usually sinus tachycardia, may be atrial fibrillation). ▪︎There may be proximal muscle weakness.
These signs may occur in thyrotoxicosis of any cause. A bruit bilaterally over the thyroid is specific to Graves’ disease.
2. Thyroid eye disease (TED) TED has an autoimmune basis, with associated thyroid autoimmunity always detectable, probably reflecting shared autoantigens between the thyroid and the orbit. Most patients have concurrent thyrotoxicosis due to Graves’ disease and the classic presentation is thyrotoxico-sis, diffuse goitre and exophthalmos.
Some patients develop TED in the months before becoming thyrotoxic,and occasionally it precedes thyrotoxicosis by years.
Extraocular muscles, retro-ocular fat and connective tissue,eyelids and anterior periorbital tissues are affected by •lymphocyte infiltration, •inflammatory cytokine cascades and •interstitial oedema, resulting in volume expansion.
Graves’ophthalmopathy occurs clinically in around 60% of patients and is radiologically detectable in around90%.
3.Pretibial myxoedema This is rare (1–2% of Graves’ disease) but specific to Graves’ disease. There are elevated shin lesions with well-defined edges. Lesions may be nodular or plaque-like, purplish red or brown and the skin is shiny, with a thickened, orange-peel appearance. Lesions can occur at other sites. They are usually painless. Coarse hairs tend to occur in the vicinity. Look also for thyroid acropachy(clubbing) and onycholysis (Plummer’s nails), which affect a small minority of patients.
Further assessment • Be aware that thyrotoxicosis and hyperthyroidism aren not synonymous and consider the causes of thyrotoxicosis
■primary hyperthyroidism ~Graves- IgG antibodies act on TSH receptors in the thyroid and stimulate- Diffuse , painless goitre ~Toxic nodular goiter[ toxic multinodular goitre]- Commenest cause in elderly yet the cause is unknown- painful goitre ~Toxic adenoma- solitary secreting adenoma-thyrotoxicosis without goitre ~other-metastatic thyroid cancer/ectopic thyroid tissue-uncommon
■secondary hyperthyroidism ~thyroid secreting pituitary adenoma - part of wider pituitary disease TSH detected with high freeT4 ,T3 levels ~thyroid hormone resistance disease - thyrotoxicosis uncommon High free T4,T3 due to peripheral resistance to thyroxine ■thyrotoxicosis without hyperthyroidism ~destructive thyroiditis ▪︎subacute (dequreveins)-Viral origin- small tender goitre with high ESR -Initial thyrotoxicosis without hyperthyroidism due to release of stored hormones- followed by hypothyroidism in weeks and recovery within 3 to 6 months ,responding to steroids. ▪︎ post partum thyroiditis - similar to viral thyroiditis but painless goiter ~drug induced- Amaidarone, lithium inducing autoimmunity or inflammatory thyroiditis
~excess thyroid hormone ingestion - suggestive history
• Explore concerns.Feedback to patient All of your symptoms are very suggestive of anoveractive thyroid gland. The eye problems can alsobe caused by this. We should aim to confirm thisdiagnosis with blood tests and then settle thingsdown with treatment. In terms of treatment wecould firstly settle down the immediate symptomswith medication (beta blockers) and then get expertadvice on treating the problem in the longer term;options usually include tablets or a radioactivetreatment to the thyroid gland, and occasionally surgery. Most patients will settle with the morestraightforward of the options, though the besttreatment is determined by a number ofconsiderations, not least pregnancy. In pregnancydrugs treatment is going to be the safest option andthe condition can be managed very effectively butbest under the supervision of a specialist in thyroidproblems. I’d be happy to answer any furtherquestions or concerns that you may have. Comments She has hyperthyroidism - diffuse goiter And thyrotoxicosis- Exophthalmos
Management plan Investigations- thyroid function tests Graves is a clinical diagnosis Even though tests such as antibodies to serum thyroglobilin and thyroxine peroxidase can be done. Its positive in 80% of graves patients and 20% of normal people. TSH receptor stimulating antibodies are not widely available. Radioiodine uptake can be done, To differentiate presence of hyperthyroidism when uptake is high. In thyrotoxicosis without hyperthyroidism uptake is low or absent. Can help in detecting a toxic adenoma where uptake is higher with complete suppression of surrounding tissues. [They are not responsive to carbomazole ]
Hyperthyroidism management Thyrotoxicosis management Carbimazole-inhibit thyroxine production by peroxidase Propranolol-symptomatic Iodine treatment- slow but very effective and contraindicated in active ophthalmopathy Thyroid surgery Graves eye disease management Stop smoking Corneal lubricants Steroids |
SUMMARY AND RECOMMENDATIONS ●Hyperthyroidism is the most common feature of Graves' disease, affecting nearly all patients, and is caused by thyroid-stimulating hormone (TSH, thyrotropin)-receptor antibodies (TRAb) that activate the receptor, thereby stimulating thyroid hormone synthesis and secretion as well as thyroid growth (causing a diffuse goiter)
●The therapeutic approach to Graves' hyperthyroidism consists of both rapid amelioration of symptoms with a beta blocker and measures aimed at decreasing thyroid hormone synthesis with the administration of a thionamide, radioiodine ablation, or surgery (table 1). The choice of therapy should involve active discussion between clinician and patient; it may also be determined by the severity of the patient's hyperthyroidism.
●Assuming there are no contraindications to its use, we recommend using a beta blocker for patients with moderate to severe hyperadrenergic symptoms until euthyroidism is achieved by thionamides, radioiodine, or surgery (Grade 1B). We typically start with atenolol 25 to 50 mg daily and increase the dose as needed (up to 200 mg daily) to reduce pulse to under 90 beats per minute if blood pressure allows.
●For patients with significant symptoms of hyperthyroidism, or patients with a significant risk of hyperthyroid complications (eg, older age, cardiovascular disease), we suggest a thionamide in addition to beta blockers to achieve euthyroidism quickly (Grade 2B). Methimazole is now used almost exclusively (except during the first trimester of pregnancy and in patients who have minor drug reactions to methimazole who refuse radioiodine or surgery) because of its longer duration of action, allowing for once daily dosing, more rapid efficacy, and lower incidence of side effects.
●Once patients with more severe hyperthyroidism are euthyroid on methimazole, we suggest definitive therapy with radioiodine or surgery (Grade 2B). A one- to two-year course of methimazole or long-term methimazole are both reasonable alternatives.
In the absence of moderate to severe orbitopathy, we suggest radioiodine therapy if definitive therapy is desired, given its lower cost and lower complication rate than surgery (Grade 2B).
●For patients who are tolerating hyperthyroid symptoms and who are not at risk for complications from hyperthyroidism, radioiodine can be used as initial therapy (without antithyroid drug pretreatment). Primary antithyroid drug therapy is an alternative option and may be preferable for patients with mild disease and small goiters, who are more likely to achieve a remission after a year of treatment. ●For patients with hyperthyroidism due to a very large or obstructive goiter, we suggest surgery (Grade 2C). It is also indicated for patients who are allergic to thionamides and are unable to or do not want to receive radioiodine. Surgery may also be preferred in patients with active orbitopathy.
●We advise women desiring to become pregnant in the near future to consider radioiodine or surgery six months in advance of a planned pregnancy to avoid the need for a thionamide during the pregnancy. However, if radioiodine or surgery is not desired, propylthiouracil (PTU) therapy would be the preferred drug during the first trimester of pregnancy.
●Several concerns of the patient also may influence the choice of therapy. As an example, the recommendation to avoid close contact with young children for several days after radioiodine administration may make this treatment temporarily unattractive if alternative childcare is unavailable. Patient fears regarding radiation exposure or agranulocytosis from thionamides should also be considered. ●Whatever treatment is used, initial monitoring following treatment should consist of periodic clinical assessment and measurements of serum free thyroxine (T4) and total triiodothyronine (T3) levels. Measurement of serum TSH can be misleading in the early follow-up period because it can remain low for weeks or even months, even when the patient is biochemically euthyroid or even hypothyroid, with serum free T4 values well within or even below the normal range |
|
|
Scenario You have 10 minutes. The examiners will alert you when 6 minutes have elapsed, stop you at 8 minutes, and in the remaining 2 minutes ask you to report your findings, the diagnosis or differential diagnosis, and a management plan. Patient information You are a 70-year-old woman admitted to the acute medical unit with a possible non-ST elevation myocardial infarction. You are now stable. You have also noticed extreme tiredness, weight gain and cold intolerance and experienced constipation and mood change over the past few months. You are usually well, but you are always so tired and wish you could have more energy. Focused history and examination Initial history • Ask about symptoms of features of hypothyroidism (Box 5.50). Initial examination • You may miss hypothyroidism and think, ‘just another little old lady’. Many of the clinical features are non-specific and insidious. They include excess weight, myxoedematous facial features (thick and coarse, with periorbital oedema – puffiness especially below the eyes, and sometimes hoarseness), dry skin, and fine, brittle hair with loss of the outer eyebrows (Fig. 5.85). There may be delayed relaxation of ankle and other deep tendon reflexes. Further assessment • Consider the possible causes of hypothyroidism (Box 5.51). The commonest cause in developed countries is autoimmune thyroiditis, which may be associated Re: Mrs Marjorie Dawe, aged 70 years This woamn has been admitted to the acute medical unit with a possible non-ST elevation myocardial infarction and is stable but reports to the doctor that she has become extremely tired in the past few months. Your task is to assess the problem by means of a focused history and focused examination. You should then advise the patient of your probable diagnosis and plan, and address any questions or concerns raised by the patie |
5.50 Symptoms of hypothyroidism • Tiredness/ exhaustion /somnolence • Weight gain • Preference for warmth /intolerance of cold • Mood change including depression, or slow cognition • Constipation • Menstrual disturbance including menorrhagia • Myalgia, especially calf discomfort and stiffness • Carpal tunnel syndrome • Hearing impairment |
|
|
|
Re: Mrs Marjorie Dawe, aged 70 years. This woamn has been admitted to the acute medical unit with a possible non-ST elevation myocardial infarction and is stable but reports to the doctor that she has become extremely tired in the past few months.Your task is to assess the problem by means of a focused history and focused examination. You should then advise the patient of your probable diagnosis and plan, and address any questions or concerns raised by the patient. |
You are a 70-year-old woman admitted to the acute medical unit with a possible non-ST elevation myocardial infarction. You are now stable. You have also noticed extreme tiredness, weight gain and cold intolerance and experienced constipation and mood change over the past few months. You are usually well, but you are always so tired and wish you could have more energy.Focused history and examinationInitial history ■Ask about symptoms of features of hypothyroidism • Tiredness/ exhaustion /somnolence • Weight gain • Preference for warmth /intolerance of cold • Mood change including depression, or slow cognition • Constipation • Menstrual disturbance including menorrhagia • Myalgia, especially calf discomfort and stiffness • Carpal tunnel syndrome • Hearing impairment Initial examination • You may miss hypothyroidism and think, ‘just another little old lady’. Many of the clinical features are non-specific and insidious. They include - excess weight, myxoedematous facial features (thick and coarse, with periorbital oedema – puffiness especially below the eyes, and sometimes hoarseness), dry skin, and fine, brittle hair with loss of the outer eyebrows. There may be delayed relaxation of ankle and other deep tendon reflexes. Further assessment • Consider the possible causes of hypothyroidism . The commonest cause in developed countriesis autoimmune thyroiditis, which may be associated with goitre (Hashimoto’s thyroiditis) or, with equal frequency, thyroid atrophy. • Be aware of serious complications of severe hypothyroidism – ◇serous effusions (pleural,pericardial, peritoneal, joint), ◇heart failure,bradycardia, ◇dyslipidaemia (raised total cholesterol and low-density lipoprotein with increased cardiovascular disease risk), ◇anaemia (iron deficiency,macrocytic, pernicious, normochromic, normocytic), ◇cerebellar dysfunction, psychiatric manifestations,and impaired consciousness (myxoedema coma). • Explore concerns. Causes of hypothyroidism • Autoimmune Hashimoto’s thyroiditis* • Atrophic autoimmune thyroiditis • Iatrogenic – thyroidectomy for hyperthyroidism or thyroid cancer, radioiodine therapy • Destructive thyroiditis – painful subacute thyroiditis (also known as De Quervain’s thyroiditis), silent thyroiditis,postpartum thyroiditis • Iodine deficiency (in some parts of the world remains highly prevalent) • Drugs – carbimazole, methimazole, propylthiouracil, iodine,amiodarone, lithium, interferons, thalidomide, sunitinib,rifampicin • Congenital hypothyroidism – thyroid aplasia or hypoplasia,defective biosynthesis of thyroid hormones • Disorders of the pituitary or hypothalamus (secondary hypothyroidism) *Hashimoto’s thyroiditis is the commonest cause of hypothyroidism, in which dense lymphocytic infiltration of the thyroid gland produces a diffuse or finely micronodular goitre. It typically affects middle-aged and older women, presenting with hypothyroidism, goitre, or both and is autoimmune. Associated conditions include ◇vitiligo, ◇pernicious anaemia, ◇type 1 diabetes, ◇Addison’s disease and ◇premature ovarian failure. Feedback to patient All of your symptoms are very suggestive of an underactive thyroid gland. We should aim to confirm this diagnosis with blood tests and then settle things down with treatment. This is a very common condition and treatment is usually successful with a small dose of medication. One thing for us to consider, especially if this turns out to be a small heart attack, is cholesterol levels since an underactive thyroid can provoke high cholesterol levels. You will of course be feeling under the weather as a result of the heart attack but it is very likely that an underactive thyroid has been making you feel chronically tired and hopefully treatment would help this. I’d be happy to answer any further questions orconcerns that you may have. Feedback to examiners Summarise the key history and examination findings This woman has numerous symptoms and signs of hypothyroidism. Provide a diagnosis or differential diagnosis with supporting evidence.-Hashimoto’s thyroiditis would be the most likely cause. Outline an investigation and management plan. Thyroid function tests are needed with a view to treatment . Diagnosis of primary hypothyroidism is confirmed by an increase in serum thyroid-stimulating hormone (TSH) concentration. If the cause is autoimmune, circulating antibodies directed at thyroid peroxidase (formerly known as microsomal antibodies) or thyroglobulin are detectable in over 90% and about 70% of patients,respectively. Hypothyroidism in older patients and those with ischaemic heart disease should always be managed with caution. Because longstanding hypothyroidism may cause bradycardia, which can mask substantial asymptomatic coronary artery disease, levothyroxine should be replaced cautiously in patients over 60 years or those with known ischaemic heart disease. Particular caution is needed in profound and longstanding hypothyroidism (TSH > 50 mU/l). Here,or in active angina or following a recent acute coronary syndrome, the starting dose of levothyroxine should be 12.5 or 25 µg daily,increased every 3–6 weeks until euthyroidism is achieved. |
|
|
|
Mrs Sue Richards, aged 40 years.This woman was admitted to the orthopaedic ward for a carpal tunnel release operation. She mentioned to the orthopaedic doctors that she has a swelling in her neck and they have asked for the opinion of a physician. You were asked by your consultant to assess the suspected swelling in her neck.Your task is to assess the problem by means of a focusedhistory and focused examination. You should then advise the patient of your probable diagnosis and plan, and address any questions or concerns raised by the patient
Patient information You are a 40-year-old woman on the orthopaedic ward and you mentioned to the admitting doctor that your neck seemed swollen. One of the medical doctors has beenasked to see you about this. You are having a short admis-sion to have surgery for carpal tunnel syndrome. You have not mentioned the neck swelling to a doctor before but your sister, who has an underactive thyroid, has been commenting on it for a few years. You do not have any of the symptoms your sister had when her thyroid was underactive. Indeed you feel well. Your weight is stable. Your skin and hair are normal. You do not seem to feel the heat or cold any more than anyone else. Your bowel worksnormally. You do not have any problem with swallowing.You want to know why your neck seems swollen and whether there might be something wrong with yourthyroid gland and what should be done.
Focused history and examination Initial history • Ask about symptoms of the neck lump. Most are asymptomatic and most are euthyroid (endocrine glands generally comprise much redundant tissue).
Pressure symptoms (dysphagia, dysphonia, stridor)or pain (especially with bleeding into an adenoma)are possible.
• Ask about symptoms of hyperthyroidism and hypothyroidism
Initial examination • Note if there is a ■diffuse goitre, ■a multinodular goitre ■or a single thyroid nodule
Further assessment • Consider causes.
Causes of a thyroid lumpDiffuse goitre• Simple, non-toxic goitre• Graves’ disease• Hashimoto’s thyroiditis• Subacute thyroiditis• LymphomaMultinodular goitre• Toxic multinodular goitre• Hashimoto’s thyroiditisSingle nodule• Adenoma• Cyst• CarcinomaWorldwide, iodine deficiency is a common cause of goitre
The key issue is to exclude malignancy with further investigations. ■Papillary thyroid carcinoma-Most commonPeak incidence young womenLocally invasivePrognosis good if detected early ■Follicular thyroid carcinomaPeak incidence in older peopleMetastases more likelyPrognosis still good if detected early ■Hurthle cell carcinoma- Uncommon Poor prognosis ■Anaplastic carcinomaPeak incidence in older peopleAggressive with high mortality ■Lymphoma- UncommonGood prognosis Explore concerns.
Feedback to patient-You have a swelling of the thyroid gland, sometimes known as goitre. These swellings do not usually giverise to symptoms of an overactive or underactive thyroid but of course the swelling itself can be uncomfortable and we should aim to establish whathas caused it and then treat it.
Usually thyroid lumps are benign but occasionally not and I think weshould arrange a thyroid scan in the first instance to assess it in more detail.
We should also arrange some blood tests to make sure that the thyroid gland is not becoming overactive or underactive. I’d be happy to answer any further questions or concerns that you may have.Feedback to examiners.Summarise the key history and examination findingsThis lady has a thyroid lump, possibly an asymmetric or possibly a large single nodule. |
Provide a diagnosis or differential diagnosis with supporting evidenceThe possible causes are wide ranging and include a simple non-toxic goitre, Graves’ disease, autoimmunethyroiditis, lymphoma or a large nodule.Outline an investigation and management planShe will require imaging to determine the nature ofthe mass and thyroid function tests to determinethyroid status. Thyroid lumps are common, oftensilent, and increasingly prevalent with age. Nodulesmay be solid, cystic, mixed (e.g. cystic degenerationwithin an adenoma) or calcified. The key issue is toexclude malignancy, although most thyroid lumps arebenign. It is not possible without scanning todetermine if a single palpable nodule is part of amultinodular thyroid. Measurement of size andexclusion of tracheal compression are best assessedby computed tomography or magnetic resonanceimaging of the neck and thoracic inlet. Radionuclideimaging is less often used these days as it does notabsolutely exclude malignancy, and although mostcold nodules are benign and malignant nodules hotthe latter may sometimes be cold. Fine-needleaspiration is the gold standard for diagnosis short ofopen excision. It is not possible to distinguishbetween a follicular adenoma and a follicularcarcinoma on cytology and all follicular lesionsshould be excised. Indications for surgery includemalignancy, concern about malignancy (e.g. largecysts are more likely to be malignant), continuingenlargement, pressure symptoms (dysphagia,dysphonia, stridor or pain) and cosmetic reasons. |
|

