![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
7 Cards in this Set
- Front
- Back
|
What is dobutamine?
|
This is a "pressor" medication.
Inotropic agents — Patients with MI, pulmonary congestion and marginal or low blood pressure often require circulatory support with inotropic and vasopressor agents and/or intra-aortic balloon counterpulsation to relieve pulmonary congestion and maintain adequate perfusion. (See "Intraaortic balloon pump counterpulsation"). The 2004 ACC/AHA STEMI guidelines suggest using dopamine in hypotensive patients with clinical evidence of shock and using dobutamine in hypotensive patients without clinical evidence of shock [2]. Dopamine — Although not mentioned in the 2006 HFSA ADHF guidelines, dopamine is recommended for hypotensive STEMI patients with clinical evidence of shock in the 2004 ACC/AHA guidelines. Its actions are complex and dose-dependent: At low doses of 1 to 3 µg/kg per min, dopamine acts primarily on dopamine-1 receptors to dilate the renal and mesenteric artery beds [7]. At 3 to 10 µg/kg per min, dopamine also stimulates beta-1 adrenergic receptors and increases cardiac output, predominantly by increasing stroke volume with variable effects on heart rate. At medium-to-high doses, dopamine also stimulates alpha-adrenergic receptors, producing arterial and venous constriction that may compromise systolic function and filling pressures. However, a study of 13 patients with class III or IV chronic HF with severe LV systolic dysfunction suggested that renal arterial vasodilation and improvement in cardiac output may persist as the dopamine dose is titrated up to 10 µg/kg per min [7]. Dopamine should be reserved for hypotensive patients without shock for whom an increase in arterial pressure is considered a priority |
|
|
What is the steroid that is used for acute spinal cord injuries?
|
IV methylprednisolone in a dose of 30mg/kg over 15 minutes, followed in 45 minutes by a continuous infusion of 5.4mg/kg/hour for 23 hours.
|
|
|
What is the treatment for acute adrenal insufficiency?
|
Hydrocortisone IV 100mg iv bolus, then 300mg/day in divided doses every 8 hours or as a continuous infusion for 48 hours. Once patient is stable can change to oral.
|
|
|
You are called overnight by the ICU nurse on your patient. He is a 56 year old man that had the sudden onset of difficulty breathing. The symptoms began 2 hours prior. He has a significant PMHx of DM, HTN, tobacco abuse. He is post-op cystectomy for bladder cancer.
On exam he is in mild respiroatyr distress, his lung exam is basically normal, CXR is normal, pulse is 120/min, RR 30/min. His pulse oximetry is 87% on room air. You order a V/Q scan that shows a high probability for a PE, what is your next step? What if the VQ scan was indeterminate? Is there a role for ordering an ABG for this patient? |
HPatients with high clinical probability of PE and a high-probability V/Q scan had a 95 percent likelihood of having PE eparin bolus followed by the heparin nomogram. You are attempting to prevent the blood clot from increasing in size or new clots from forming and breaking off to the lungs or the heart or the brain.
That is a tough call because your pre-test probability in this patient is so high. You would probably then order a PE protocol CT, if the Cr was too high or for some reason the patient couldn't get one then you could attempt starting Heparin without a definitive diagnosis. Arterial blood gas (ABG) measurements and pulse oximetry have a limited role in diagnosing PE [1]. ABGs usually reveal hypoxemia, hypocapnia, and respiratory alkalosis. Patients with room air pulse oximetry readings <95 percent at the time of diagnosis are at increased risk of in-hospital complications, including respiratory failure, cardiogenic shock, and death [2]. The typical arterial blood gas findings are not always seen. As an example, massive PE with hypotension and respiratory collapse can cause hypercapnia and a combined respiratory and metabolic acidosis (the latter due to lactic acidosis). In addition, hypoxemia can be minimal or absent. A PaO2 between 85 and 105 mmHg exists in approximately 18 percent of patients with PE |
|
|
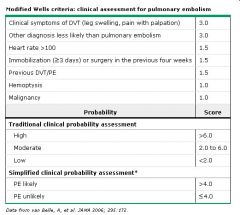
What are the Modified Wells Criteria for assessing clinical risk of PE?
|
|
|
|
What is the definition of brain death in the US?
|

|
|
|
If you have a patient that you suspect has compartment syndrome and you check their compartment pressures, what number is suggestive of compartment syndrome?
|
The exact pressure in the compartment to which ischemia occurs and blood flow stops to that part of the leg is controversial however a pressure higher than 30 is generally accepted as the number.
|

