![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
34 Cards in this Set
- Front
- Back
|
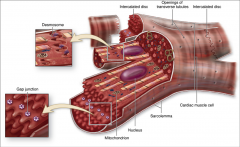
cardiac muscle
|
- central nuclei
- cross-striation - intercalated disks = fascia adherens and numerous desmosomes - cells have Y shape - gap junction between cells - lots of mitochondria - fibrils of reticular fibers - contact between cells accomplished by interdigitation in transverse region |
|
|
Y shape fibers
|
- cells often branched
- allow muscle fibers to interweave in a more complicated arrangement within fascicles - produces efficient contraction mechanism for emptying heart |
|
|
junction specializations of intercalated disk
|
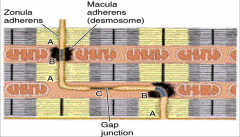
- zonulae adherentes anchor actin filaments of the terminal sacromeres to plasmalemma
- desmosomes bind cells together, preventing their separation during contraction cycles - gap junctions couple cells and provide for spread of contractile depolarization - zonulae adherentes and desmosomes in transverse portion - gap junctions restricted to longitudinal portions where least stress |
|
|
membrane bound granules
|
- aggregated at nuclear pores
- most abundant in muscle cells of right atrium - smaller quantities found in left atrium and ventricles - atrial granules contain precursor of atrial natriuretic factor |
|
|
atrial natriuretic factor (ANF)
|
- target cells of kidneys to bring about sodium and water loss
- opposes action of aldosterone and antidiuretic hormone |
|
|
features of cardiac muscle
|
- myofibrils less dense and organized than skeletal muscle
- alternate with abundant mitochondria - mitochondria may occupy up to 40% of cytoplasm - heart relies on aerobic respiration - T tubules are larger and more numerous compared to skeletal - diads rather than triads - SR reduced |
|
|
cardiac sacromere
|
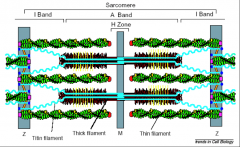
- actin, myosin, tropomyosin
- thin filaments anchored by Z-disk by cross-linking protein alpha actinin and capped by Capz - thin filaments pointy ends terminate within A band - capped by tropomodulin - myosin-binding-protein C |
|
|
fatty acid
|
- transported to heart by lipoproteins
- major fuel for heart - triglycerides and glycogen stored as droplets in cytoplasm - enter cardiac muscle cell by passive diffusion or protein-mediated transport - glucose enters via a glucose transporters (GLUT) |
|
|
lactic acid
|
- also used by heart
- generated by skeletal muscle as energy source - convert back to pyruvic acid |
|
|
layers of connective tissue
|
- wrap around cardiac muscle
- endocardium - myocardium - epicardium |
|
|
endocardium
|
- simple squamous
- elastic fiber - subendocaridal layer |
|
|
myocardium
|
- heart muscle arranged in spiral layers
- thickest layer - contractile fibers - purkinje fibers |
|
|
epicardium
|
- mesothelium
- thin layer of CT |
|
|
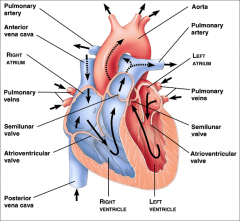
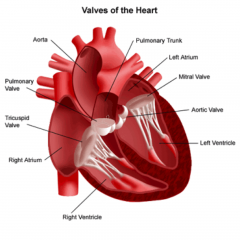
heart diagram
|
|
|
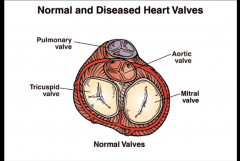
annulus fibrosis
|
- contains all the heart valves
- pulmonary valve - aortic valve - tricuspid valve - mitral valve |
|
|
endogenous action potentials
|
- generated at periodic intervals
|
|
|
intrinsic conduction system
|
- consist of non contractile cardiac cells specialized to initiate and distribute impulses throughout heart
- SA node - AV node - bundle of HIS - purkinje fibers |
|
|
action potential of pacemaker cells
|
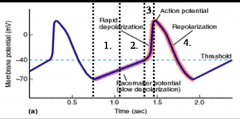
- auto rhythmic cell membranes show slow drift to threshold = pacemaker potential
- at rest = -55 - slow depolarization to threshold caused by a cyclical decrease in passive outward flux of K+ coupled with slow unchanging inward leak of Na+ - transient Ca (CaT) channels open along with voltage gated Na channels until threshold reached - voltage gated Na+ channels open - long lasting Ca channels (Ca L) open and cause plateau coupled with outward flow of K+ - K+ causes depolarization - Calcium permeability decreases |
|
|
impulse generating and conducting system
|
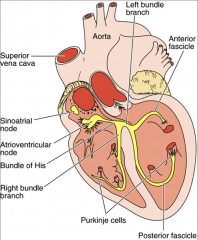
|
|
|
senatorial node (SA)
|
- located in right atrial wall just inferior to superior vena cava
- generates about 75 action potentials per minute - hearts main pacemaker - sinus rhythm |
|
|
atrioventricular node (AV)
|
- located in inferior portion of interaertrial septum
- from the SA node depolarization wave spreads to AV via internodal system - impulse delayed by 0.1 seconds - depolarizes about 50 times per second |
|
|
bundle of HIS
|
- atrioventricular bundle
- only electrical connection between atria and ventricles - right and left branches - depolarize about 30 times per second |
|
|
purkinje fibers
|
- modified muscle fibers with few myofibrils
- depolarize about 30 times per second - controls ventricles and papillary muscles - tighten chodae tenineae - open tricuspid and mitral valve |
|
|
contractile muscle fibers
|
- bulk of heart muscle
|
|
|
action potential of contractile cardiac cell
|
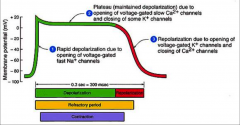
- rest membrane potential is about -90 due to Na/K ATPase pump, Na/Ca exchanger of inward rectifying K channel
- fast Na+ channel opens—3 gates - resting = m closed and d/j open - depolarization = m open and and d/j closed - Ca in slow at 25mV and all fast Na channels closed - K permeability decreased producing plateau phase - transient Cl- channel opens dropping potential to 20mV - K+ permeability increases with decreasing repolarization delayed rectifying channels with inactivation of Ca++ channels |
|
|
long refractory period
|
- period in which heart can't regenerate action potential
- can't go into tetany and summation - don't want contraction until blood has pumped through heart - can't start contraction until first contraction is complete - heart must be empty |
|
|
control of heart rhythm
|

- pacemaker generates wave of signals to contract
- signals are delayed getting to AV node - signals pass to heart apex - signals spread throughout ventricles |
|
|
heart beat
|
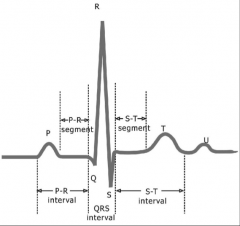
- P wave is depolarization of SA node through atria
- QRS is ventricular depolarization - covers atrial depolarization as well - T wave is ventricular repolarization |
|
|
myocardial contraction
|
- activated by a transient rise in cytosolic free calcium concentration to about 1 μM from about 0.1 μM
- bulk of this Ca required for activation of contraction originates from the sarcoplasmic reticulum (SR) - Ca influx through L-type Ca channels interacting with Ryr receptors - Na–Ca exchangers (NCX) making more minor contributions - Ryr receptor is a different isoform than in skeletal muscle - different type of DHPR in cardiac muscle |
|
|
heart controlled by nervous system
|
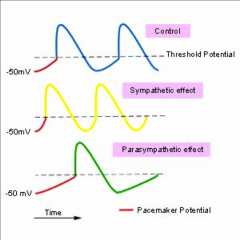
- sympathetic nervous system increases contraction
- parasympathetic nervous system decreases contraction - extrinsic control - fibers of autonomic nervous system modify intrinsic control - vagus nerve |
|
|
medulla
|
- cardiac center
- nucleus tractus solitarius (NTS) of the medulla receives sensory input from different systemic and central receptors - receives information from other brain regions |
|
|
cardioacceleratory center
|
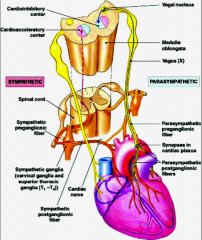
- sympathetic
- projects motor neurons in T1-T5 that synapse with neurons in cervical and upper thoracic sympathetic ganglia - from sympathetic ganglion fibers run to the heart - they innervate SA and AV node, heart muscle, and coronary arteries |
|
|
cardioinhibitory center
|
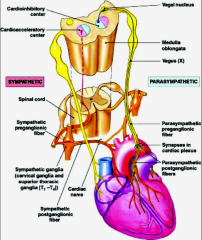
- parasympathetic
- sends impulse via vagus nerve - ganglia lie in heart wall and send fibers to SA and AV node |
|
|
cardiac cycle
|
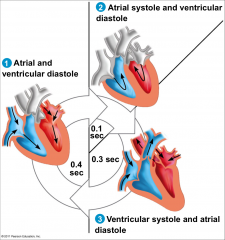
- movement of blood through heart
- mechanical events - blood flows from vena cava and pulmonary veins into atria and then into ventricle through tricuspid and bicuspid valve - brief period of atrial contraction forces all remaining blood in atria into ventricles - ventricular contractions pump blood into pulmonary artery and aorta through semilunar valve |

