![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
Adaptive immunity |
Develops naturally Pathogen invades body and elicits a primary or secondary immune response |
|
|
Passive immunity |
Provides immediate short-term protection (only transfer of Igs) Occurs naturally when Ig crosses the placenta or in breast milk. These antibodies protect the infant from pathogens that have not infected the infant before |
|
|
Immunization |
Introducing antigens into the body Inactivated bacterial toxins, killed pathogens, parts of pathogens, weakened pathogens and even gene-encoding microbial proteins |
|
|
First immunization |
1st occurred in 1796 Edward Jenner discovered that cowpox created adaptive immunity with smallpox. Smallpox was eradicated in 1970 Now have reduced polio, measles, and whooping cough |
|
|
Artificial passive immunity |
Antibodies from immune animal are injected into nonimmune animal ie: antivenin (from sheep and horses) works against snake venom ie: immunoglobulins injected for XLA |
|
|
Antibodies |
Products of many different clones of plasma cells Produced by animal after exposure to antigen |
|
|
Monoclonal antibodies (MAbs) |
From a single clone of B cells grown in culture Cells are altered to become immortal constantly producing antibodies Specific for one epitope Used in types of medical dx and tx (biomarkers) ie: home pregnancy test-detects chorionic gonadotropin (HCG) which is produced as soon as embryo implants in uterus |
|
|
Immune rejection |
Cells transferred from one person to another can be attached by immune defenses ie: blood groups |
|
|
Blood groups |
Antigens on red blood cells determine whether a person has blood type A, B, AB, or O (neither antigen) Antibodies to nonself blood types exist Serum sickness (chills fever shock and kidney malfunctioning) due to incompatible blood types |
|
|
MHC molecules |
Transmembrane glycoproteins that identify an individual from non-identical individuals Multiple alleles for each 12 MHC genes enabling presentation of antigen fragments that vary in shape and charge (non2 people will have same set except twins) Classes I: span membrane of every cell Clases II: restricted to macrophages and lymphocytes |
|
|
Transplants |
Increase risk of rejection of MHC molecules Try to match as closely as possible Treat leukemia, hemotological Lymphocytes in bone marrow transplants may cause donor tissue to be rejected Can use immunosuppressive drugs (but leave a person open to infection); radiation to reduce immune response in donor marrow, skin grafts) |
|
|
Humoral immune response |
Antibodies help neutralize or eliminate toxins and pathogens in the blood and lymph Includes a primary and secondary immune response enabled by memory cells |
|
|
Cell-mediated immune response |
Specialized T cells destroy infected host cells Includes a primary and secondary immune response enabled by memory cells |
|
|
Helper T cells (a response to nearly all antigens) |
Triggers both the humoral and cell-mediated immune response Initiate production of antibodies that neutralize pathogens and activate T cells that kill infected cells |
|
|
2 requirements of helper T cell |
1. A foreign molecule must bind specifically to the antigen receptor of the T cell 2. This antigen must be displayed on surface of antigen presenting cell (which can be dendritic, macrophage, or B cell) |
|
|
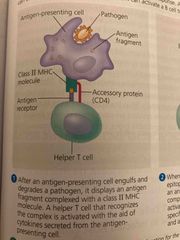
A helper T responding to a dendritic cell 1of 3 |
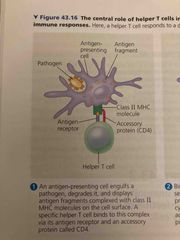
1. Antigen presenting cell (apc) engulfs pathogen, degrade it, and displays antigen fragment with MHC II molecule along with an accessory protein CD4 |
|
|
2. |
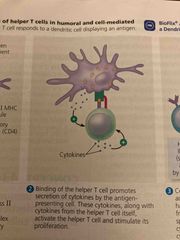
Binding of helper cells promoted release of cytokines from both cells. Apc secretes interleukin 1 and helpers secrete interleukin 2. These cytokines begin proliferation of T cell |
|
|
3. |

Cell proliferation produces clones of helper T cells. All clones have receptors for same antigen. Secrete cytokines to activate B cells and cytotoxic T cells |
|
|
The humerus response is characterized by.. |
Secretion of antibodies by B cells It begin with activation of B cells |
|
|
Activation of B cells |
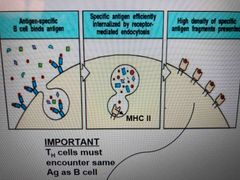
Involves helper Ts and proteins on surface of pathogens 1. Antigen binds on B cell and is taken in by receptor-mediated endocytosis. 2. Class II MHC protein of B cell then presents antigen fragment to helper T (this is critical to B cell activation) |
|
|
Activation of B cell in humoral immune response 3 parts |
After an apc engulfs and degrades pathogen it display antigen fragment complex (class II MHC and CD4 protein) T cell recognizes with help of cytokines from apc |
|
|
2. |

When B cell internalized with matching receptors to antigen, it displays a complex on surface A helper T cell recognizes and binds to B cell activating it |
|
|
3. |
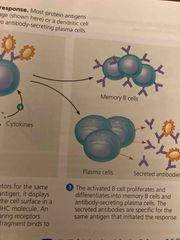
Activated B cell proliferates and differentiates into memory B cells and antibody-secreting plasma Antibodies are Specific for same antigen |
|
|
Activated B cell gives rise to thousands of identical plasma cells |
Produce and secrete antibodies (each secretes about 2000 antibodies every second of its 4-5 day life span) Most antigens recognized by B cells contain multiple epitope |
|
|
Antibody function |
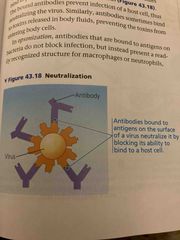
Do not kill pathogens but mark them for inactivation or destruction Can bind to viral surface proteins and prevent infection of host (neutralization) Will bind to toxins in body fluids and prevent them from entering body cells |
|
|
Opsonization |
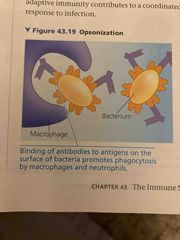
Antibodies bind to antigens on bacteria triggering phagocytosis by linking bacterial cells virus particles or other foreign substances |
|
|
Positive feedback btw innate and adaptive immunity |
Phagocytosis enables micro phages and dendritic cells to present antigens to stimulate helper T cells which in turn stimulate B cells whose antibodies contribute to phagocytosis |
|
|
Antigen-antibody complexes bind to a complement protein |
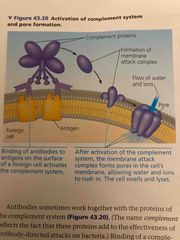
This triggers a cascade of complement protein activation These proteins increase effectiveness of antibody-directed attacks on bacteria Membrane attack complex-forms a pore in membrane of foreign cell leading to lysis |
|
|
Antibodies can cause death of infected body cells |
Virus uses cells biosynthetic machinery to produce viral proteins which can appear on cells surface Presence of antibody can recruit a natural killer cell which releases proteins that induce apoptosis |
|
|
Cytotoxic cell |

1. Binds to specific antigen presented by dendritic cell in lymph node. Binds with Class I MHC and CD8 protein. T cell recognizes and activated and clones 2. T cells leave lymph node to seek n destroy infected cells (cancer, transplanted). Secretes toxic proteins ( perforin and granzymes) to kill infected cells 3. Granzymes initiate apoptosis and then move on to other cells |
|
|
Perforin and granzymes |
P: disrupts membrane integrity G: apoptosis |
|
|
Visual aid |

A |
|
|
Allergies |
Hypersensitive or exaggerated responses to antigens called allergens |
|
|
How allergies happens |
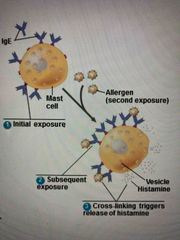
IgE antibodies produced by plasma cells after 1st exposure to an allergen. After clearance, IgE attached to receptors on mast cells Mast cells release histamine and other mediators that cause vascular changes (sneezing, watery eyes, runny nose) |
|
|
Anaphylactic shock |
A life threatening reaction produced by an Acute allergic response within seconds of ingested allergen exposure Widespread release of mast cell contents triggers dilation of blood vessels causing drop in bp and construction of bronchioles Bee venom, penicillin, peanuts Epinephrine reverses effects |
|
|
Autoimmune disease |
Immune system loses tolerance for self and turns against certain molecules of the body ie: lupus, type I diabetes, and MS |
|
|
Lupus |
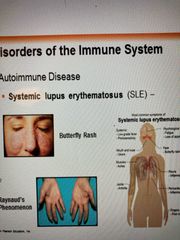
Immune system generates antibodies against various histones and dNA Characterized by skin rashes, fever, arthritis and kidney dysfunction |
|
|
Type I diabetes |
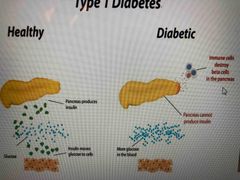
Insulin producing beta cells of the pancreas are target of autoimmune cytotoxic T cells |
|
|
Multiple sclerosis |

Most common chronic neurological disease T cells reactive against myelin infiltrate CNS and destroy myelin sheath Muscle paralysis |
|
|
Rheumatoid arthritis |

Inflammatory response of the capsule around joints .6% of US population Prevalence in women 2-3x |
|
|
Immunodeficiency dieseases |
Inborn: results from genetic or developmental defect in innate or adaptive defense Defects in development of immune cells or proteins (antibodies in X-linked BTK which prevent B cells from developing) Defects in complement system in proteins Functional lymphocytes are rare/absent (severe combined immuno or SCID) |
|
|
Acquired immunodeficiency |
Develops later in life due to exposure to chemical or biological agents AIDS Drugs that suppress immune system or fight autoimmune diseases Certain cancers suppress immune system (Hodgkins) |
|
|
Antigenic variation |
Pathogens are able to change epitope expression and prevent recognition(sleeping sickness, flu) |
|
|
Latency |
Some viruses remain in host in an inactive state Herpes: bc sensory neurons express relatively few MHC molecules, infected cells are inefficient at presenting viral antigens to lymphocytes |
|
|
HIV |
Infects helper T cells (attacks adaptive immune response) CD4 molecule is main receptor Impairs both humoral and cell-mediated immune response Lives in host despite immune response bc it had a high mutation rate that promotes latency (antigen variation) Over time abolishes adaptive immune response (susceptible to infections and cancers) |
|
|
Cancer and immunity |
Freq of certain cancers increases when adaptive immune is inactivated 15-20% of cancers involve viruses Immune system can act against viruses that cause cancer and cancer cells (hepatitis B) A vaccine was developed against human papilloma (HPV) assoc with cervical cancer |
|
|
Interferon- alpha (cytokines) |
Proteins that boost immune system Man-made versions such as interferon-alpha and interleukin 2 are used for melanomas and bone marrow donors (enhances stem cell production) Both drugs shrink stage III and IV melanomas in 10-20% of patients when used alone. May be combined with chemo |
|
|
Bacillus callmette-guerin vaccine |
bGM is related to tuberculosis Does not cause disease in humans but activated immune system (bladder cancer and melanoma) |

