![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
132 Cards in this Set
- Front
- Back
|
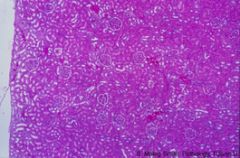
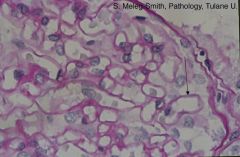
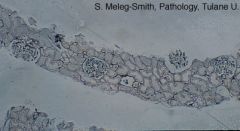
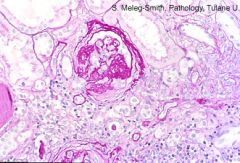
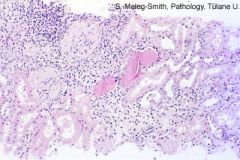
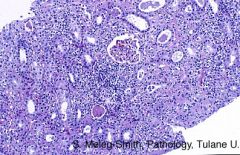
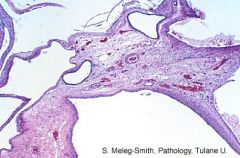
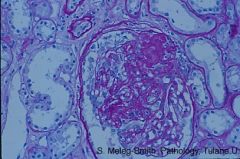
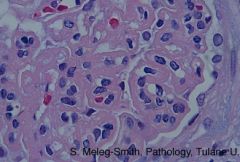
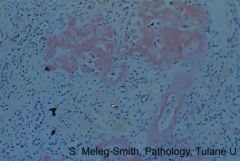
Low magnification of normal kidney cortex (HE)
|
|
|
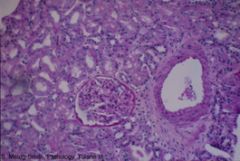
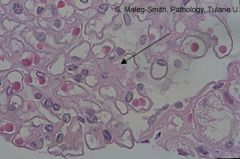
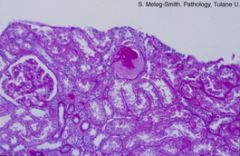
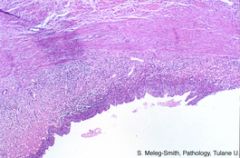
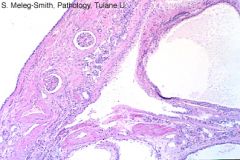
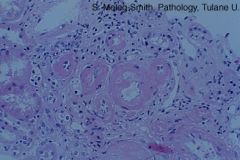
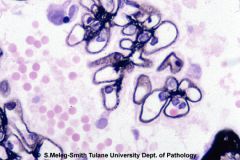
Normal kidney showing glomerulus, tubules and muscular artery (PAS). Interstitial stroma is only present surrounding the muscular artery.
|
|
|
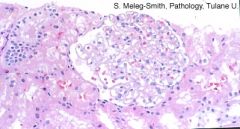
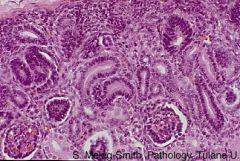
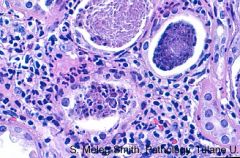
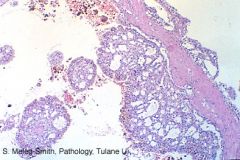
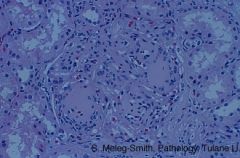
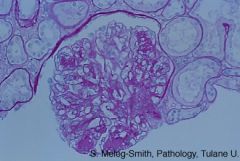
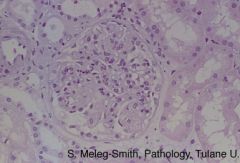
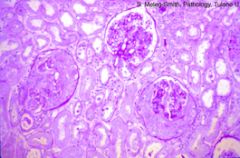
Normal glomerulus with patent (open) capillaries surrounded by tubules (H & E).
|
|
|
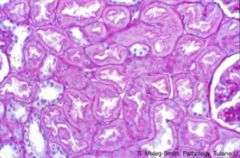
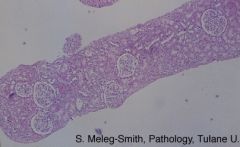
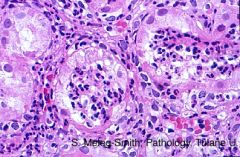
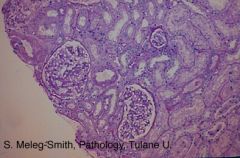
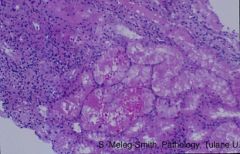
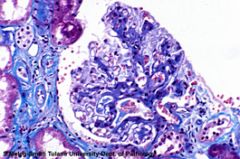
Normal kidney cortex with no apparent interstitial connective tissue between tubules (PAS).
|
|
|
Normal proximal tubules with slender basement membrane. Proximal tubules are lined by epithelium with brush border (center and right). Distal tubules have no brush border (left). (PAS)
|
|
|
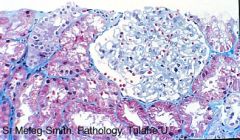
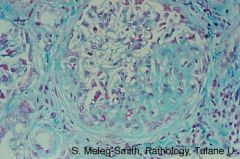
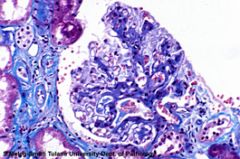
Normal glomerulus surrounded by tubules. Scant interstitium, stained blue, is visible in this trichrome preparation. In an H and E preparation, the interstitial tissue is normally not apparent.
|
|
|
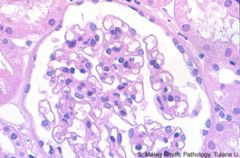
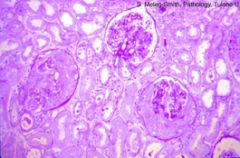
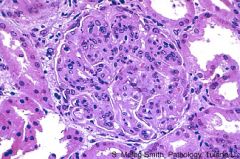
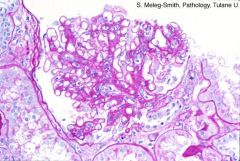
Normal glomerulus with patent (open) capillaries separated by mesangium (H & E). The urinary space (white) is surrounded by parietal epithelial cells that line Bowman's capsule.
|
|
|
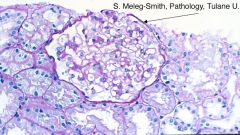
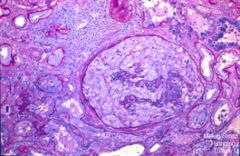
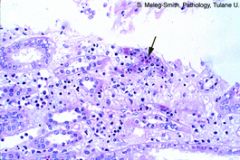
Bowman’s capsule (arrow) contains a normal glomerular tuft surrounded by Bowman’s space. The glomerulus is surrounded by tubules (PAS).
|
|
|
Capillary loops are surrounded by delicate basement membrane (arrow). Visceral epithelial cells (podocytes) are outside the loops (PAS stain).
|
|
|
Normal glomerulus: mesangium (arrow) is the amorphous eosinophilic tissue between the loops which are surrounded by GBM. (H & E)
|
|
|
Higher magnification of the nephrogenic zone of the kidney of a fetus at 13 weeks gestational age. Tubular structures lined by several layers of hyperchromatic epithelial cells are present (HE).
|
|

|
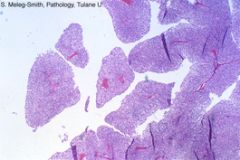
Kidney fetus of 13 weeks gestation. The nephrogenic zones shows solid areas of small blue cells (blastema). Stroma is present in the lower portion (HE).
|
|
|
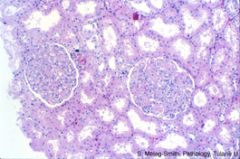
Needle biopsy of kidney: unremarkable glomeruli at low power. (H & E)
|
|
|
Needle biopsy shows normal renal cortex. (Jones)
|
|

|
Appearance of normal kidneys using computer assisted tomography (CT) scan at approximately mid-level of the kidneys. The kidneys are normal in size and a well-delineated cortex is easily visualized (the white area surrounding the inner dark area--medulla). Biopsy for diagnosis of medical diseases of the kidney should be obtained from the cortex.
|
|

|
Ultrasound appearance of normal kidney in sagittal view. The kidney is of normal size and normal echogenicity with an easily discernible normal width cortex. (Optional: US imaging is widely utilized in guiding the needle for kidney biopsy).
|
|
|
The glomerulus in the center of the field is replaced by global sclerosis. In contrast, the glomerulus on the left is normal (PAS)
|
|
|
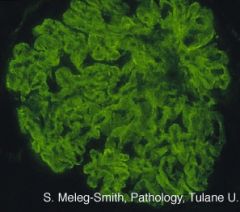
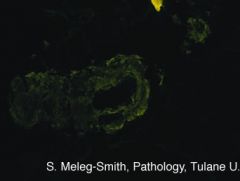
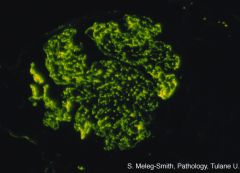
Granular deposits of IgG along the basement membrane stain intensely positive with FITC labelled antiserum.
Normal kidney does not contain Ig. When present, Ig's are part of immune complexes. Several renal diseases are immune-complex mediated. |
|
|
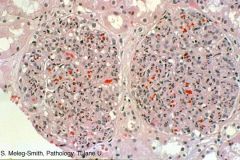
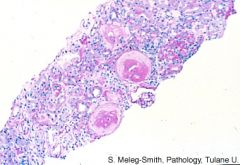
Diffuse Glomerulosclerosis -Two of three glomeruli surrounded by proliferation of parietal epithelial cells, i.e. crescents. (PAS)
|
|
|
Segmental sclerosis from 3 to 6 o’clock of the glomerulus. Interstitial fibrosis is also present. (Trichrome).
|
|
|
Global sclerosis - Glomerulus is hypercellular and lobulated. Bowman’s space is not apparent.
|
|

|
Reflux - Excretory urogram shows marked blunting of calices in a patient with hydronephrosis and hydroureter secondary to reflux.
|
|

|
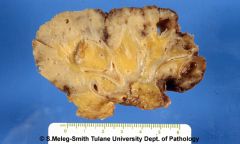
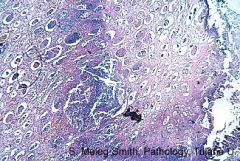
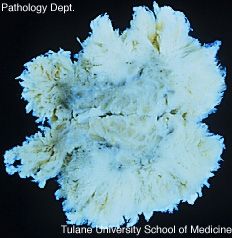
Reflux - The cut surface of the kidney is white with total loss of the normal architecture. The changes suggest a chronic inflammatory disease (formalin-fixed surgical specimen).
|
|
|
Reflux - The cut surface of the kidney is white with total loss of the normal architecture. The changes suggest a chronic inflammatory disease (formalin-fixed surgical specimen).
|
|
|
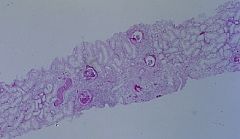
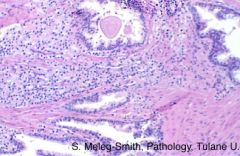
Reflux - The renal biopsy shows a patchy process. In the center of the field glomeruli look solid and tubules are not recognizable (PAS).
|
|
|
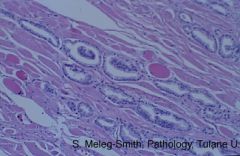
Reflux - The glomerulus in the center of the field shows severe periglomerular fibrosis and segmental fibrosis of the tuft. Focal tubular atrophy and interstitial fibrosis are seen, with mononuclear inflammatory infiltrate. These non-specific changes are observed in reflux nephropathy (PAS).
|
|

|
Acute Pyelonephritis - The nephrographic phase CT demonstrates a striate appearance of the cortex and medulla of the left kidney. This is characteristic for pyelonephritis.
|
|

|
Papillary Necrosis - The renal cortex is well preserved. The papilla (tip of the pyramid) is replaced by yellow necrosis (autopsy specimen).
|
|
|
Papillary Necrosis - The normal architecture is entirely lost. The necrotic papilla (on the right) is surrounded by a rim of inflammatory cells (H & E).
|
|
|
Xanthogranulomatous pyelonephritis - The interstitium is expanded by abundant mononuclear inflammatory cells. Glomeruli show global or segmental sclerosis.
|
|

|
Xanthogranulomatous pyelonephritis - The normal renal architecture is replaced by diffuse yellowish tissue that infiltrates the surrounding adipose tissue.
|
|

|
Acute pyelonephritis due to Lithiasis - Cortico-medullary phase CT shows dilated calices (hydronephrosis) and a large calculus. There is also loss of parenchymal thickness. Note striation and fluid in the perirenal space, and marked thickening of the posterior renal fascia, findings suggestive of a perirenal abscess. In view of the infection, this is a case of pyonephrosis.
|
|

|
Hydronephrosis - Genitourinary system obtained at autopsy. The right kidney shows very severe dilatation of the pelvis.
|
|
|
Hydronephrosis - Kidneys are enlarged and the parenchyma is reduced to a thin membrane by the severe dilatation of pelvis and calyx.
|
|
|
Hydronephrosis - Two glomeruli are replaced by global sclerosis. Interstitial fibrosis and inflammation are observed. Tubules in the center of the field are distended by proteinaceous material (PAS).
|
|
|
Acute Pyelonephritis - Inflammation and fibrosis are observed under the urothelium covering pelvis.
|
|
|
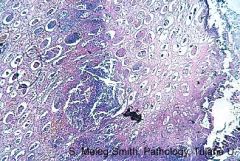
Acute Pyelonephritis - The interstitium is infiltrated by abundant PMNs. Tubules are distended by inflammatory cells and granular necrotic material (H & E)
|
|
|
Acute Pyelonephritis - Tubules contain abundant PMNs in the lumen. (H & E)
|
|
|
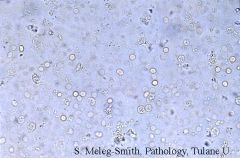
Granular casts. --> ATN (Microscopic examination of urinary sediment)
|
|
|
Acute Pyelonephritis - Severe interstitial inflammatory infiltrate is observed. The glomerulus is unremarkable. (H & E)
|
|
|
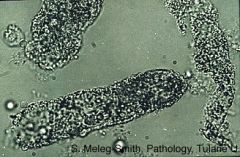
"glitter cell"
|
Neutrophil containing cytoplasmic granules exhibiting Brownian motion.
|
|
|
Papillary Necrosis - The normal architecture is entirely lost. The necrotic papilla (on the right) is surrounded by a rim of inflammatory cells (H & E).
|
|
|
Microscopic Hematuria - Microscopic examination shows that abundant red blood cells and occasional PMN are present in the urinary sediment.
|
|

|
Papillary Necrosis - Late nephrographic-excretory phase spiral CT of the left kidney with an area of non-staining and destruction in the tip of the pyramid of the posterior mid calyceal group, with a small projection of remaining tissue and contrast material pooling in the calyx. The appearance is characteristic of papillary necrosis.
|
|
|
Xanthogranulomatous Pyelonephritis - The inflammatory infiltrate contains abundant macrophages with vacuolated cytoplasm (xanthoma cells).
|
|
|
Xanthogranulomatous Pyelonephritis - The interstitium is expanded by abundant mononuclear inflammatory cells. Glomeruli show global or segmental sclerosis. (H & E)
|
|
|
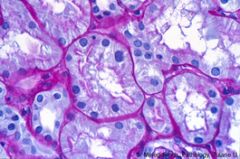
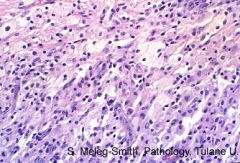
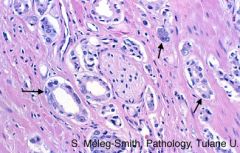
Renal Cell Carcinoma - The most frequent microscopic presentation of renal cell carcinoma is clear cell carcinoma. As the name implies, the cytoplasm of the cells is pale (HE).
|
|

|
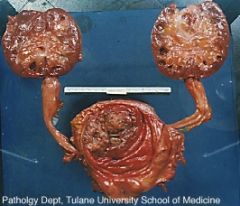
Wilms tumor - Spiral CT cut through the mid portion of both kidneys during the cortico-medullary phase: normal though slightly angulated left kidney. An approximately 8 by 6.5 cm slightly heterogeneously staining mass originates from the anterior circumference of the mid pole of the right kidney, with "spaghetti" vessels; the appearance is characteristic for a Wilm's tumor . The posterior half of the right kidney shows normal cortico medullary enhancement.
|
|
|
Cystic dysplasia - The nephrectomy specimen has been fixed in formalin and bisected. Abundant cysts replace the normal architecture.
|
|

|
Autosomal recessive polycystic kidney disease - The renal parenchyma is replaced by uniform, small, linear cysts that run perpendicular to the capsule.
|
|
|
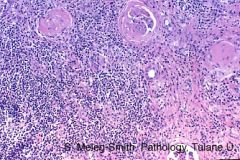
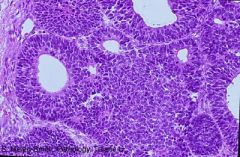
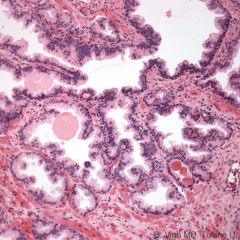
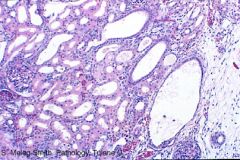
Wilm's Tumor - The neoplasia is triphasic: eosinophilic stroma, solid proliferation of small blue cells (blastema) and formation of epithelial tubular structures (HE).
|
|
|
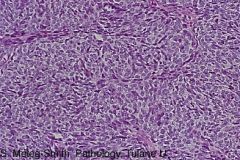
Wilm's Tumor - Blastema: diffuse proliferation of small blue cells, i.e., cells with large blue nuclei and scant cytoplasm (HE).
|
|
|
Wilm's Tumor histologic features
|
Tri-phasic nephrogenic process with epithelial, stromal and blastemic cell types.
A tumor that is reminiscent of fetal kidney |
|

|
Urothelial Carcinoma - Bladder - An arterial phase CT through the pelvis further highlights the papillary aspect of the large bladder tumor arising from the trigone and floor of the bladder. Note that the right anterior and left lateral bladder walls are not involved and are not thickened.
|
|
|
Urothelial Carcinoma - Bladder - Urinary tract obtained at autopsy; the bladder has been opened and shows multiple nodular masses that have replaced most of the normal mucosa. Both ureters are dilated and kidneys show dilated calix (hydronephrosis).
|
|
|
Urothelial Carcinoma - Bladder - Transverse sections of papillary tumor, ie, composed by finger-like projections. The central core shows congested blood vessels.
|
|
|
Urothelial Carcinoma - Bladder - This papillary mass was attached to the mucosa of the bladder by the pedicle, partially present to the left (surgical resection)
|
|
|
Carcinoma of the Prostate - Normal prostatic glands are separated by proliferation of poorly-differentiated glands in the center of the field.
|
|
|
Carcinoma of the Prostate - Skeletal muscle is infiltrated by well-differentiated malignant glands.
|
|
|
Normal prostate: glands are lined by pseudostratified epithelium. Glands are separated by fibromuscular stroma.
|
|
|
Prostatic Adenocarcinoma - Perineural invasion; well-differentiated malignant glands are present in the perineural spaces. Note the prominent nucleoli within malignant glands (arrows) HE.
|
|
|
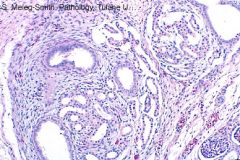
Areas of normal kidney parenchyma on the left alternate with cystic structures on the right (HE).
|
|
|
Renal Dysplasia - The cystic structures are surrounded by immature mesenchyma. (H and E).
|
|

|
Renal Dysplasia - A spiral CT cut on the same patient (shown in 3C) 3 cm lower confirms a normal right kidney. There is minimal residual parenchyma near the hilum of the left kidney, a slightly enhanced septum in the mid segment of the mid pole of the left kidney, and large septate cysts. The appearance is characteristic of a cystic dysplastic kidney.
|
|

|
Renal Dysplasia - A spiral CT cut (late parenchymal-early excretory phase) demonstrates a normal kidney on the right side. On the left there is only a rim of normally enhancing renal tissue with a septate large cyst occupying the posterior circumference.
|
|
|
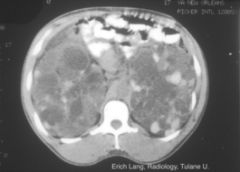
Autosomal Dominant Polycystic Kidney Disease (ADPKD) - Nephrographic phase computed tomogram: severe enlargement of both kidneys by innumerable cysts of variable size. The appearance is characteristic for polycystic disease of the kidney. Some of these cyst contain high-density material, attributable to hemorrhage into the cysts.
|
|

|
Autosomal Dominant Polycystic Kidney Disease (ADPKD) -A late phase arteriogram demonstrates innumerable non-enhancing cystic masses throughout the cortex and cortico medullary junction of this enlarged kidney. The "Swiss cheese" appearance is characteristic for adult polycystic disease.
|
|

|
Autosomal Dominant Polycystic Kidney Disease (ADPKD) - An excretory phase CT demonstrates bilateral displacement of calices by non-enhancing cysts. Note one cystic lesion in the left kidney anteriorly, and one in the right kidney laterally, with higher density attributable to hemorrhage into a multilocular cyst.
|
|

|
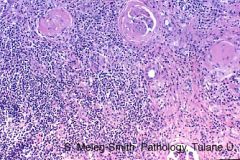
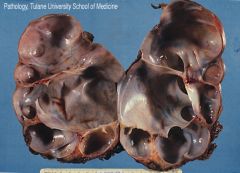
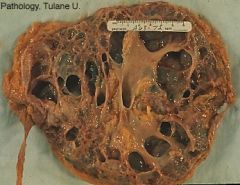
Autosomal Dominant Polycystic Kidney Disease (ADPKD) - Enlarged kidneys with abundant hemorrhagic cysts.
|
|
|
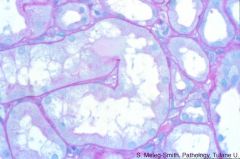
Autosomal Dominant Polycystic Kidney Disease (ADPKD) - The normal renal architecture is replaced by cysts of various sizes.
|
|
|
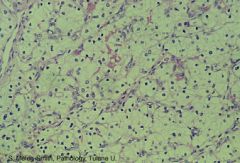
Autosomal Dominant Polycystic Kidney Disease (ADPKD) - Remnants of kidney parenchyma are compressed by cysts
|
|
|
Autosomal Dominant Polycystic Kidney Disease (ADPKD) - Proliferation of the epithelial lining of cyst
|
|

|
Simple Cyst - Normal kidney parenchyma surrounds a 5cm cyst .
|
|

|
Benign renal cyst - A cortico-medullary phase CT demonstrates a spherical cortical mass which fails to enhance. The wall is pencil thin. Delineation from the staining parenchyma is sharp. The findings are characteristic of a benign renal cyst.
|
|
|
Nephrotic Syndrome
|
Nephrotic Syndrome (NS) is defined as the excretion of more than 3.5 gm protein/24 hours/1.73m2 BSA usually, associated with hypoalbuminemia, hypercholesterolemia, and edema. The patients" urine may also show oval fat bodies, coarse granular casts, and microscopic hematuria; however, the heavy proteinuria is the distinguishing feature. A careful history and physical examination, as well as a variety of laboratory and serologic studies can determine if the disease is primary or systemic. The evaluation of a patient with more than 3.5 gm/24 hours is the same whether or not edema, high cholesterol, or hypoalbuminemia is present.
|
|
|
Primary Nephrotic Syndrome
|
Primary Nephrotic Syndrome indicates that the nephrotic syndrome and underlying glomerular disease are the main (or only) clinical presentation. Diagnosis is by histopathology.
eg: - Minimal change disease (MCD) - Focal segmental glomerulosclerosis (FSGS) - Membranous glomerulopathy (MGN) (idiopathic) - Membranoproliferative GN (MPGN) (idiopathic)(can also present as nephritic syndrome) |
|
|
Systemic Nephrotic Syndrome
|
Systemic Nephrotic Syndrome indicates that the kidney, and specifically the glomerulus, is one of several organ system involved simultaneously by a disorder. Consequently, symptoms from non-renal systems will be present and point to a clinical diagnosis.
Caused by: - Diabetes mellitus - Amyloidosis and multiple myeloma - Systemic lupus erythematosus (WHO class 5) - Membranous glomerulopathy (infectious diseases) - Membranoproliferative GN (infectious diseases) |
|
|
Nephritic syndrome
|
Nephritic syndrome is usually characterized by the relatively sudden onset of hematuria with RBC casts and poteinuria. This is accompanied clinically by variable degrees of salt and water retention, circulatory congestion, hypertension, and a reduced glomerular filtration rate. The presentation can be quite sudden and associated with acute renal failure. A simplified classification of the nephritic disorders is based not only on primary or systemic forms, but on the serum complement levels.
Serum complement levels may be LOW or NORMAL - Hematuria with RBC casts and proteinuria - GFR reduced due to glomerulonephritis (-itis = inflammation) - Reduced GFR --> salt and water retention --> HTN - Imaging is non-contributory to diagnosis, only necessary for biopsy |
|
|
Primary Nephritic Syndrome
|
Primary Nephritic Syndrome indicates that the glomerular disease is the main (or only) clinical presentation. Diagnosis is by histopathology.
Low Serum Complement: - Post-infectious (Post-streptococcal) GN - Membranoproliferative GN (idiopathic)(can also present as nephrotic syndrome) Normal Serum Complement: - IgA Nephropathy - Hereditary Nephritis (Alport syndrome) - Crescentic Rapidly progressive ANCA positive GN |
|
|
Systemic Nephritic Syndrome
|
Systemic Nephritic Syndrome indicates that the kidney, and specifically the glomerulus, is one of several organ system involved simultaneously by a disorder.
Low Serum Complement: - Infectious endocarditis - Systemic lupus erythematosus (WHO class 3, WHO class 4) Normal Serum Complement: - Anti-basement membrane disease (Goodpasture's disease) - Systemic vasculitis, ANCA positive - Thrombotic microangiopathy |
|
|
Acute Renal Failure (ARF)
|
Acute Renal Failure is characterized by Azotemia developing in a short period of time: i.e., days or a few weeks. It may be accompanied by hematuria and proteinuria.
|
|
|
"Pre-renal" Acute Renal Failure (ARF)
|
Acute renal failure is pre-renal when the kidney does not have intrinsic pathology but is reacting to an external cause; i.e. dehydration
True decreased renal perfusion: - hypovolemia due to fluid losses, GI bleeding - Decreased "Effective" Circulating Volume >> Decreased renal perfusion stimulates RAA system and leads to dysfunction/necrosis of tubular epithelium - Creatinine increases rapidly, over a few days - Oliguria/anuri - Assessment: history of medications, especially divretics, NSAIDs and ACEI - Associated with dehydration, shock, i.e. volume depletion and hypoperfusion states - Treatment of pre-renal problem corrects the acute renal failure - Excellent prognosis; no persistent renal damage - Renal biopsy only if no response to therapy, to rule out other diagnosis |
|
|
"Renal" Acute Renal Failure (ARF)
|
Acute renal failure is "renal" when a severe acute kidney disease is the cause of the azotemia. It can be a disease off any of the histologic components of thee kidney: glomerulus, tubules, interstitium, vessels
- Acute Glomerular diseases - Acute Tubulointerstitial diseases - Acute Vascular diseases |
|
|
Post-renal Acute Renal Failure (ARF)
|
Acute renal failure is post-renal when the kidney is essentially normal but there is extrarenal interference with the outflow: tumor, lithiasis, etc
- Obstruction |
|
|
Chronic renal failure (CRF)
|
Chronic renal failure is characterized by azotemia developing over a long period or time, i.e., months. It is the result of diseases affecting the kidney
|
|
|
Thrombotic Microangiopathy
|
Thrombotic Microangiopathy (TMA or MAHA)
Nephritic syndrome or acute renal failure accompanied by hemolytic anemia, hemorrhages, and purpura Has multiple clinical presentations and names: - with predominantly neurologic symptoms: thrombotic thrombocytopenic purpura (TTP) - with diarrhea: hemolytic uremic syndrome (HUS) - as complication of hypertension: malignant hypertension - as complication of pregnancy: eclampsia Most frequent presentations are TTP & HUS Many cases respond to treatment Renal biopsy confirms the diagnosis Also referred to as micro-angiopathic hemolytic anemia (MAHA) |
|
|
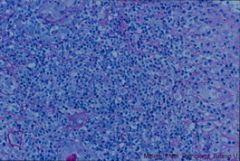
Minimal Change Disease (MCD) - Unremarkable glomeruli surrounded by tubules with no pathologic change. (H & E)
- Most frequent cause of nephrotic syndrome in children - Represents 10-15% cases of nephrotic syndrome in adults - Sudden onset of severe nephrotic syndrome: with hypoalbuminemia, hyper-cholesterolemia, normal BP, normal GFR - UA: 4+ protein, oval fat bodies, hematuria in 20% cases - Most cases are idiopathic - Frequently, especially in children, responds to treatment and has good prognosis - Final diagnosis: by renal biopsy |
|
|
FSGS (Focal Segmental Glomerulosclerosis) - Segmental glomerulosclerosis from 12 to 2 o’clock (PAS)
- Nephrotic syndrome frequently accompanied by HTN and reduction in GFR - Occurs in all age groups - Most frequent cause of nephrotic syndrome in African-Americans - Usually has poor prognosis, despite treatment - U/A: 75% cases> 3 gm/d protein, 75% cases have hematuria - Frequently idiopathic; can be associated with IV drug abuse, reflux nephropathy, and AIDS - Digonosis can only be made by biopsy |
|
|
Diabetic nephropathy - Arterioles are severely hyalinized and thickened. (H & E)
|
|
|
Diabetic nephropathy - Glomerulus with intense increase in mesangial matrix with formation of acellular nodules. (H & E)
|
|
|
Severe tubular damage with dilatation in HIV-Associated Nephropathy - Tubules show vacuolization and disruption of the cytoplasm. (H& E)
|
|
|
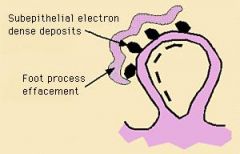
Membranous Glomerulopathy - The basement membrane around the capillary loops appears severely thickened. (H & E)
SUB-EPITHELIAL electron-dense deposits |
|
|
Membranous Glomerulopathy - Capillary loops are surrounded by GBM with "spikes": perpendicular out-growths (Jones).
|
|
|
Diabetic Nephropathy - Glomerulus with intense increase in mesangial matrix with formation of acellular nodules. (PAS)
|
|
|
Diabetic Nephropathy - The glomerulus shows increase in mesangial matrix; (Trichrome)
|
|
|
Amyloidosis - Congo Red shows positive material in glomeruli and blood vessels.
Amyloid fibrils appear green under polarized light. |
|
|
Amyloidosis - The normal glomerular architecture is replaced by increased mesangium with formation of acellular nodules. ( H & E)
|
|
|
Amyloidosis - The wall of the arteriole is fluorescent when incubated with FITC antiserum to lambda light chain.
|
|
|
Post-Infectious Glomerulonephritis - Hypercellular glomeruli with abundant PMNs. Capillary lumens are not apparent and there is loss of Bowman’s space.
|
|
|
WHO Kidney Classification (1-5)
|
Kidneys:
1: Normal 2: Mesangial GN 3: Focal proliferative GN 4: Diffuse proliferative GN 5: Membranous glomerulopathy |
|
|
Post-Infectious Glomerulonephritis - Intensely positive granular deposits of IgG along the capillary loops.
|
|
|
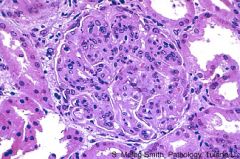
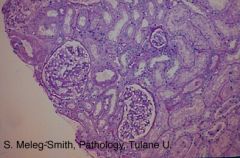
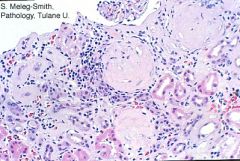
MPGN (Membranoproliferative GN) - Glomerulus is hypercellular and lobulated. Bowman’s space is not apparent.
- MPGN involves *mesangium* - (in contrast, Membranous GN does NOT) |
|
|
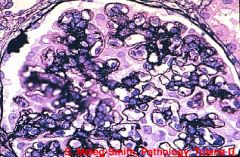
MPGN - Silver stain shows capillary loops surrounded by double basement membrane.
|
|
|
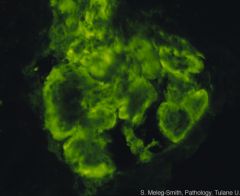
MPGN - Confluent granular deposits of complement along the basement membrane which has been displaced to the periphery of the glomerulus.
|
|

|
SLE:
- Low levels of circulating serum complement - Sub-endothelial and mesangial electron dense deposits - Intracytoplasmic tubloreticular bodies |
|
|
SLE:
- Lobulated hypercellular glomerulus with few patent capillary loops. - Capillary loops surrounded by severely thickened GBM - Almost complete loss of Bowman’s space. - Segmental necrosis of the glomerulus - IF shows: IgG, IgM, IgA, complement (full house) |
|
|
Normal - Unremarkable glomeruli surrounded by tubules with no pathologic change.
|
|
|
SLE - EM: Electron-dense deposits are observed in the mesangium (left arrow). Deposits are also observed in the inside of the capillary loop (subendothelial, middle arrow) and on the outside of the GBM (subepithelial, right arrow).
|
|
|
Infectious Endocarditis
|
Systemic nephritic syndrome, low complement
- Nephritic syndrome in patient with fever and heart murmur - Low levels of circulating complement - Nephritic syndrome resolves with appropriate antibiotic therapy - hypercellular glomeruli - granular IgG and complement along GBM - large electron dense deposits along the outside of the GBM |
|
|
IgA Nephropathy
|
Primary Nephritic syndrome, Normal complement
- Most frequent GN in Native Americans; very rare in African-Americans; low incidence in US caucasians. - Initial clinical presentation is hematuria and frequently follows immediately after an upper respiratory viral illness - Hematuria can be gross and recurrent or persistently microscopic - Proteinuria varies from mild to severe - Designated Henoch-Schonlein purpura syndrome when accompanied by purpura, arthralgia, and abdominal pain - Normal serum complement - Diagnosis by renal biopsy - No well defined therapy - Prognosis varies and progressive renal insufficiency over several decades can be seen. |
|
|
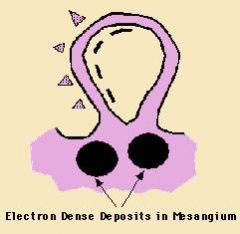
IgA Nephropathy - MESANGIAL electron dense deposits
|
|
|
IgA Nephropathy
or SLE [WHO class 2] - The glomerulus shows increase in mesangial matrix |
|
|
IgA Nephropathy - The glomerulus shows minimal increase in cellularity but severe expansion of the mesangium .
|
|
|
Alport's Disease
|
Primary Nephritic Syndrome, normal complement
X-linked: a5 of collagen IV Autosomal: a3 or a4 of collagen IV - Rare familiar disease - Hematuria, mild proteinuria, and normal serum complement - More common and severe in males who develop renal failure in early adulthood - Prognosis is variable in females - Nerve deafness and ocular disorders may occur - Diagnosis is made by renal biopsy ** Absence of Ig deposits |
|
|
Rapidly Progressive GN, ANCA-associated - Two of three glomeruli surrounded by proliferation of parietal epithelial cells, i.e. crescents.
|
|
|
Rapidly Progressive GN, ANCA-associated - The glomerulus is compressed by a severe proliferation of epithelial cells: cellular crescent.
|
|
|
Goodpasture's Disease (Anti-GBM Disease)
|
Goodpasture's Disease (Anti-GBM Disease)
(Systemic Nephritic syndrome, normal complement) - crescentic GN - Linear pattern of IgG deposition along GBM - Fibrin in crescents - antibodies against a3 of collagen IV of GBM - Typically presents with hemoptysis and hematuria - Normal serum complement levels - Diagnosis depends on demonstrating anti-GBM Ab in serum or tissue - Prognosis is poor despite aggressive treatment with steroids and plasma pheresis |
|
|
Systemic Vasculitis
|
Systemic Vasculitis
- Glomeruli with crescents, fibrin in crescents - Vasculitis in multiple organs, which includes the glomeruli - T-cell mediated injury - Multiorgan symptoms: polyarteritis nodosa, Wegener' s granulomatosis, and hyper-sensitivity angiitis - Vasculitis is focal patchy disease, which is seldom represented in a biopsy - Nephritic syndrome progresses to renal failure in months, weeks, or days, i.e. acute renal failure - Progression to uremia is rapid unless diagnosed and treated - Serologic marker is ANCA (anti-neutrophil cytoplasmic antigen) - Normal serum complement - Despite aggressive treatment, prognosis is poor in most cases - Renal biopsy confirms crescentic GN |
|
|
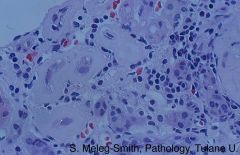
Thrombotic Microangiopathy - The afferent arteriole and a capillary loop are occupied by eosinophilic fibrin thrombi.
- Endothelial damage leads to aggregation of platelets followed by thrombocytopenia - Microthromi contain fibrin - Fibrin filaments damage RBC, causing hemolysis |
|
|
Acute Tubular Necrosis (ATN)
|
Acute Tubular Necrosis (ATN)
*** UA: "dirty brown" granular casts *** - Associated with renal ischemia or exposure to toxic substances - Urine Na> 20Meg | L, Fe Na>2% - Most frequent toxins: radiocontrast dye, myoglobin ( rhabdomyolisis ) aminoglycosides and other antibiotics |
|
|
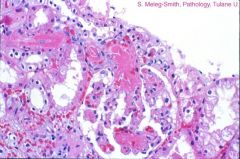
ATN - Severely dilated tubules with focal loss of epithelium
|
|
|
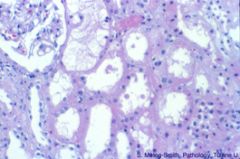
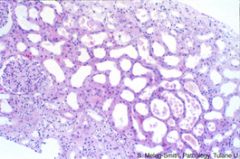
ATN - Tubules are severely dilated and some contain desquamated cells
|
|
|
ATN - Tubules are severely dilated and some contain desquamated cells
|
|
|
Acute Interstitial Nephritis
Tubules are separated by interstitial edema that contains abundant inflammatory cells with frequent eosinophils. <-- Allergic reaction - Glomeruli not affected - Creatinine increases rapidly-over a few days - Common disease - Most frequent cause: iatrogenic, especially nonsteroidal anti-inflammatory drugs and antibiotics - Can be associated with skin rash - Good prognosis if offending agent stopped |
|
|
Chronic Renal Failure - Loss of normal architecture (PAS)
|
|
|
Chronic Renal Failure - All three glomeruli are replaced by global sclerosis. Interstitial fibrosis and mononuclear inflammatory infiltrate surround atrophic tubules
|
|
|
Chronic Renal Failure - Atrophic tubules (left) surrounded by severly thickened basement membrane. Interstitial inflammatory infiltrate (right)
|
|
|
Acute Renal Graft Rejection - Tubules destroyed by severe mononuclear inflammatory infiltrate (PAS)
|
|
|
Acute Renal Graft Rejection - Tubulitis: PAS stain highlights the basement membrane of the tubule, invaded by mononuclear inflammatory cells (lymphocytes)
|
|
|
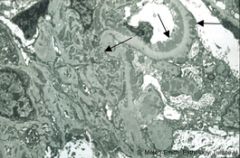
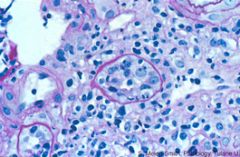
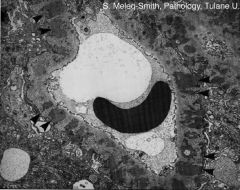
Membranous Glomerulopathy - The basement membrane is severely thickened with abundant SUB-EPithelial electron-dense deposits. The deposits are initially on the outside of the GBM which grows to flank the deposits. These projections (not shown here) of the GBM correspond to the spikes seen by silver stains.
This is also seen in Post-streptococcal GN |
|
|
Membranous Glomerulopathy - Capillary loop contains red blood cells in the lumen. The basement membrane is severely thickened with abundant electron-dense deposits shown by arrowheads. The deposits were originally on the outside of the GBM which now has grown to flank the deposits. These projections of the GBM correspond to the spikes seen by silver stains.
This is also seen in Post-streptococcal GN |
|
|
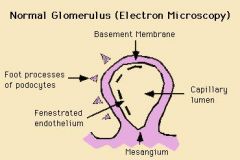
Normal EM - Capillary loops are surrounded by GBM, with fenestrated (interrupted) endothelium on the inside and foot processes from podocytes (visceral epithelial cells) on the outside.
|

