![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
101 Cards in this Set
- Front
- Back
|
1. the renal system receives ____% of cardiac output
2. ____% of diseases involve the kidney in some fashion |
1. 20-25%
2. 40% |
|
|
fxns of the renal system
|
conservation
- water and electrolytes - acid-base regulation excretion - nitrogenous wastes - metabolites endocrine - renin-angiotensin-aldosterone - erythropoietin - thrombopoietin - calcitrol "D3" |
|
|
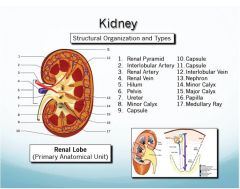
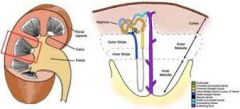
components of the renal system & their function
|
Kidney:
- Capsule : organ strx - Cortex : filtration, modification, endocrine - Corticomedullary Jxn : modification, concentration - Medulla : modification, concentration - Papilla (Renal Crest) : transport - Pelvis : transport Ureters/Urethra - transport Urinary Bladder - storage - controlled release |
|
|
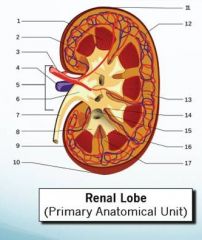
the anatomic unit of the kidney is the ________
what is it composed of |
lobe
composed of - cone shaped wedge of tissue renal (pyramid) in the medulla - the cortex external to it - one or more pyramids make up the medulla - contains visible stripes from the parallel "straight" segments of the nephrons |
|
|
who has unilobar kidneys?
multilobar? |
unilobar
- rodents - cats multilobar (completely fused so appears as unilobar externally) - dogs - humans - horses - small ruminants multilobar (incompletely fused) - swine - large ruminants |
|
|
The ___A_____ delivers urine via the "area cribrosa" to the ____B_____
|
A. renal crest (unilobar) or papilla (multilobar)
B. renal pelvis (unilobar) or minor/major calyx (multilobar) |
|
|
|
|
|
describe the kidney capsule
|
very little CT in kidney (except at intersections of the lobe in multilobar kidneys)
the strx is provided by the combination of the veins, arteries, and tubules that are enclosed in the capsule capsule provides an inelastic envelope that lacks CT connections to the renal cortex (except in the horse) |
|
|
_______ provides an inelastic envelope that lacks CT connections to the renal cortex.
What spp is the exception to this rule? |
Capsule
horse |
|
|
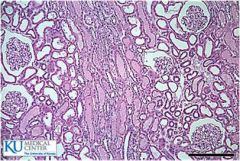
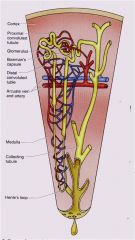
describe the cortex/ medulla
|
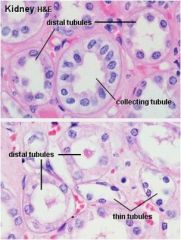
cortex includes
- renal corpuscles - convoluted tubules - collecting ducts medulla - renal tubules - collecting ducts |
|
|
describe the corticomedullary jxn
|
corticomedullary jxn is not a sharp demarcation but can provide a rough idea proportions b/w the 2
the arcuate arteries follow the jxn |
|
|
describe medullar rays
|
parallel streaks that radiate through the medulla and cortex
composed of straight tubules (loop of henle) and collecting ducts |
|
|
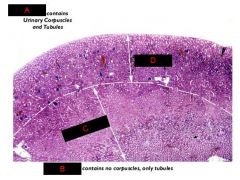
_____ contains no corpuscles, only tubules
|
medulla
|
|
|
_____ contains urinary corpuscles and tubules
|
cortex
|
|
|
describe the pelvis
|
the upper "expanded" cup-shaped end the beginning of the ureter
large collecting ducts empty inot the pelvis with urine being collected and drained by the ureter the strx of the pelvis matches the overall strx of the kidney (whether unilobar or multilobar) mucous glands are present in the horse is the reason for cloudy urine |
|
|
why anatomic abnormality is the reasong that horses have cloudy urine
|
they have mucous glands in the pelvis
|
|
|
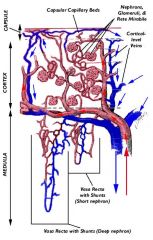
the vascular system of the kidney is a(n) _________ system
|
end arterial
|
|
|
describe the progression of blood through the kidney
|
- renal artery
- interlobar artery - arcuate artery - interlobular artery - intralobular artery - afferent arteriole - renal corpuscle (glomerulus) - efferent arteriole - peritubular plexes (vesta recta/ rete mirable) - intralobular vein - interlobular vein - renal vein |
|
|
Describe rete mirabile
|
Complex network of post glomerular capillaries (second capillary system)
Covers the nephron but is most dense in the cortex around the glomeruli |
|
|
Describe the vasa recta
|
Capillary loops of the rete mirabile
send straighter segments deeply into the medulla and surround the straight tubules (loop of henle) play a critical role in maintaining the interstitial Na+ gradient in the medulla |
|
|
_______ is the basic functional unit of the kidney
|
nephron
|
|
|
________ functions to filter blood to produce a large volume of plasma filtrate then to modify and concentrate prior to excretion
|
nephron
|
|
|
1. Is modification active or passive?
2.Is concentration active or passive? |
Modification and concentration are both an active and passive process and depend on the vascular system and intersititium
|
|
|
What is the function of the nephron?
|
Filters blood to produce a large volume of plasma filtrate
Then modifies and concentrates this prior to excretion |
|
|
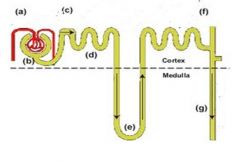
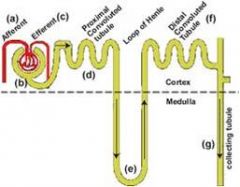
Components of the nephron and their fxns
|
Renal corpuscle
- Filtration Proximal convoluted tubule - Resorption (water, glucose, protein, Na Loop of Henle - Countercurrent ion exchange Convoluted tubule - Active Na Transport |
|
|
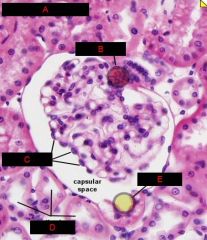
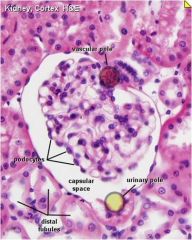
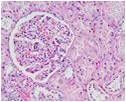
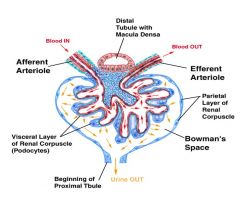
Renal Corpuscle (glomerulus)
What is it and what does it do? |
Complex strx uniquely designed to filter blood
Pressure sensitive mechanical filtration Some electrostatic selective exclusion of proteins |
|
|
Components of the Renal Corpuscle (glomerulus)
|
Afferent & efferent arterioles
Visceral and parietal epithelium Bowman’s capsule and space Mesangium |
|
|
What forms the filtration slits that both physically (pressure) and electrostatically produce the glomerular filtrate that empties into bowman’s space which is continuous with the PCT
|
Combination of the basement membrane and podocyte foot processes
|
|
|
What is the basis of the fxn of the glomerulus
|
The unique strx of the capillary knot
|
|
|
Describe the glomerulus strx (cellular description)
|
Capillary knot is the basis of its fxn
An extra thick 3-layer basement membrane Specialized viscerial epithelial cells (podocytes) with long extensions (fingers and foot processes) cover the basement membrane Combination of basement membrane and podocyte foot processes form filtration slits that both physically (pressure) and electrostatically produce the glomerular filtrate that empties into bowman’s space which is continuous with the PCT Parietal epithelium and its assoc basement membrane make up bowman’s capsule Mesangial cells provide strx and also have macrophage-like fxn to maintain the integrity of the strx |
|
|
What cells provide structure to the glomerulus and have macrophage-like fxn
|
mesangial cells
|
|
|
What makes up bowman’s capsule?
|
Parietal epithelium and its assoc basement membrane
|
|
|
What influences the length of henle’s loop and the depth of its penetration into the medulla?
|
the location of the glomerulus w/in the cortex
|
|
|
The length of the loop of Henle ______the ability to concentrate urine
(increases or decreases) |
increases
|
|
|
True or false
The number of glomeruli (nephrons) can increase creating the kidney’s significant functional reserve |
False
The number of nephrons doesn’t increase but some increase in functional capability is possible |
|
|
_____ begins at the urinary pole of the glomerulus and makes up the bulk of the cortex
|
PCT
|
|
|
What makes up the bulk of the cortex
|
PCT
|
|
|
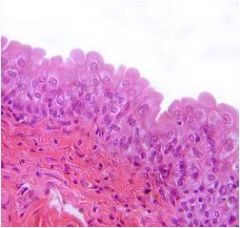
Where do you see simple cuboidal epithelium with microvillus brush borders?
|
PCT
|
|
|
Describe the PCT
|
Simple cuboidal epithelium with microvillous brush borders
Packed with mitochondria (to provide energy) Highly interdigitated on their lateral sides to form tight jxns |
|
|
______ is where 99% of the water is resorbed
|
PCT
|
|
|
______ is where protein/ glucose/ salt are absorbed
|
PCT
|
|
|
______ provides birds and mammals with the ability to concentrate urine
|
loop of Henle
|
|
|
1. How much water is resorbed in the PCT?
2. how much protein/glucose/salt are absorbed in PCT? |
1. 99% (over 1 liter/min)
2. over 2.5 kg/day |
|

|

|
|
|
|
|
|

|

|
|
|

|
|
|
|
|
|

|

|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
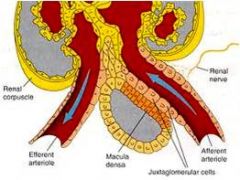
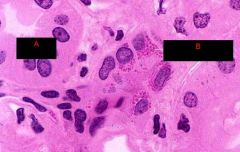
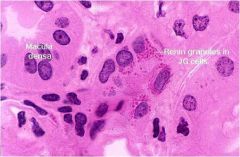
composition of juxtaglomerular apparatus
|
Juxtaglomerular (granular) cells
- Modified myoepithelial cells (pericytes) - Assoc with afferent arteriole - Closely assoc with macula densa - Contain secretory granules Macula densa - Modified epithelial cells of DCT - Assoc with extraglomerular mesangial cells Extraglomerular mesangial cells (lacis cells) - b/w the afferent and efferent arterioles |
|
|
____ are the cells that contribute to the juxtaglomerular apparatus and are located between the afferent and efferent arterioles
|
extraglomerular mesangial cells (lacis cells)
|
|
|
____ are modified epithelial cells of DCT which contribute to juxtaglomerular apparatus
what do they associate with |
macula densa
associated with extraglomerular mesangial cells |
|
|
____ are cells which contribute to the juxtaglomerular apparatus and are modified myoepithelial cells (pericytes) containing secretory granules
|
juxtaglomerular (granular) cells
|
|
|
______ is located at the vascular pole of the corpuscle and the DCT.
Why is this advantageous |
Juxtaglomerular complex (apparatus)
this location allows it to sense and regulate the fxn of the nephron by controlling blood flow (pressure) and thus GFR. |
|
|
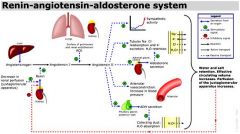
JG cells secrete ____ in response to low perfusion pressure
|
renin
|
|
|
What portion of the renal system fxns to provide active transport of Na+ into the interstitium to maintain the osmotic gradient?
|
distal tubules
|
|
|
describe the macula densa
|
Special region of modified epithelial cells near the vascular pole of the glomerulus
Part of the distal tubules |
|
|
describe the distal tubules
|
Shorter in length than proximal tubules
Composed of simple cuboidal epithelium (no microvilli) Fxn to provide active transport of Na+ into intersititum to maintain osmotic gradient Includes a special region of modified epithelial cells near the vascular pole of the glomerulus called the macula densa |
|
|
describe the loop of henle
|
Provides birds/ mammals the ability to concentrate urine
An abrupt transition from short straight portion of the proximal tubule is marked by the beginning of squamous epithelium Loop reverses course in medulla and w/ the beginning of the distal tubule in the cortex transitions back to cuboidal epithelium (that lack brush borders) During the course of reaching into the depths of the medulla, the loop passes through a concentration gradient, the greatest being deeper in the medulla, where additional water is passively resorbed by diffusion |
|
|
understand the jg apparatus
|
|
|
|
juxtaglomerular apparatus
|
|
|
What are the 3 components of the JG apparatus?
|
Juxtaglomerular (granular) cells
- Modified pericytes around afferent arterial that have myoepithelial fxns Macula densa - Modified epithelial cells of DCT - Interface with JG and mesangial cells Mesangial (lacis) cells - Extraglomerular mesangial cells b/w afferent and efferent arterioles |
|
|
How does the macula densa control GFR?
|
Senses salt concentrations in DCT
Produces locally active vasopressor to control GFR |
|
|
The fxn of ______ is to sense and regulate blood pressure/ flow/ volume and thus glomerular filtration rate.
|
JG complex (apparatus)
|
|
|
____ senses salt concentrations in DCT and produces locally active vasopressor to control GFR
|
macula densa
|
|
|
____ triggers the RAAS in response to low perfusion
|
Juxtaglomerular (granular) cells
By secreting renin |
|
|
|
|
|
______ converts angiotensinogen to angiotensin I
|
renin
|
|
|
Angiotensin I is converted to _______, which is a strong _____ and also stimulates release of ______
|
angiotensin II
strong arterial constrictor stimulates release of aldosterone |
|
|
what does angiotensin II do?
|
strong arterial constrictor
stimulates release of aldosterone from adrenal - increases Na & Cl reabsorption (& therefore H2O retention) in the renal tubule |
|
|
What does renin do?
|
converts angiotensinogen to angiotensin I
stimulates production of antidiuretic hormone (vasopressin) from the posterior pituitary - increase water absorption from collecting ducts |
|
|
_____ increases water absorption from the collecting ducts
_____ increases water retention in the renal tubule |
1. ADH (vasopressin) from anterior pituitary (in response to renin)
2. aldosterone from adrenal in response to angiotensin II (increases Na & Cl reabsorption) |
|
|
Describe the RAAS
|
low perfusion pressure
JG cells secrete renin renin converts angiotensinogen to angiotensin I angiotensin I is converted to angiotensin II (potent vasoconstrictor) angiotensin II stimulates release of aldosterone from adrenal aldosterone increases Na+ and Cl reabsorption and thus H2O retention in renal tubule renin also stimulates the production of ADH (vasopressin) from posterior pituitary - increases H2O absorption in collecting ducts |
|
|
collecting ______ from multiple nephrons connect into collecting ________ which drain into _______
|
collecting tubules
collecting ducts the renal pelvis |
|
|
collecting tubules and ducts are lined by _______
|
columnar epithelium
|
|
|
_______ fxn as the final stage in water and electrolyte balancing
|
collecting tubules/ ducts
|
|
|
collecting tubules/ ducts are regulated by _____
|
ADH (vasopressin)
|
|
|
What happens when ADH levels are high
|
the cells of the CD becmoe highly permeable to water
influence the osmotic gradient (increases from the cortex to the medulla) |
|
|
understand the raas
|
|
|
|
collecting ducts
|
|
|
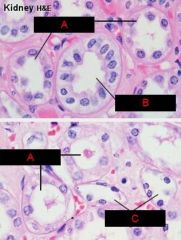
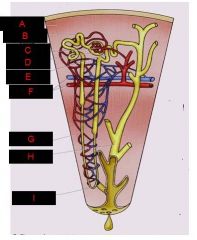
know the arrangement of the kidney
|
|
|
|
A. Cortex
B. Medulla C. Medulla D. Cortex |
|
|
understand the layout of the nephron in relation to the capillary system
|
|
|
|
understand the layout of the nephron in relation to the capillary strx
|
|
|
|
|
|
|
|
|

|
|
|
|
what are teh cell types of the ureter/bladder/urethra
|
transitional epithelium (some squamous in urethra)
lamina propria tunica muscularis (note absences of a muscularis mucosa) stratum cavernosum (veins w/in submucosa of urethra) |
|
|
Where is the very important valve assoc with the urinary system? What does it do?
|
functional one-way valve b/w ureter and bladder
prevents retrograde flow of urine during micturition |
|
|
1. where is transitional epithelium found
2. why is it advantageous to have it in this location 3. describe the appearance of it 4. what problem can be associated with this type of epithelium |
1. occurs exclusively in the urinary system
begins in pelvis of kidney and extends towrds the distal end of the urethra where it transitions into squamous epithelium. 2. advantageous b/c - virtually impenetrable to water - protects against the custic effects of urine 3. cuboidal when not stretched, flat irregular squamous when stretched 4. rapid turnover (mitotic figures common) makes them prone to some viral infections |
|
|
transitional epithelium (urothelium)
begins in pelvis of kidney and extends towards the distal end of urethra where it transitions to squam epi |
|
|
describe the lamina propria of the ureter/bladder/urethra
|
consists mainly of dense CT with bundles of coarse collagenous fibers
|
|
|
describe the musclularis of the ureter/bladder/urethra
|
consists of inner longitudinal and outer circular lary of smooth musc cells
in lower parts of ureter and bladder, an additional outer longitudinal layer of muscles is added |
|
|
describe the lamina propria of the urethra
|
contains loose CT with smooth muscles cells in the muscularis mainly oriented longitudinally
|
|

|

|
|

|

|

