![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
139 Cards in this Set
- Front
- Back
|
1. Where is the thymus located
2. What does it look like 3. When is it largest |
1. in the mediastinum of the thoracic inlet
2. soft multi-lobulated tissue 3. largest prior to puberty (replaced by fat as age) |
|
|
even in the adult, the thymus continues to have ______ activity
|
endocrine
|
|
|
what is unique about nude mice
|
thymus is congenitally absent
no functional immune system |
|
|
what organ has a function to prevent autoimmune disease
|
thymus
thymic stromal cells select T-cells for exclusion in order to provide self-tolerance |
|
|
Premature involution of the _____ is associated with reduced immune fxn
|
thymus
|
|
|
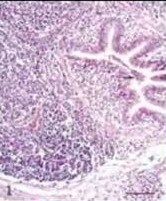
describe the structure of the thymus
|
composed of 2 lobes covered by a thin CT capsule
numerous lobules incompletely divided by septa originating from the capsule |
|
|
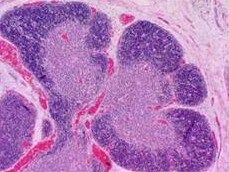
how does the thymus appear in cross section
|
thymic lobules appear to be distinct but are in fact interconnected (incomplete lobulation) with each other through bridges of parenchymal material.
lobules vary in size and are made up of a number of small nodules or follicles lobules are clearly divided into dark staining cortex and a lighter medulla by the differential density of cells in each region. |
|
|
describe thymic follicles
|
irregular in shape and fused together (esp toward interior)
each follicle consists of a medullary and cortical portion |
|
|
why are thymic nodules have such distictly different staining of the cortex/ medulla
|
due to the differential density of cells
the cell types (thymocytes) are the same but the distribution is not equal there are impt physiological differences between those in the cortex and those in the medulla |
|
|
how is the thymus different than the lymph nodes
|
there are no germinal centers
it is not a site of antibody production |
|
|
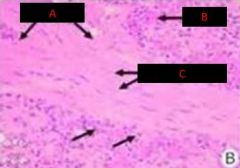
Understand the layout of cells within the thymus
|

|
|
|
thymus
|
|

|
thymus
|
|
|
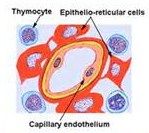
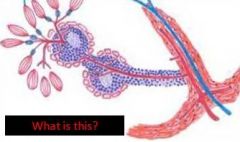
understand the blood thymus barrier
|
|
|
|
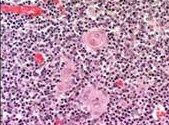
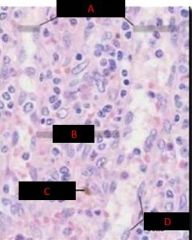
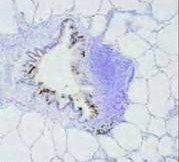
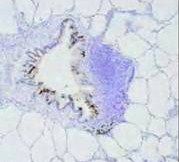
Hassal's Corpuscles
|
|

|
Hassall's Corpuscle
|
|

|
Bursa of Fabricius
|
|

|
Bursa of Fabricius
|
|

|
Bursa of Fabricius
|
|

|
Bursa of Fabricius
|
|
|
Bursa of Fabricius
|
|
|
|
|
|
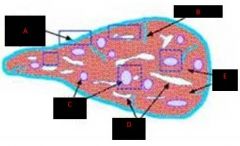
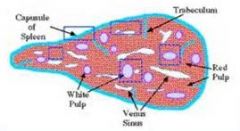
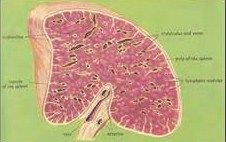
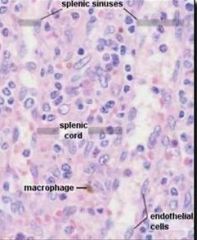
spleen
|
|

|
spleen
|
|
|
spleen
|
|

|
spleen
|
|
|
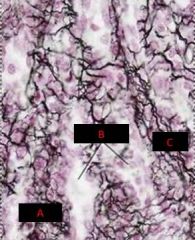
Spleen
A. Trabeculae B. RBC C. Smooth Muscle |
|
|
spleen
periarteriolar lymphocyte sheath |
|
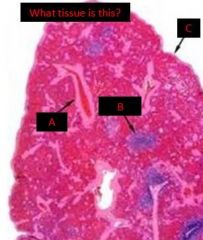
|
spleen
a. trabeculum b. periarteriolar lymphocyte sheath c. capsule |
|
|
|
|
|
|
|
|
|

|
|

|
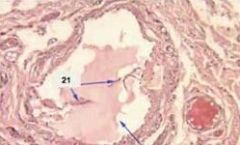
lymph vessel
notice the 1 way valves |
|
|
lymph vessel
|
|
|
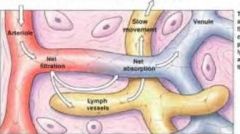
understand the relationship between capillaries and lymphatic vessels
|
|
|
|
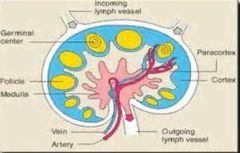
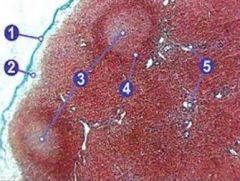
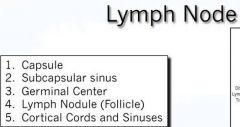
lymph node
|
|

|
lymph node
|
|
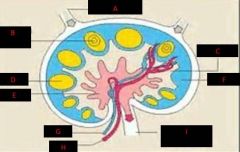
|
|
|
|
|
|
|
|
|
|
|
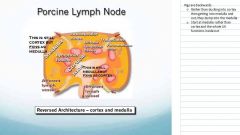
why are pigs screwed up (anatomically...)
|
|
|
|
hemal lymph node
|
|
|
you don't need to cut it out during surgery/necropsy and send it for histopath b/c you will make UT look like a sub-par vet school
|
|
|

|
|
|
|
|
|
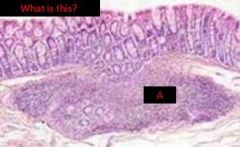
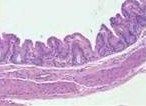
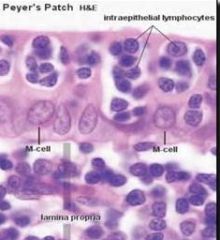
MALT (mucousa associated lymphoid tissue)
peyer's patch in ileum |
|
|
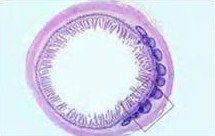
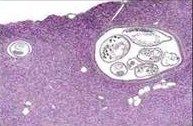
parasite/ MALT
|
|
|
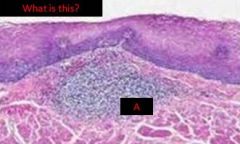
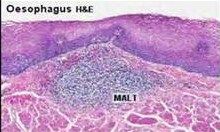
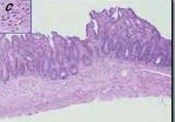
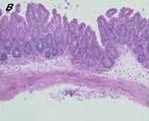
MALT (mucousa associated lymphoid tissue)
|
|
|
MALT (mucousa associated lymphoid tissue)
|
|
|
MALT (mucousa associated lymphoid tissue)
|
|
|

|
|

|
|
|

|

|
|
|
|
|
|
BALT
|
|
|
BALT
|
|
|
BALT
|
|
|
What negative consequence can be associated with BALT?
|
Diffusely lines all airways
Lots of lymphoid hyperplasia around the airways can result in difficult breathing. |
|
|
Where is BALT concentrated
|
concentrated at branch points b/c that is where particles build up
lymph follicles (nodules) with GCs |
|
|
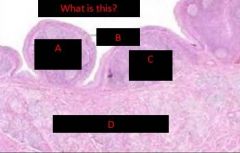
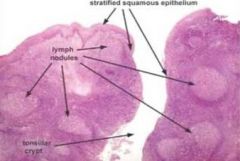
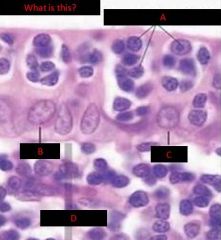
What are 2 examples of GALT and describe them
|
Tonsils (palatine)
- deep crypts - stratified squamous epithelium - lymphoid nodules with germinal centers Peyer's Patch (ileum) - lymphoid domes, nodules, germinal centers - intraepithelial lymphocytes - M cells |
|
|
what makes tonsilar epithelium unique
|
most squamous epithelium has tight jxns to keep things from getting across, but this has crypts
this allow some things to get across |
|
|
GALT primarily produces what antibody
|
IgA
|
|
|
what makes M cells unique
|
M cells (microfold cells)
have invaginations that penetrate up into the epithelium and allow lymphocytes up into this area (so easier to detect antigen...or screw up your gut if you carry the HLA-DQ2, HLA-DQ8, or the MY09B gene) |
|
|
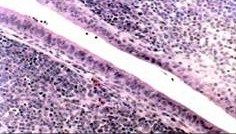
describe thymic blood supply
|
blood vessels enter though capsule
travel ialong septa to the corticomedullary border & enter the parnechyma arterioles entering the thymus send capillaries to the cortex, which branch at the periphery and return at corticomedullary jxn, postcapillary venules are found (represent specialized sites of transit of mature lymphocytes into the blood) |
|
|
how is thymic stroma different than many other organs
|
it is cellular in nature rather than fibrillar
epithelio-reticular cells are branching (tree-like) in shape & put forth processes supported by intracellular cytoskeletal elements these processes come into contact with each other and are held together at points of contact (desmosomes) the process form a completely cellular scaffolding (cytoreticulum) which distinguishes it from other, truly fibrillar parenchyma of other organs |
|
|
the thymic cortex is composed of
|
lymphoid cells supported by a network of finely branced epithelial reticular cells which is continuous with a similar network in the medullary portion
the network of epithelial cells connects with blood vessels |
|
|
where are the largest lymphocytes located in the thymic cortex
|
in the periphery of the cortex
|
|
|
where do the earliest events in thymocyte development occur in the thymus?
|
in the cortex
|
|
|
where does T cell receptor rearrangement & postive selection take place in the thymus
|
in the cortex
|
|
|
thymocytes that reach the _____ have already successfully undergone T cell receptor gene rearrangement & positive selection & have been exposed to a limited degree of negetave selection
|
medulla
|
|
|
what area of the thymus is specialized to allow thymocytes to undergo additional rounds of negative selection to remove auto-reactive T cells
|
the medulla
|
|
|
name the 3 principal cell types in the thymus
|
thymocytes (lymphocytes of the thymus)
few macrophages specialized epithelio-reticular cells (stellate cells) which provide supporting framework (stroma) for the parenchyma |
|
|
most of the lymphocytes in the thymus are _______ (B or T cells)
|
T cells
|
|
|
in order to acqiure immunocompetence, what must happen to lymphocytes
|
they must reside in the thymus for a period of time
|
|
|
how do you know whether you are looking at a macrophage or thymocyte?
|
macrophages are larger with cacuolar nuclei
frequently have coarse granules of undigested material in their cytoplasm |
|
|
describe epithelio-reticular cells
|
obscured by the lymphocytes that sit on them
form a physical, cellular boundary b/w the parenchymal thymocytes and the rest of the body @ periphery of cortex, subjacent to teh capsule and around all blood vessels, the processes form a continuous cellular layer constitutin the blood thymus barrier - prevents exposure of immature lymphocytes to blood borne antigens |
|
|
what forms a physical, cellular boundary b/w the parenchymal thymocytes and the rest of the body?
|
epithelio-reticular cells
|
|
|
what prevents exposure of immature lymphocytes to blood borne antigens
|
epithelio-reticular cells in concert with the lining epithelium of the capillaries
|
|
|
what forms the blood-thymus barrier
where is it |
the processes of the epithelio-reticular cells
at periphery of the cortex, subjacent to the capsule & around all blood vessels |
|
|
hassall's corpuscles
|
degenerate epithelio-reticular cells
appear as concentric eosinophilic whorls of materials no function each consists of a concentraic mass of epithelial cells joined by desmosomes and containing intracellular bundles of filaments |
|
|
where to B cells get their name from
|
bursa of fabricius
- the site of hematopoiesis in birds - particularly the source of B cells |
|
|
describe the bursa of fabricius
|
unique to birds
site of hematopoiesis source of B cells in mammals, bone marrow does this located in the caudal dorsal part of cloaca as a diverticulum (atrophies with age like thymus) has blind, crypt-like invaginations appears like the thymus unlike tonsil, overlying epithelium is columnar (not squamous) and there are no germinal cells |
|
|
is the bursa of fabricius more like the thymus or tonsil
|
looks similar to thymus & atrophies with age
unlike tonsil - has columnar (not squamous) overlying epithelium - no germinal centers |
|
|
infectious bursal disease
|
viral dz that destroys the bursa
- reduces immune fxn - increases susceptibility to other infectious dz |
|
|
is the spleen part of the circulatory system or the lymphatic system
|
yes
(it is though of as part of the circ sys but traditionally described with lymphatic organs b/c large pop of lymphocytes so significant immune fxn) |
|
|
what is the pulp of the spleen?
|
the parenchyma
most of it is soft, dark red masss (red pulp) - large, irregular, thin-walled blood vessels (splenic sinusoids) interposed b/w sheets and strands of reticular CT (spenic cords) - red b/c of blood the balance of the spleen is composed of lymphoid tissue (white pulp) - small irregularly sized pale yellow to white nodules & cords |
|
|
describe the splenic capsule
|
composed mostly of collagenous and elastic CT interspersed with smooth muscle (responsible for splenic contraction)
tear or rupture in the capsule results in significant internal hemorrhaging the capsule sends septa (trabecula) part way into the interior andfrom these arise a delicate network of reticular fibers, to from a stromal network on which the lymphocytes rest |
|
|
what is one impt fxn of the spleen (esp significant for racing horses and marine mammals)
|
act as a reservoir for erythrocytes
the contractionj of the capsule expels these into circulation when extra oxygen carrying capacity is needed |
|
|
how does the spleen differ from lymph nodes (as far as its lymphatic fxn goes)
|
it is inserted directly into the blood stream
|
|
|
where in the spleen does storage and blood filtration occur
|
in the red pulp (composed of sinuses, splenic cords, and the marginal zone)
|
|
|
why does the spleen become enlarged when under some general anesthetics?
|
relaxation of muscle tone
|
|
|
describe the spleen's hematopoietic fxns
|
impt during gestation
after birth (in mammals) stops erythropoietic fxn except when extra erythropoietic production is needed (extramedullary hematopoiesis) |
|
|
describe the spleen's lymphoid fxns
|
has significant reticuloendothelial fxns
produces lymphocytes and antibody |
|
|
what is the spleen's most impt fxn?
|
acts as a vascular filter (clearing blood of aged and diseased cells and foreign particles
is the site of immune rxns to blood-borne antigens antibodies are produced and antibody coated blood cells are removed from circulation by the spleen immune fxns occur in white pulp (composed of periarteriolar lymphocyte sheath which are rich in T cells as well as lymphoid follicles and germinal centers which are rich in B cells) |
|
|
what is the fxn of the white pulp, what is it composed of?
what is the fxn of the red pulp, what is it composed of? |
White Pulp = immune fxns
composed of - PALS (rich in T cells) - lymphoid follicles & germinal centers (rich in B cells) Red pulp = storage & blood filtration composed of - sinuses - splenic cords - marginal zone |
|
|
why is the spleen a common site of infection/ cancer/ emboli/ etc.
|
b/c of its fxn of storage and filtration, plus the reticuloendothelial fxns
|
|
|
______ are the first part of the arterial input inot the spleen
|
central arteries
branches of splenic artery enter via the capsule & divide into trabecular arteries as these leve septum and enter the interior of the spleen, it immediately acquires a continuous coating of lymphocytes and is thus called central arteries (the sleeve of lymphocyte is the PALS) |
|
|
_____ collectively constitute what is called the "white pulp" of the spleen
|
all the PALS
|
|
|
Where in the spleen can the special conditions required for proliferation of B lymphocytes be met
|
the PALS (white pulp)
will see germinal centers at intervals (number and size of them will vary based on the immune state of the animal) |
|
|
______ separates the red and white pulp
|
the marginal zone
|
|
|
what happens to the central artery once it reaches the marginal zone
|
divide into smaller vessels
fine branches of central artery (penicillar arteries - characterized by cuboidal epi) branch again to form arterial capillaries as they exit white pul, are surrounded by a sheath of phagocytic cells and reticular fibers (now called sheathed arteries) may empty the blood iirectly into splenic sinusoids (closed circulation) or into reticular CT of splenic cords (open circulation) |
|
|
the white pulp surrounds ________ as a periarterial lymphoid sheath
|
the central arteries
|
|
|
describe the PALS
|
has a diffuse framework of reticular fibers
resident lymphocytes of the diffuse region are supported by it mostly T lymphocytes with less numbers of macrophages and plasma cells nymph nodules and germinal centers (Malpighian bodies) formed by B lymphocytes are present along the course of the central arteries germinal cneters are clones of B lymphocytes that are isolated so that these cells can develop properly consequently the stroma in GCs isnt' fibrillar in nature (similar to the thymus) |
|
|
Does red or white pulp constitute teh bulk of splenic volume
|
red
|
|
|
describe the red pulp
|
constitutes the bulk of splenic volume
supporting reticulum of red pulp is continuous with the septa (consist of reticular fibers invested by reticulocytes) arranged into anatomizing splenic cords separated by venous sinuses sinuses are blood spaces lined with endothelium and contain circulating blood cells cords are the masses of cells in between sinuses containing erythrocytes & many other cell types (esp macrophages) phagocytosis of aged erythrocytes occurs in cords (hemosiderin present) |
|
|
where in the spleen does phagocytosis of aged erythrocytes occur?
|
the cords of the red pulp
|
|
|
where in the spleen is hemosiderin present
|
the cords of the red pulp (b/c that's where phagocytosis of aged RBC occurs)
|
|
|
how are sheathed capillaries different from other blood vessels
|
most blood vessels are lined by simple squamous epithelium
sheathed capillaries have endothelium composed of fusiform cells oriented paralell to the long axis surrounded by a sheath of reticulocytes and macrophages bound together by reticular fibers the cells of the walls are phagocytic |
|
|
true or false
all capillaries arising from the penicillar arteries become sheathed capillaries |
false
|
|
|
what cell types are the main resident population of the splenic cords
|
macrophages & reticular cells
|
|
|
blood cells emptied into the splenic cords re-enter the blood vessels through ________
|
the endothelium of the sinusoids
|
|
|
describe the endothelial cells of the splenic sinusoids
|
elongated (in cross section, may appear cuboidal) oriented along the long axis of the sinusoids
no jxnal complexes incomplete basement membrane (forming narrow circular bands around the endothelial cells with large intervening fenestrations) |
|
|
macrophages ingest aged erythrocytes, platelets, and other matter as they pass through _______
|
the splenic cords
|
|
|
true or false
cells of the blood can move from a splenic sinus to an adjacent cord and vice versa |
true
|
|
|
true or false
the endothelium lining the splenic sinusoids is phagocytic |
true
|
|
|
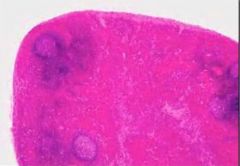
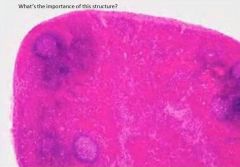
why do lymph nodes become enlarged?
|
b/c of proliferation of lymphocytes (mostly B cells)
|
|
|
name 2 common sites for metastatic cancers to be found
|
lymph nodes
spleen |
|
|
what is interstitial fluid
|
lymph once it enters a lymph capillary
|
|
|
most interstitialfluid returns via ______
|
venous circulation
1% becomes lymph and passes through 1 or more LN before returning to venous circulation |
|
|
describe high-endothelial vessels
|
in deep cortex of lymph nodes
low cuboidal epithelium lymphocytes which reach the lymph node via blood stream migrate through this epi as part of their recirculation |
|
|
what 2 things result in edema
|
excessive lymph production
failure to flow |
|
|
describe lymph vessels
|
simple endothelial lined tubes that do no branch or anastomose
at their periphery, the basement membrane is incomplete and lacks pericytes can be difficult to see histologically larger vessels have complete basement membranes, pericytes, and some smooth muscle |
|
|
what is the medulla made up of
|
meduallary cords of lymphatic tissue
- plasma cells - macrophages - B cells medullary sinuses - vessel like spaces separating the cords - lymph flows into the sinuses from cortical sinuses and into efferent lymphatic vessels |
|
|
describe a reactive germinal center
|
dark and light zones
dark - mostly T cells & proliferating B cells light - where B cells mature |
|
|
what is the importance of the paracortical zone
|
where T cells mainly interact with dendritic cells and macrophages to promote the immune response
|
|
|
as lymph moves through the __a____ & ___b____, antigens are detected by and processed by _____c____ & ____d____
|
a. subcapsular
b. cortical sinuses c. macrophages d. lymphocytes |
|
|
describe the main cell types of the cortex
|
outer cortex
- mainly B cells arranged as follicles (may develop germinal center) deeper cortex - mainly T cells |
|
|
how are pig LN different
|
lymph nodules (including germinal centers) are located in the medulla and medullary cords are located in the cortex
|
|
|
where do you find hemal LN
|
in ruminants
retroperitoneal along vertebral column with some visceral organs along the jugular furrow |
|
|
describe a hemal LN
|
strx similar to LN but with some characteristics of the spleen (capsule and trabecula contain smooth muscle and sinuses are filled with blood rather than lymph)
|
|
|
diffuse vs nodular lymphatic tissue
|
diffuse
- unorganized collection of lymphocytes - usually assoc with all mucosal surfaces (even skin) - density of lymphocytes assoc with the degree of antigenic stimulation &/or infection (so mine are currently over-run) - lymphatic tissue outside of specifically lymphatic organs is, by definition, diffuse - lymphoid organs (spleen/ LN) also have diffuse lymphatic tissue located b/w more defined strx (nodules) nodular tissue - always occurs w/in a background of diffuse lymphatic tissue (even spleen & LN) - typical ex of nodular lymphatic tissue is germinal center (highly ordered collection of B cells found in some lymphoid organs) when diffuse lymphatic tissues associated with mucosal surfaces become particularly dens but is not encapsulated, they can become so well defined to be recognized as a specific strx (tonsil/ peyer's patch) |
|
|
______ protects the body against pathogens which may enter the body via the mucosa
|
MALT
|
|
|
give an example of MALT
|
tonsil
in resp airway |
|
|
MALT produces ____ which can be taken up by epithelial cells and released onto epithelial surface
|
IgA
|
|
|
what are tonsils
|
accumulations of llymphoid tissue surrounding the openings of the digestive and resp tracts
palatine tonsils are ofspecial significance and are located in teh lateral wall of the oropharynx and covered by strat squam epi - surrounded by thick hemicapsule of CT (not a capsule) which delimits them from the pharyngeal muscle and facilitates their removal |
|
|
why do deep crypts help the tonsils fxn
|
exposure to antigens relies on contact of antigens with cells of the immune system across the epithelium
the deep crypts result in increase of surface area to facilitate this the epithelium may specialize in places to form open meshwork of cells with an incomplete basal lamina (reticulated epi) which allows infiltration of epi by lymphocytes and macrophages |
|
|
tonsilar lymphoid nodules consist mainly of
other areas are occupied by |
B lymphocytes
T lymphocytes, activated B lymphocytes (germinal centers), and other cells of the immune system |
|
|
where do the most prominent accumulations of diffuse lymphocytes or activated lymph follicles of the GI sys occur
|
in the ileum & the appendix in the form of peyer's patches
dome shaped protrusions into the lumen of the ileum (germinal centers deep in submucosa) |
|
|
describe the epithelium of peyer's patch domes
|
appears columnar and contains cells with deeply invaginated basal surfaces (M cells)
immune system cells can enter these invaginations (intraepithelial pockets) where they are exposed to materials which have been endocytosed by the epithelial cells and then released into the invaginations goblet cells are rare or absent in the epithelium which covers the domes |

