![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
Six functions of kidneys |
1) excrete waste: Urea- main waste product breakdown of proteins urobilin- breakdown of hemoglobin ammonia- in small amounts. Most is converted to urea metabolites- broken down hormones, vitamins, etc 2)regulate blood volume (H20 balance) 3) regulate electrolyte balance (Na+, K+, Mg+, Ca+) 4) hormone synthesis (renin, calciteol-active form of vitamin D erythropoietin- synthesis of new red blood cells) 5)pH regulation (excretion of H+ ions vs reabsorption of HCO3- ions) 6) gluconeogenesis (under starvation) |
|
|
Pyelitis |
Infection of the renal pelvis and calyces |
|
|
Pyelonephritis |
Infection and inflammation of an entire kidney More common in females as fecal bacteria can more easily enter the urethra and spread upwards Severe cases:swelling of the kidney, abscess formation, and pus filling the renal pelvis leading to kidney damage. |
|
|
Polycystic kidney |
Relatively common congenital abnormality Development of many fluid filled cysts interfering with kidney function and significant enlargement of the kidneys Most often causes by changes to PKD1 and PKD2 genes Many people have kidney failure by age 60 |
|
|
Nephrons |
Smallest functional unit of kidney
1 million per kidney
2 types based on location 1)cortical-85% mostly in the cortex 2) juztamedullary- long loops of Henle. Have greatest concentrated power for producing urine
Cheif functions: regulates H2O, and soluables by filtering blood, reabsorbing what is needed, and secreting what is not.
|
|
|
Blood flow through kidneys |
Aorta, renal artery.......afferent arteriole, glomerulus, efferent arteriole.......renal vein, inferior vena cava |
|
|
Ultrafiltrate vs tubular fluid vs preurine vs urine |
Ultrafiltrate- glomerulus Tubular fluid- Preurine- loop Urine- |
|
|
Renal corpuscle |
Ultrafiltration of blood |
|
|
Proximal tubule |
Cuboidal cells with microvilli for reabsorbtion of H2O , glucose, and other solites |
|
|
Defending loop of Henle |
Reabsorption of H2O establishment corticomedullary gradient |
|
|
Ascending loop of henle |
Active transport of Na+ and other ions, establishment of corticomedullary gradient |
|
|
Distal tubule |
Cuboidal cells with few microvilli, secretion/reabsorption of H2O and ions |
|
|
Collecting duct |
Receive fluid from several distal tubules, principal cells (reabsorption of H20 dependent upon hydration state) and intercalated cells (maintenance of acid-base- balance of blood |
|
|
Vasa Recta |
Capillary surrounding Loop of Henle, Maintenance of corticomedullary gradient |
|
|
Ultrafiltrate |
Just like plasma, without protein |
|
|
What is special about glomeruli capillaries |
1) thin- They are fenestrated making them 50x more leaky, 2) huge surface area- they zig zag and spiral many times. 3) Blood pressure is higher because blood flow enters the capillary at a higher volume than what can leave. |
|
|
What pressures affect glomerular filtration |
1) glomerular hydrostatic pressure (PGC) pressure in capillary causes fluid to flow out. Promotes filtration 2) Bowman's Hydrostatic Pressure (PBS)- Drives reabsorption back into the capillary (opposes filtration) 3) Plasma Colloid Osmotic Pressure (πGC)- opposes filtration 4) Bowman's Colloid Osmotic Pressure ( πBS) promotes filtration |
|
|
Regulation of glomerular filtration rate |
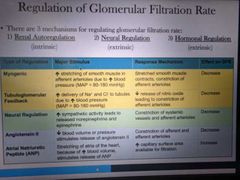
|
|
|
Renal clearance |
Volume of plasma the kidneys can clear of a substance in a given time Tests of renal clearance are used to determine GFR and health of kidneys |
|
|
Inulin |
A plant polysaccharide used to test renal clearance Because it is easily filtered but not reabsorbed And it's gfr is about the same as a normal kidney |
|
|
Renal clearance rate formula |
C ml/min= UV/P U- concentration mg/ml in urine V- flow rate of formation ml/min P- concentration of same substance in blood |
|
|
Chronic renal disease |
GFR <60ml/min for >3 months |
|
|
Renal failure |
GFR <15 ml/min Typically occurs in the final stages of chronic renal disease Results in uremia -ionic and hormonal imbalances and metabolic abnormalities |
|
|
Paracellular vs transcellular |
Substances are reabsorbed between cells vs Substances are reabsorbed through the cells often requiring energy |
|
|
Dehydration |
DT reabsorbs up to 19.8% of water. Max total water reabsorbed is 99.8%. Creates very hyperosmotic urine |
|
|
Normal hydration |
DT absorbs 19% of water. Total reabsorbed is 99%> slightly hyperosmotic urine |
|
|
Over hydration |
DT absorbs as low as 0% of water. Minimum water absorbed is 80% Very hypoosmotic urine |
|
|
Distal tubule collection duct relationship |
10 dt drain into 1 cd |
|
|
Urine |
Typically 95% water Nitrogenous wastes (urea, uric acid, creatine) Na, k, Ca, Mg, Cl, HCO, phosphates, and sulfates |
|
|
Diuretic |
Chemicals that enhance urinary output Alcohol, glucocorticoid drugs |
|
|
Specific gravity of urine |
Concentration of solutes 1 is water, 1.03 is very high |
|
|
Urobilinogen |
(bilirubin) from breakdown of hemoglobin Elevated suggests anemia Can be from hemolytic or pernicious anemia Hepatitis Cirrhosis Congestive heart failure Mono |
|
|
Blood in urine could be from |
Inflammation of urinary organs Kidney stones or damage |
|
|
Ketones |
Diabetes |
|
|
Glucose |
Diabetes. You shouldn't loose glucose |
|
|
Proteins |
Kidney damage |
|
|
Kidney stones |
Renal calculi. Crystalized deposits of CA mg or uric acid
|
|
|
Nephrolithiasis |
Kidney stones in the kidney |
|
|
Ureterolithiasis |
Stones in the ureters |
|
|
Trigone |
Smoothe triangular area of the bladder where the ureters empty urine |
|
|
Rugae |
Helps bladder stretch and expand |
|
|
Urethritis |
Inflammation of urethra |
|
|
Cystitis |
Inflammation of bladder |
|
|
Kidney infection |
When bladder infection spreads upwards |
|
|
Micturition |
Urination: Contraction of destrusor muscle Opening of internal urethral sphincter Opening of external sphincter |
|
|
4 types of incontinence |
1) urge- sudden intense urge followed by involuntary loss of urine 2) stress- increase in intra-abdominal pressure forces urine out 3) mixed- involuntary leakage due to a mix of urge and stress 4) overflow- dribbling due to a bladder that doesn't empty completely |
|
|
Summary slide |
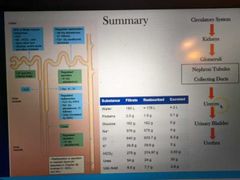
|

