![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
77 Cards in this Set
- Front
- Back
|
Lymphoid organs and tissues 2 categories |
Structures in which lymphocytes develop, are stored, or carry out immune responses 1-primary 2-secondary |
|
|
Primary lymphoid sites |
Sites where pluripotent stem cells give rise to mature b cells and immature/mature pre-t cells
These sites change with age and season Thymus and bone marrow |
|
|
Secondary lymphoid sites |
Sites where most immune responses occur Nodes-focus on lymph Spleen-focus on blood Tonsils-focus on respiratory tract and pharynx Appendix and Peyer's patches- focus on gi tract |
|
|
Types of leukocytes |
Granulocytes: Neutrophils Eosinophils Basophils Agranulocytes: Monocytes Lymphocytes |
|
|
Neutrophils |
Most abundant immune cell Attack by Phagocytosis and degranulation Bacterial infection |
|
|
Eosinophils |
Attack endoparasites Contribute to allergic reactions
They attach themselves to TLRs and release granules containing enzymes (lipases, ribonuleases, deoxyribonuclease) and peroxidases. Contribute to allergic reactions |
|
|
Basophils |
Release pro-inflammatory chemicals Contribute to allergic reactions Has lots of granules that have histamines and prostaglandins Releases chemicals to attract other cells, and to inflame the area |
|
|
Monocytes |
Can be wandering or fixed. Grow into macrophages |
|
|
Lymphocytes |
B cells T cells Memory T&B cells B= antibodies T= helper regulatory cytotoxic |
|
|
Mast cells |
Produce pro-inflammatory chemicals Contribute to allergic reactions |
|
|
Dendritic cells |
Antigen presenting cells |
|
|
Innate immunity |
Non specific (all non self cells are attacked the same way) Immediate response (1st and 2nd lines) No immunological memory |
|
|
Surface Barriers |
Skin Mucous membranes Hairs and cilia Secretions |
|
|
Internal barriers |
Antimicrobial substance Granulocytes Macrophages Nk cells Inflammation Fever |
|
|
Adaptive immunity |
Antigen-specific Lag time from exposure to response (3rd line) Immunological memory after exposure Systematic response |
|
|
Cell mediated immunity |
Cytotoxic T cells Immunity to intracellular bacteria, viruses, fungi, and protozoa
|
|
|
Humoral immunity |
B cells/plasma cells Immunity to extracellular bacteria viruses and toxins |
|
|
Toll-like receptors |
Identify and bind tightly to structures or patterns (pathogen associated molecular patterns) on pathogens Humans have 11 tlr types Each recognizes a pamp present in while groups of pathogens but not in human cells |
|
|
Macrophages |
Largest leukocyte and primary phagocytic Free macrophages wander blood and lymph killing pathogens Fixed macrophages are found in: Brain-miceoglia Liver-coopver? Skin- Dermal macrophages Aveoli-aveolar inhaled Small intestine |
|
|
Opsonization |
Antibodies or complement proteins are opsonins that coat pathogens making them easier to attach to |
|
|
How do phagocytic cells destroy microbes? |
1) adhere to pathogen using TLRs 2) form pseudopodia, engulfing the particle and forming a phagosome 3) lysosome fuses with phagocytic vesicle, forming phagolysosome 4) toxic compounds and lysosomal enzymes destroy pathogens 5) exocytosis of the vessicle may remove debris |
|
|
Respiratory burst |
Helper T cells stimulate macrophages to produce respiratory bursts which kill resistant pathogens by 1)releasing cell-killing free radicals 2) producing oxidizing chemicals (ex. H2O2) |
|
|
Definsins |
In neutrophils, pierce cell membrane of pathogen |
|
|
Nk cells |
Natural killer cells Non phagocytic granular lymphocytes that police the blood and lymph Target virus infected cells before adaptive immune system is activated Also target "non self" cancer cells Kill by binding and releasing toxic substances from granules Perforin Granzymes |
|
|
Perforin |
Creates perforations in membrane...lysis |
|
|
Granzymes |
Enter perforin channel, digests proteins and induce apoptosis |
|
|
Interferons |
Immune modulating proteins Cells that are infected secrete ifns to warn neighboring cells to put up defenses Inf-a inf-b. (Alpha and beta) Stimulate production of antiviral proteins Activate nk cells Inf-y (gamma) Secreted by t cells, nk cells, and macrophages Widespread immune mobilizing effects Potent activator of macrophages, but also activates nk and t cells Also blocks t cells that are immune supressor cells |
|
|
Complement proteins |
20 blood proteins that enhance immune responses Circulate in blood in inactive form Includes c1-c9 Enhanses inflammation and directly destroys bacteria Enhanses both innate and adaptive defenses Can be activated 3 ways |
|
|
How are complement proteins activated? |
1) Classical pathway: antibodies bind to bacteria. antibody binds to circulating complement proteins. That activate until C3 is activated 2) lectin pathway: activated when lectin (sugars) bind specific bacterial surface carbohydrates, then bind/activate complement proteins. They activate until C3 is activated. 3) alternative pathway: activated when complement proteins directly bind to bacteria All three pathways happen in an immune response. All about activating c3 |
|
|
What can complement do? |
Once c3 is activated, it splits into two parts. C3b-opsonizarion- coats surface of pathogen which enhanses Phagocytosis by making it much more noticeable to phagocytes C3a- enhanses inflammation, stimulates histamine release by basophils, increases blood vessel permability, attracts phagocytes by chemotaxis. Makes travel to infected cell easier for the cells |
|
|
Fever |
High body temperature Innate immune response Leukocytes and macrophages exposed to foreign substances secrete pyrogens As long as the fever remains below 40c (104f) there are benefits |
|
|
Benefits of fever |
1-liver and spleen increase storage of Fe and zn which bacteria need to reproduce 2) inhibition of microorganism growth/reproduction 3- promotes activation of macrophages 4- stimulates bactericidal activity of neutrophils 5- increases production of interferons 6- stimulates activation lymphocytes 7- promotes antibody production 8- increased BMR= tissue repair |
|
|
Inflammation and steps |
Non specific response to local tissue damage such a trauma, heat, infections Steps: 1) Chemical signals (inflammatory chemicals) 2) vasodilation and vascular permeability 3) phagocyte mobiliation |
|
|
Important chemical signals |
Histamine- vasodilation and permability Kinins- " " and attract phagocytes Prostaglandins- intensity the effects of histamines and kinins Leukotrienes- increase permeability and promote phagocyte adherence to pathogens Complement- multifunctional Cytokines- have a multitude of functions |
|
|
4 cardinal signs of inflammatory reaponse |
Redness and heat (hyperemia) swelling (exudate-fluid with clotting factors and antibodies & edema) Pain (chemicals from bacteria and edema pushes on nocireceptors) |
|
|
Benefits of edema |
Surge of fluid helps sweep foreign particles into lymph vessels to lymph nodes to trigger more response Delivers complement proteins to the area |
|
|
Neutrophils |
Most abundant leukocytes and first to arrive to injury Bacteria specialists |
|
|
Inflammation diapedesis and chemotaxis steps |
1) leukocytosis- neutrophils are released from bone marrow in response to leukocytosis-inducing factors 2) margination- cell adhesion proteins (can's) like Velcro, grab passing neutrophils 3) diapedesis- neutrophils flatten and squeeze outside of the capillaries 4) chemotaxis- following a chemical trail. The cells follow the route to the infected area chemical trail is made of : complement proteins, c3b bacteria parts, histamines, gamma After about 12 hours macrophages come in as reinforcements. They consume bacteria and cell debris. Tissue repair |
|
|
Benefits of inflammation |
1) prevents spread of damaging agents 2) disposes call debris and pathogens 3) alerts adaptive immune system 4) sets the stage for repair |
|
|
Homeostatic imbalance: abscesses |
Occurs when collegen fibers are laid down over a sac of pus
Pus is a mixture of dead neutrophils, tissue, and living/dead pathogens
Causes a painful swollen lump that may need to be drained |
|
|
Adaptive immune system |
Provides protection against specific microbes and pathogens. Targets specific viruses based on their antigens There is a lag time from exposure to response (3rd line) Immunological memory after exposure Systematic response Cell mediated and humoral immunity |
|
|
Cell mediated immunity |
Cytotoxic T Cells Immunity to intracellular bacteria, viruses, fungi, protozoa, and cancer
Attack infected self cells |
|
|
Humoral immunity |
B cells/plasma cells Immunity to extracellular bacteria viruses and toxins |
|
|
Pathogen vs antigen |
Pathogen- potential disease causing microorganisms Focus of the innate immune system All are antigens
Antigen- Elicits an adaptive immune response (immunogenicity) and reacts specifically to the antibodies and cells it provoked (reactivity). Ex. Pollen no it all are pathogens Can be complete, or just a small part (hapton) The part of the antigen that is bound by an antibody by or lymphocyte receptor (epitope) |
|
|
Mhc proteins |
Major histocompatibility complex proteins Transmembrane glycoproteins that are unique to the cells of every individual. All body cells, except RBC have MHC1. Allows immune cells to identify all cells as self cells MHC2 only on antigen presenting cells (macrophages, dendritic cells, and v cells) Contain grooves that hold a piece is self antigen or foreign antigen allowing T cells to identify self cells as non-antigenetic and foreign antigens as not self T lymphocytes can only recognize antigens that are presented on MHC proteins |
|
|
Where do t and b lymphocytes originate |
Red bone marrow |
|
|
Where do t and b cells mature? |
Thymus (t) and bone marrow (b) They develop immunocompetence, self recognition, and self-tolerance
|
|
|
Immunocompetence |
Ability of a lymphocyte to recognize one specific antigen (there are a billion different receptors they could develop) |
|
|
What is self recognition and self tolerance. How is it developed |
Positive selection If MHC1 binds to T cell if moves on. If T cell doesn't bind to MHC1, it is destroyed Negative selection Next if T cell binds to a self antigen it is destroyed. |
|
|
Seeding secondary lymphoid organs and circulation |
Immunocompetent, but naive lymphocytes leave and colonize secondary lymphoid organs (wait until they are needed) |
|
|
Antigen encounter and activation |
When a lymphocyte's antigen receptor binds it's first antigen, that lymphocytes becomes active |
|
|
Proliferation and differentiation |
Activated lymphocytes replicates lots of clones (clonal selection) Then differentiate into memory or effector cells Most become effector cells (actually have an effect) |
|
|
Steps of adaptive immunity |
1. Origin 2. Maturation 3. Seeding secondary lymphoid organs and circulation 4. Antigen encounter and activation 5. Proliferation and differentiation |
|
|
Antigen presenting cell apc |
Do not respond to specific antigens. They break down the pathogen, then show t and b cells the antigen to activate them
Macrophages Dendritic cells B cell |
|
|
Macrophages |
Widely distributed in connective tissues and lymphoid organs Present antigens to t cells. Which activates t cell and itself Once activated it becomes a voracious phagocytic killer monocyte>macrophages>activated |
|
|
Dendritic cells |
Best antigen presenting cell Found in connective tissues and epidermis Acts as mobile sentinel (constantly moving around and looking for pathogen) of tissue separating inside from environment Phagocytize pathogens that enter the body, dig at them, travel to lymph nodes, and present the antigens to t cells Key link between innate and adaptive immune system |
|
|
Exogenous antigens |
Antigens not already in a cell Pollen, bacteria, toxins, parasites, and viruses that are not already in a cell |
|
|
B cells |
Can recognize and bind to exogenous antigens in lymph, blood, or tissue fluid Apc aslo activate b cells |
|
|
Humoral immune response |
Process of a naive b cell to a ln active b cell to a plasma cell
Initiated when b cells encounter a specific target antigen
Route one: (t cell independent activation) ~unprocessed antigens bind (cross-linked) to specific B cell receptors and the cell activates ~Activation triggers receptor-mediated endocytosis of antigen-receptor complexes ~Clonal selection is the result, but the T cell-independent response is short lived, and does not result in the production of memory b cells. So if another exposure occurs, you won't have memory cells for the antigen Route 2: first two steps are the same. Then processed antigens, bound to MHC II, are presented to a TH cell specific for that antigen. It clones memory cells for future infection. |
|
|
Epitope |
Parts of a pathogen that receptors bind to that identify it as foreign |
|
|
B cell activation and development |
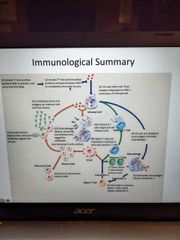
Look at summary slide on lecture 4 |
|
|
Immunoglobulins |
Antibodies Secreted by plasma cells (activated b cells) Bind to a specific epitope on the antigen in a lock and key fashion They don't destroy pathogens, but they bind to them to prepare for later destruction
|
|
|
What is the structure of an antibody |
Composed of Two long heavy chains and two short light chains. Each chain had a variable "sensory" region that binds antigens And a constant region "effector" which determines the class and function of antibody |
|
|
5 Immunoglobulin classes |
IgM (pentamer- 5 parts) IgA (dimer- 2 parts) IgD (monomer- 1 part) IgG (monomer) IgE (monomer) |
|
|
IgM |
First Ig class secreted by plasma cells during the primary response, so it's presence indicates active infection Readily activates complement |
|
|
IgA |
Known as secretory IgA because it is found in body secretions such as saliva, sweat, breast milk, and intestinal juice Helps stop pathogens from attaching to epithelial cell surfaces including mucus membranes |
|
|
IgD |
Found on B cell surface |
|
|
IgG |
Most abundant antibody in the plasma (75-85% of antibodies)
Main antibody of both secondary and late primary responses
Readily activates complement
Ex chicken pox. And vaccine Monomer circulating in blood stream |
|
|
IgE |
Binds to mast cells or basophils. Triggers the release of histamines and other chemicals that mediate inflammation and allergic reaction |
|
|
How do antibodies work? |
They bind to antigens which deactivates them, and tags them for destruction They form antigen-antibody complexes |
|
|
Neutralization |
Antigens Block dangerous parts of bacterial endotoxins and viruses keeping them from causing damage while waiting for other cells to phagocytize them |
|
|
Aggulination |
Antibodies link cell-bound antigens together |
|
|
Precipitation |
Antibodies make soluble antigens insoluble |
|
|
How do you acquire adaptive immunity? |
1) active natural immunity- own immune system, after your own b-cells encounter a pathogen by chance 2) active artificial immunity- delivered exposures to an antigen (vaccine) 3) passive natural immunity- someone else's antibodies are passed to you (breastfeeding, through placenta). They degrade over time 4) passive artificial immunity- IgG serum when someone (or animal) else's immune cells are received (ex. for someone with lukeimia) |
|
|
Immunodeficiencies and which cells they target |
Severe combined immunodeficiency (scid) - deficit in b and t cells Hodgkin's disease (lymphoma)- cancer of b cells Hiv- destroys helper T cells |
|
|
Autoimmune diseases, and what they target |
Rheumatoid arthritis-joints Myasthenia gravis- nerve and muscle connections Multiple sclerosis- mylenin sheaths Type 1 diabetes mellitus- beta cells in the pancreas Glomerulonephritis- nephrons of the kidneys Graves disease- thyroid Systemic lupus- multiple systems |
|
|
Review this slide |
|

