![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
90 Cards in this Set
- Front
- Back
|
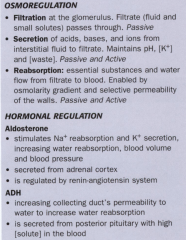
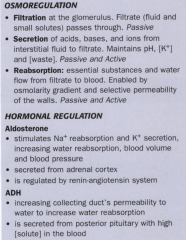
4 processes of urinary system?
|
Filtration
Reabsorption and Secretion Concentration of Urine Excretion |
|
|
The process by which the kidney removes unwanted substances from the plasma.
Desired substances reabsorbed |
Filtration
|
|
|
Process of filtration occurs through what membrane?
|
Glomerular membrane
|
|
|
What kind of pressure is used to creat pressure gradient to filter substances through the glomerular membrane?
|
Osmotic Pressure
|
|
|
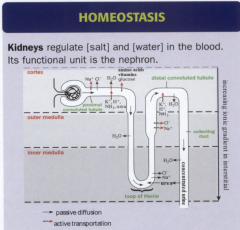
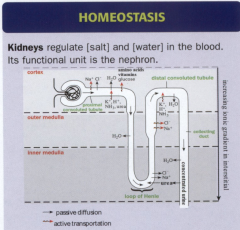
Basic functional unit of the kidney?
Approximately how many per kidney? |
Nephron
Approximately 1 million nephrons per kidney |
|
|
What has 2 limbs and facilitates movement of substances?
|
Loop on Henle
|
|
|
What is location where filtration takes place, has vascular pole where blood enters and urinary pole where urine exits?
Essentially it is the combination of the glomerulus and bowman's capsule |
Renal Corpuscle
|
|
|
What do afferent arterioles do with blood?
|
Carry blood into glomerulus ("APPROACH glomerulus")
|
|
|
What do efferent arterioles do with blood?
|
Carry blood out of glomerulus ("EXIT glomerulus")
|
|
|
This capillary bed is where filtration occurs
|
Glomerulus
|
|
|
Capillaries within glomerulus are made of __________ cells and ___________. (Cells of filtration)
|
Endothelial cells and podocytes
|
|
|
What is the structure that surrounds the glomerulus?
|
Bowman's capsule
|
|
|
What are the 2 types of cells the make up bowman's capsule and what are their locations?
|
Parietal epithelial cells- outer surface
Mesangial cells- in the lumen of glomerulus and assist blood moving through |
|
|
Arteries:
Run with the radial axis of kidney |
Interlobar arteries
|
|
|
Arteries:
run perpendicular to interlobar arteries |
Arcuate arteries
|
|
|
Arteries:
branch off the arcuate arteries |
Interlobular arteries
|
|
|
Arteries:
comes off other end of capillary bed within renal corpuscle and goes around the proximal convoluted tubule Also allows for substance exchange between loop of henle and vasa recta |
Efferent arterioles
|
|
|
Describe the pathway of efferent arterioles
|
comes off other end of capillary bed within renal corpuscle and goes around the proximal convoluted tubule → loop of henle → distal convoluted tubule → interlobular veins → arcuate veins
|
|
|
Capillary bed that surrounds the entire nephron
|
Vasa recta
|
|
|
Describe the path of blood through the vasa recta
|
Drains into stellate veins → interlobular veins → arcuate veins → interlobar veins → renal veins → system
|
|
|
Blood flow vs filtrate is in what relative direction?
|
Opposite
|
|
|
Renal arteries have one of the highest blood pressures in the body at _________ mmHg
|
100 mmHg
|
|
|
Place in order of relative pressure from highest to lowest:
Peritubular capillaries Arcuate veins Arcuate arteries Glomerulus |
Arcuate artery (100 mmHg)
Glomerulus (45-60 mmHg) Peritubular capillaries (18, 13, 10 mmHg) Arcuate veins |
|
|
Second step in filtration is generation of _________ fluid pressure
|
High
|
|
|
Cells:
Have contractile properties and provides mechanical barrier to filtration |
Podocytes
|
|
|
Cells:
Forms filtration slits |
Podocytes
|
|
|
Cells:
Has primary and secondary extensive processes. |
Podocytes
|
|
|
Cells:
Secondary process involves pedicels, which are finger-like projections allowing fluid to move through |
Podocytes
|
|
|
Cells:
Fenestrated to allow fluid to pass through |
Endothelial cells
|
|
|
Cells:
2 cell types that make up glomerulus |
Podocytes and endothelial cells
|
|
|
Glomerular membrane has what 3 layers?
|
Lamina densa
Lamina rara Externa Lamina rar Interna |
|
|
Glomerula membrane is the filtering membrane involved in what step of filtration?
|
Third step
|
|
|
Glomerular membrane layers:
Utilizes size exclusion |
Lamina densa
|
|
|
Glomerular membrane layers:
Utilizes collagen and laminin |
Lamina densa
|
|
|
Glomerular membrane layers:
Utilizes heparin sulfate |
Lamina rara (externa & interna)
|
|
|
Glomerular membrane layers:
Central layer that appears dark |
Lamina densa
|
|
|
Glomerular membrane layers:
Surrounds central layer and appears light in color |
Lamina rara (externa & interna)
|
|
|
Glomerular membrane layers:
Resists movement of charged particles |
Lamina rara (externa & interna)
|
|
|
2 functions of glomerular membrane
|
1. Pass large amounts of fluid
2. Have selective permeability |
|
|
Glomerular filtration rate (GFR) is averaged at _____ L / Day or _______ the body weight or _________ mL / Minute
|
180 L / Day
or Twice the body weight or 125 mL / Minute |
|
|
What are 3 functions of Mesangial cells?
|
1. Provides structural support
2. Synthesis of ECM 3. When mesangial cells contract: a. Decreases glomerular membrane area b. Decreases GFR |
|
|
Cells:
These are contractile cells |
Mesangial cells
|
|
|
Cells:
How do mesangial cells affect blood flow? |
Decreases flow within glomerulus during contraction, and thus decrease GFR (glomerular filtration rate)
|
|
|
What are the 2 hormone receptors of Mesangial cells?
What is their main function? |
ANF (atrial natriuretic factor) and A II (angiotensin II)
These control kidney blood flow |
|
|
What are the 3 cells types in Juxtoglomerular Apparatus?
|
Macula densa cells
Juxtoglomerular cells (JG cells) Extraglomerular mesangial cells (Lacis cells) |
|
|
Juxtoglomerular Apparatus cells:
Columnar epithelial cells Secretory cells Modified DCT cells *Senses ionic content and water volume – when ionic content decreases, GFR decreases |
Macula densa cells
|
|
|
Juxtoglomerular Apparatus cells:
-Modified smooth muscle cells -Secretory cells – they secrete renin -Line afferent and efferent arterioles -*Converts angiotensinogen to angiotensin I (inactive), then angiotensin I is converted to angiotensin II (active) -Angiotensin II is a vasopressor thus when blood pressure increases, GFR increases |
Juxtaglomerular cells (JG cells)
|
|
|
Juxtoglomerular Apparatus cells:
-Have extensive cell processes -Gap junctions -Fills the space between macula densa and JG cells and helps signal between the two cell types |
Extraglomerular mesangial cells (Lacis cells)
|
|
|
Two methods of reabsorption and secretion
|
Active transport
Diffusion |
|
|
Types of active transport:
-ATP driven |
Primary
|
|
|
Types of active transport:
-ATP independent (no ATP required) -Carrier proteins |
Secondary
|
|
|
What are the two types of active transport?
|
Primary
Secondary |
|
|
What are the two types of diffusion?
|
Passive (Gradient)
Facilitated |
|
|
Types of Diffusion:
-Osmotic -Concentration -Charge |
Passive (Gradient)
|
|
|
Types of Diffusion:
-Ion Channels -Carrier Proteins |
Facilitated
|
|
|
Tubules:
1. Low columnar cuboidal epithelium 2. Brush border – increase cell membrane surface area 3. Apical caniliculi |
Proximal convoluted tubule
|
|
|
Tubules:
Function is absorption and secretion |
Proximal
|
|
|
Tubules:
1. Cuboidal Epithelium 2. Penetrates the Cortex 3. NO brush border, doesn’t have a lot of surface area, not a major player in absorption |
Distal
|
|
|
Tubules:
How does DCT differ from PCT? |
DCT differs from PCT in:
-No Brush border -No apical Canaliculi -Cells smaller -More mitochondria (ion exchange) |
|
|
|
|
|
Tubules:
-Cuboidal Epithelium -From nephron to ureters -Empties from medullary pyramids |
Collecting tubule
|
|
|
Tubules:
Function is permeability to H2O regulated by hormonal response |
Collecting tubule
|
|
|
Concentration of Urine:
Concentrated Urine is formed by ___________ the amount of H2O |
decreasing
|
|
|
Concentration of Urine:
What are two important structures in concentration of urine? |
-Loop of Henle
-Juxtamedullary nephrons |
|
|
Concentration of Urine:
What are two mechanisms for concentrating urine? Hint: One is active, the other is passive |
-Active transport of Na+
-Passive diffusion of Urea |
|
|
Concentration of Urine:
Decreasing Body fluid osmolality = ____ H2O in urine = _____ Urine |
Decreasing body fluid osmolality = (increasing) H2O in urine = (Dilute) urine
|
|
|
Concentration of Urine:
Increasing Body fluid osmolality = ____ H2O in urine = _____ Urine |
Increasing body fluid osmolality = (decreasing) H2O in urine = (Concentrated) urine
|
|
|
Concentration of Urine:
*The further down into the tissue you go in the kidney pyramid, from cortex to medulla, the _________ the osmotic pressure – this creates the osmotic gradient. ________ osmotic pressure drives water out of the filtrate. Then, majority of water is reabsorbed in the proximal convoluted tubule. |
Higher
High |
|
|
Concentration of Urine:
Nephrons: -Short Thick Descending -Long Thin Descending and Ascending -Short Thick Ascending |
Juxtamedullary Nephrons
|
|
|
Concentration of Urine:
Nephrons: -Very Short Thin Descending -NO Thin Ascending |
Cortical Nephrons
|
|
|
Concentration of Urine:
Nephrons: Has short, thin sections of the Loop of Henle where passive diffusion out of the loop takes place |
Cortical Nephrons
|
|
|
Concentration of Urine:
Permeability: Descending limb is ___________ to water and ___________ to NaCl as the tube goes into the medulla |
Descending limb is (permeable) to water and (impermeable) to NaCl as the tube goes into the medulla
|
|
|
Concentration of Urine:
Permeability: Ascending limb is ___________ to water and ___________ to NaCl |
Ascending limb is (impermeable) to water and (permeable) to NaCl
|
|
Juxtamedullary Nephron
|
Juxtamedullary Nephron
|
|
Juxtamedullary Nephron
|
Juxtamedullary Nephron
|
|
Juxtamedullary Nephron:
Permeability: |
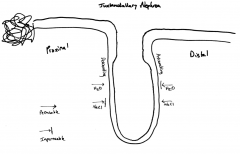
Juxtamedullary Nephron:
Permeability: |
|
|
Concentration of Urine:
What are 2 key structures of Countercurrent mechanism? |
-Loop of Henle
-Ascending -Descending -Vasa Recta |
|
|
Excretion of Urine:
What are the 2 main structures of urine excretion process outside the nephron? |
-Collecting Tubules
-Papillary Ducts |
|
|
Excretion of Urine:
Outside of nephron: ___________ come together to form ___________, which collect fluid from nephrons |
(collecting tubules) come together to form (papillary ducts), which collect fluid from nephrons
|
|
|
Excretion of Urine:
What are the 4 main structures of urine excretion process outside the nephron? |
-Renal pelvis
-Calyces -Ureter -Bladder |
|
|
Excretion of Urine:
Under each renal pyramid: you can see ___________ – they all combine to form ___________ |
Under each renal pyramid: you can see (minor calyces) – they all combine to form (major calyces)
|
|
|
Excretion of Urine:
All major calyces come together and form the ___________ – this whole area is called the ___________ |
All major calyces come together and form the (ureter proper) – this whole area is called the (renal pelvis)
|
|
|
Excretion of Urine:
Ureter Is formed from calyces: What are the 3 layers? |
-Mucosa
-Lamina Propria -Smooth Muscle |
|
|
Excretion of Urine:
3 Layers of ureter: What layer is on the inside – with transitional epithelium? |
Mucosa
|
|
|
Excretion of Urine:
3 Layers of ureter: What layer varies from loose to dense CT between mucosa |
Lamina Propria
|
|
|
Excretion of Urine:
3 Layers of ureter: What layer is on the outside- internal longitudinal, middle, and outer longitudinal? |
Smooth muscle
|
|
|
Excretion of Urine:
Section of the ureter: What epithelium is specifically designed to stretch and maintain a waterproof lining that prevents water from moving through the epithelium? |
Transitional epithelium
|
|
|
How many cell layers wide is the ureter in its:
Relaxed state? Stretched state? |
Relaxed state= 7-8 cell layers wide
Stretched state= 3 cell layers wide |
|
|
Male ureter is long and is separated into what 4 parts starting from most proximal?
What is the tissue type of each part? Lastly which part contains the sphincter? |
-Prostatic (Transitional ep.)
-Membranous (Stratified or pseudostratified columnar ep.) -contains sphincter -Bulbous (Pseudostratified columnar ep.) -Pendulous (Pseudostratified columnar ep.) |
|
|
Female ureter is short and is made of what tissue type?
What tissue is the external sphincter made of? |
Female urethra is stratified squamous epithelium
External sphincter is striated voluntary |

