![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
80 Cards in this Set
- Front
- Back

Common finding in adults.
|
Solar lentigo. (liver spots)
|
|

Targets. What is this?
|
Erythema multiforme. Hypersensitivity reaction commonly caused by mycoplasma or HSV
|
|

What causes this?
|
Tinea versicolor. The Malassezia furfur. Fungus acid inhibits melanosomes.
|
|

Gluten-sensitive enteropathy.
|
Dermatitis herpetiformis. IgA-anti-IgA complexes deposit subdermal
|
|
|
Compare the terms:
macula vs patch papule vs. nodule vesicle vs. bulla wheal vs. angioedema |
Macule: flat, circumscribed area of skin discoloration. Patch > 1 cm macula.
Papule: circumscribed elevation of the skin < 5 mm diameter. Nodule > 5 mm. Vesicle: colleciton of fluid < 5 mm. Bulla > 5 mm. Weal: cutaneous edema, angioedema: dermis edema. |
|
|
Define the terms.
Maceration: Lichenification: Excoriation: |
Maceration: surface softening due to constant wetting.
Lichenification: thickening of the skin secondary to scratching. Excoriation: secondary, superficial ulceration due to scratching |
|
|
Define the histological terms.
Hyperkeratosis: Parakeratosis: Acantholysis: Acanthosis: Exocytosis: |
Increased thickening of stratum corneum.
Persistence of nuclei in stratum corneum layer. Loss of cohesion between keratinocytes. Hyperplasia of the stratum spinosum. Exocytosis: infiltration of the epidermis by inflammatory or circulating blood cells. |
|
|
What are the cell layers of the skin?
|
Stratum basalis: dividing stem cells (50 day turnover). Stratum spinosum: contain desmosomes. Stratum granulosum: contain keratohyaline granules. Stratum lucidum: only in thick skin. Stratum corneum: anucleated cells with keratin.
|
|
|
How does the basement membrane of the skin remain attached to the superficial dermis and the dermis?
|
BM is attached to keratinocytes via hemidesmosomes. BM is attached to dermis via anchoring fibrils (type IV collagen).
|
|
|
Describe the function of melanocytes and where they are located?
|
Melanocytes are derived from neural crest cells and are located in the stratum basalis (whites) or in all layers (blacks). They synthesize melanin in melanosomes which are passed to keratinocytes. Tyrosinase converts tyrosine to DOPA. DOPA is converted to melanin.
|
|
|
What causes albinism?
|
Melanocytes cannot produce melanin (absence in tyrosinase or inability to uptake tyrosine).
|
|
|
Vitiligo is associated with what disorders?
|
Hypoparathyroidism and hashimoto's. Autoimmune destruction of melanocytes causes the depigmentation.
|
|
|
What is an ephilis?
|
A freckle. Increaseed amounts of melanin pigment.
|
|
|
Is solar lentigo a result of increased number of melanoctyes or an increased production of melanin by the melanocytes?
|
Solar lentigo occurs in elderly individuals with sun damage in sun exposed areas. The result is macules due to an increase in the number of melanocytes.
|
|
|
What causes Ritter's disease?
|
Staphylococcal scalded skin syndrome (Ritter's) is causes by S. aureus which releases an exotoxin (exfoliatin) that cleaves desmoglobin that holds together the spinosum and granulosum layers.
|
|
|
Hidradenitis suppurative is an infection of what gland?
|
Hidradenitis suppurativa is a chronic condition characterized by swollen, painful, inflamed lesions in the axillae, groin, and other parts of the body that contain apocrine glands.
|
|

What is this child suffering from?
|
Impetigo, which is a contagious superficial infection. Staph aureus causes the bullous type while strep pyogenes causes the non-bollous type. Impetigo appears as pustules that rupture to form honey-colored, crusted lesions.
|
|

What pathogen causes this characteristic skin lesion?
|
Moluscum contagiosum caused by poxvirus (dsDNA) Picture shows a small bowl-shaped lesion with an umbillication.
|
|
|
Patient presents to your office with a fever, conjunctivitis, runny nose, a cough, otitis media and Koplik spots on the buccal mucosa. How will the patient present in the near future?
|
A patient with rubeola measels (ssRNA paramyxovirus, - , env) will develop a maculopapular rash after Koplik spots disappears. Complications in this patient can include acute appendicitis in children and giant cell pneumonia.
|
|
|
40 year old male presents with polyarthritis, a maculopapular rash, and painful postauricular lymphadenopathy. What pathogen caused these symptoms?
|
Rubella (German measels, RNA togavirus, +, Env).
|
|
|
Patient presents with a slapped face appearance on his cheeks. The maculopapular rash also spreads to the trunk. What virus caused this and what other disorders are caused by this virus?
|
The patient has erythema infectiosum caused by parvovirus B19 (ssDNA). Parvo also causes aplastic anemia in chronic hemolytic diseases. Pregnant mothers exposed to a child with this infection may abort the fetus.
|
|
|
What is the disease caused by HHV-6 that causes febrile convulsions?
|
Roseola infantum. Maculopapular rash occurs 3-7 days after a high fever.
|
|
|
Although clinically obvious, varicella (chickenpox) can also be diagnosed with a positive Tzanck test (scraping + culture). What are some complications of this DNA herpesvirus?
|
Reye syndrome. Pneumonia. Remains latent in cranial and thoracic sensory ganglia. Reemerges as shingles (zoster): painful vesicles following sensory dermatomes.
|
|
|
What is Reyes syndrome?
|
Reye syndrome is characterized by acute noninflammatory encephalopathy and hepatic failure. Typically occurs after a viral illness, particularly an URTI, influenza, varicella, or gastroenteritis, and it is associated with the use of aspirin during the illness.
|
|
|
Patient recovering from rubeola develops a low grade fever, non-productive cough and flu-like symptoms. What cells may a pathologist find in the lungs of this patietn?
|
Some patients will develop pneumonia as a sequela to measles. Histologically, a unique cell can be found in the paracortical region of hyperplastic lymph nodes in patients affected with this condition. This cell, known as the Warthin-Finkeldey cell, a multinucleated giant cell with eosinophilic cytoplasmic and nuclear inclusions
|
|
|
What disease in newborns and children is caused by coxsackie and the clinical features include: small grey vesicles with a halo of erythema on hands/feet, fever, sores, rash with blisters, and buccal mucosa is studded with erosions?
|
Hand, foot, and mouth disease.
|
|
|
Where are lesions present in HSV-1 and HSV-2?
|
HSV-1: cold sores on lip and face.
HSV-2: sores in genital region. HSV-1,2 can be located in both sites, but are most commonly associated with the sites above. |
|
|
You notice a row of painful vesicles on a patient. You determine this rash is secluded to a distribution pattern along the T8 dermatome. What test can you use to diagnose this disease?
|
Tzanck test. This is herpes zoster causing shingles. This DNA herpesvirus remains latent in cranial and thoracic sensory ganglia. Flair ups can result in shingles.
|
|
|
What skin lesions can Staph aureus cause?
|
Furunculosis (deep infection of a hair follicle), carbuncle (deep infection of a group of adjacent hair follicles), bollous type impetigo, Hidradenitis suppurativa (apocrine gland infection), Ritters/scalded skin
|
|
|
Patient presents with a desquamating, sandpaper-like erythematous rash. He also has a strawberry tongue appearance. The rash spares the patients face. Diagnosis?
|
Streptococcus pyogenes. Increased risk for developing poststreptococcal glomerulonephritis.
|
|
|
Name the two types of leprosy and the causitive agent.
|
Mycobacterium leprae.
Tuberculoid type: granulomas with few acid-fast bacteria. Intact cellular immunity. Lepromatous type: absence of granulomas. Lack of cellular immunity. |
|
|
What bacteria cause acne vulgaris?
|
Propionibacterium has lipases that breakdown the lipids in sebum into fatty acids. These FA cause local irritation and inflammation.
|
|
|
Whats the underlying pathophysiology of the rhinophyma that is seen in acne rosacea?
|
Sabaceous gland hyperplasia.
|
|
|
Describe the two test used for diagnosing dermatophytoses: Wood's lamp and KOH-treated skin scrapings.
|
Wood's: ultraviolet A light detects fluorescent metabolites produced by organisms.
KOH: identify yeasts and hyphae in the stratum corneum of hair shafts. |
|
|
What is the bacteria that causes syphillis and what are the stages of diseased cause by this STI?
|
Treponema pallidum.
Primary – chancre: painless ulcer (punched out). Secondary – rash on palms and soles, condyloma latum (painless, wart-like lesion). Latent. Tertiary (6-40 years later) – gummatous syphilis, cardiovascular syphilis, neurosyphilis. |
|
|
What type of leprosy will produce:
1) + lepromin test 2) Granulomas 3) Classic leonine facies 4) Autoamputation of digits |
1) Tuberculoid type
2) Tuberculoid type 3) Lepromatous type 4) Tuberculoid type |
|

What causes this disease?
|
This is a characteristic rash caused Borrelia burgdorferi (transmitted by the Ixode tick) which causes Lyme disease. May progress to meningitis and cranial nerve palsies
|
|
|
What is the pathogenesis of acne vulgaris?
|
Chronic inflammation of the pilosebaceous unit. Abnormal keratinization. Increased sebum production (androgen-mediated). Propionibacterium acne produces irritating fatty acids.
|
|
|
What does acne rosacea cause?
|
Rhinophyma.
|
|
|
Tinea capitis is most commonly caused by what two pathogens?
|
Trichophyton tonsurans: negative wood's lamp.
Microsporum canis: positive wood's lamp. |
|
|
Tinea corporis (body), tinea pedis (foot), tinea cruris (groin), and tinea unguium (nail) are most common caused by _______.
|
Trichophyton rubrum.
|
|
|
What is intertigo and what causes it?
|
Intertigo is an erythrematous rash in body folds and it is caused by candida albicans.
|
|
|
Where is seborrheic dermatitis distributed on the body in adults?
|
Face, scalp. Scaly, greasy on scalp leading to dandruff. Caused by Malassezia furfur.
|
|
|
Sarcopes scabiei causes scabies and transfered from person to person via mites. What are the clinical features of scabies?
|
Mites burrow into corneum. Allergic reaction to mites: pruritis, eczematized or urticarial papules.
|
|
|
What is the pathogenesis of the most common skin disorder (autosomal dominant)?
|
Ichthyosis is characterized by dry, rough skin with marked scaling but no inflammation. There is a defect in production of filaggrin (keratohyalin granules): defect in keratinization. There is an increased thickness of the stratum corneum, absent granulosum, and hyperkeratotic, dry palms, soles, extensor areas.
|
|
|
What is the most common cause of dry skin and pruritus in the elderly (due to decreased skin lipids)?
|
Xerosis.
|
|
|
Eczema = dermatitis. Lymphocytes damage e-cadherins (desmosomes) to disappear. What are the clinical features of eczema?
|
Wheepy, vesication, crusting, chronic lichenification (thickening of skin due to itching). Acutely: erythrematous, papules, swelling. Chronic: mores scaly and lichenification.
|
|
|
Name some types of dermatitis (eczema).
|
Atopic dermatitis - type I hypersensitivity (latex gloves).
Contact dermatitis: allergic contact (type IV) or irritant (poison ivy, nickel). Discoid – associated with chronic stress. Seborrhoeic – involves hairy areas. Gravitational (stasis) – due to venous insufficiency. Asteatotic - dry skin (old age). |
|
|
What test can be used to differentiate pemphigus vulgaris and bullous pemphigoid?
|
Pemphigus vulgaris: IgG against desmosomes (type II) , intraepithelial vesicles/bullae – positive Nikolsky sign.
Bullous pemphigoid: IgG’s against basement membranes (type II), vesicles are subepidermal – negative Nikolsky sign. |
|
|
Farmer presents to you with a hyperkeratotic, pearly gray-white skin lesion in a sun exposed area. What is it?
|
Actinic (solar) keratosis: precursor to squamous cell carcinoma and is associated with chronic UV exposure.
|
|
|
Intensely pruritic, scaly, violaceous, flat-topped papules with the potential of progress to SCC are ______.
|
Lichen planus.
|
|
|
Describe two clinical signs in psoriasis.
|
Koebner phenomenon – scratching leaves a streak of skin lesions.
Auspitz’s sign: blood vessels rupture to cause bleeding. Extension of papillary dermis close to the surface of epithelium. |
|

|
Psoriasis: hyperproliferation of keratinocytes. 30% are genetically linked. Well demarcated erythematous plaques with silver scales. Normally occur on extensor surfaces.
|
|
|
Christmas tree distribution rash that spontaneously remits after 2-10 weeks: ___________.
|
Pityriasis rosea.
|
|
|
Define urticaria.
|
Urticaria: Pruritic elevation of the skin due to mast cell release of histamine (type I).
|
|
|
What is the chronic inflammatory dermal disorder associated with diabetes mellitus?
|
Granuloma annulare.
|
|
|
Acanthosis nigricans: verrucoid, pigmented skin lesion in axilla. What can this skin lesion indicated?
|
Gastrointestinal adenocarcinoma.
|
|
|
What is the skin distribution:
atopic ezcema adult acne psoriasis erythema nodosum |
Flexor surfaces.
Face/back. Extensor surfaces. Anterior shins. |
|
|
What is the pathogenesis of erythema nodosum?
|
Panniculitis – inflammation of the subcutaneous fat.
Immune reaction elicited by various fungi, bacteria, viral infections, malignancies, drugs, etc. Common in sarcoidosis. |
|
|
Name some melanocytic lesions.
|
Ephelis
Lentigines Acquired melanocytic nevi Common mole Blue nevus Cellular blue nevus Spindle and epithelioid nevus of Spitz Halo nevus Dysplastic nevus |
|
|
Increased pigment production or increase in melanocyte:
Ephelis Solar lentigo/lentigo simplex Dysplastic naevi Melanocytic naevi Melasma |
Pigment
Melanocytes Melanocytes Melanoctyes Pigment |
|
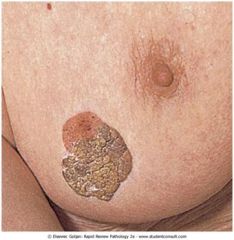
Is this benign or malignant?
|
Seborrheic keratosis: coin like macular to raised lesion that occurs in individuals older than 50.
|
|
|
What is Leser-Trelat sign and what is it an indicator of?
|
Leser trelat sign: rapid increase in the number of keratoses. This can be a paraneoplastic syndrome of stomach adenocarcinoma.
|
|
|
Is a keratocanthoma benign or malignant?
|
Benign skin neoplasm that rapidly develops. It mimics SCC, but will heal spontaneously with scarring.
|
|
|
Name the four histologically different melanocytic naevi (aka benign neavi, common mole).
|
Junctional: macule; nested proliferation that occurs along the basal cell layer.
Compound: pigmented papillomatous surface; nested proliferation extends into dermis. Intradermal naevi: often hairy; no epidermal nest; entirely dermal. Dysplastic naevi: |
|
|
Describe the microsopic and macroscopoic appearance of a dysplastic neavi.
|
Micro: dysplasia - abnormal architecture, mitosis, nuclei:cytoplasm ratio, hyperchromasia. Shoulders (junctional nests on either side), loss of melanin, and linear fibrosis surrounding the epidermal rete ridges.
Macro: diameter greater than 6 mm, irregular borders, irregular distribution of melanin. |
|
|
What is the acronym ABCDE stand for when using it to observe a skin lesion?
|
A - asymmetry
B - border (irregular) C - color (multicolor, changes) D - diameter (>10 mm, changes) E - elevation |
|
|
What are the 7-point checklist (major and minor) used to determine if a skin lesion could be malignant?
|
Major: change in size, shape, color
Minor: diameter >6mm, inflammation, bleeding/oozing, and mild itch or altered sensation |
|
|
What are the risk factors for developing melanoma?
|
Excessive sunlight at a young age, chronic sun exposure, and intermittent sun burning.
Family history (1st, 2nd relatives). Dysplastic naevi syndrome (autosomal dominant). Light complexion (+ red/blond hair). Xeroderma pigmentosum (autosomal recessive, defect in DNA repair). |
|
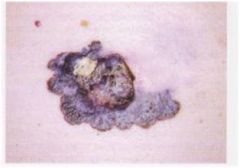
What scale would you use to determine the prognosis of a patient with this lesion?
|
This is a malignant melanoma. Breslow's depth is measured from the granular layer of the epidermis down to the deepest point of invasion. < 0.76 mm invasions: do not metastasize. > 1.7 mm invasions have potential for lymph node metastasis.
|
|
|
What are the steps in tumor progression of a melanoma?
|
Atypical melanocyte hyperplasia.
In situ melanoma. Invasive radial growth phase: no metastatic potential. Invasive vertical growth phase: malignant cells penetrate the underlying reticular dermis. |
|
|
What are the four common types of melanoma?
Which is the most common? |
Superficial spreading: (70%), ass. w/ sunburn, may contain areas of regression, extremities/back.
Lentigo maligna: (4-10%), long radial growth phase, flat, on face. Nodular: (15-30%), no radial growth, directly invasive, poor prognosis. Acral lentiginous: (2-8%), palm/sole/subungual, most common melanoma in blacks. |
|

This is Hutchinson's sign. What is this?
|
Acral lentiginous melanoma. Account for 2-8% of meloma cases. It is the most common melanoma in blacks and commonly found on soles of feet, palms, and subungual. This cancer has a poor prognosis.
|
|
|
Patient presents with a skin lesion. You describe it as a pearly, telangiectatic nodule. It is most likely this is the most common malignant skin tumor. How would this nodule look on a histological slide?
|
Basal cell carcinoma which arises from the basal cell layer of the epidermis. Risk factor: chronic sun exposure. On a slide it will appear blue and have palisading nuclei. BCC does not metastasize.
|
|
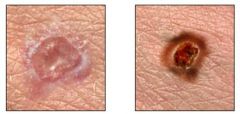
Which is SCC and BCC?
|
Left: BCC. Pearly, telangectatic nodule.
Right: SCC. Scaley nodule that is often ulcerated. |
|
|
What are some risk factors for SCC?
|
Excessive exposure to UV light (damage to DNA or damage to (Langerhan’s)), actinic keratosis, lichen planus, Bowen’s disease – SCC in situ, arsenic exposure, scar tissue in a third-degree bird, chronic ulcers and draining osteomyelitits, immunosuppressive therapy, xeroderma pigmentosum, HPV, tobacco (oral cavity), leukoplakia.
|
|
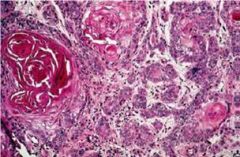
What tumor is this?
|
SCC. Note the keratinized pearl and the pink staining.
|
|
|
What are the three phases of hair growth?
|
Anagen - growth.
Catagen - resting phase. Telogen - shedding? |
|
|
What is the most common cause of hair loss in 20-40 year old women?
|
Postpartum. Other: oral contraceptive pills, stress, chemo.
|
|
|
What disease/syndrome is associated with these nail changes;
1) Nail pitting 2) Koilonychia (spoon) 3) Splinter hemorrhages 4) Mees' lines (white lines) 5) Subungual hematoma |
1) Psoriasis
2) Iron deficiency 3) Infective endocarditis and trichinosis 4) Arsenic poisoning and systemic illness 5) Blood clot due to trauma |

