![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
|
What is the term for any infection of the lung parenchyma?
|
Pneumonia
|
|
|
What is the definition of Pneumonia?
|
- Any infection of the lung parenchyma
- Can be bacterial, viral, mycoplasmal, or fungal - Can also be used for interstitial lung diseases, which are non-infectious |
|
|
How do you classify the types of Pneumonia?
|
Epidemiologically:
- Community-acquired (typical/bacteria or atypical) - Nosocomial (hospital acquired) - Aspiration - Chronic (TB/fungi) - Immunocompromised host |
|
|
What is the most common cause of Typical Community Acquired Pneumonia?
|
- Majority caused by bacterial pathogens (Streptococcus pneumonia)
- Usually d/t aerosol inhalation from infected patient - Aspiration of nasopharyngeal flora during sleep |
|
|
What are the two patterns for the gross pathology of Pneumonia?
|
- Lobar Pneumonia (entire lobe involved)
- Bronchopneumonia (patchy areas around bronchioles) |
|
|
What are the characteristics of Lobar Pneumonia?
|
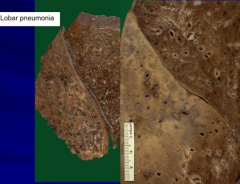
Entire Lobe involved
|
|
|
What are the characteristics of Bronchopneumonia?
|

Patchy areas around bronchioles
|
|
|
What are the four stages of Lobar Pneumonia?
|
1. Congestion
2. Red Hepatization 3. Gray Hepatization 4. Resolution |
|
|
What is the first stage of Lobar Pneumonia? What happens during this stage?
|
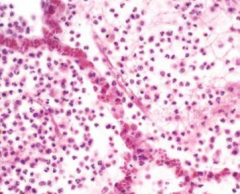
Congestion:
- Vascular engorgement / capillary leak - Neutrophil migration - Intra-alveolar fluid |
|
|
What is the second stage of Lobar Pneumonia? What happens during this stage?
|
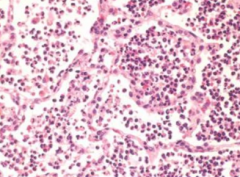
Red Hepatization
- Confluent exudate w/ RBCs - Red, firm and airless lung - "Liver-like" consistency |
|
|
What is the third stage of Lobar Pneumonia? What happens during this stage?
|
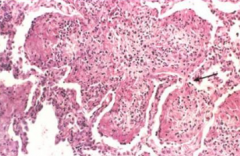
Gray Hepatization
- Fibrinosuppurative exudate - Disintegration of RBCs |
|
|
What is the fourth stage of Lobar Pneumonia? What happens during this stage?
|
Resolution
- Enzymatic degradation - Resorption - Expectoration - Macrophage ingestion - Fibroblastic organization |
|
|
What is the term for the pleural fibrinous reaction to underlying inflammation?
|
Pleuritis
|
|
|
What is Pleuritis?
|
Pleural fibrinous reaction to underlying inflammation
|
|
|
What are the potential complications of Pneumonia?
|
- Abscess
- Empyema (spread into pleural space) - Bacteremic dissemination (septic emboli, endocarditis, arthritis, etc) - Bronchopleural fistula |
|
|
What are the infectious agents of Community Acquired Pneumonia?
|
- Streptococcus pneumonia
- Haemophilus influenza - Moraxella catarrhalis - Staphylococcus aureus - Klebsiella pneumonia - Pseudomonas aeruginosa - Legionella pneumophila |
|
|
How do you acquire an atypical community acquired Pneumonia?
|
Droplet infection - inhalation
|
|
|
What are the symptoms of an Atypical Community Acquired Pneumonia?
|
- Varied clinical course
- Appear as severe URIs or chest colds - Cough may be absent - Numerous extra-pulmonary abnormalities may help key in to diagnosis - Moderate to no sputum - No physical findings of lung consolidation - Moderate to no elevation in WBCs - Lack of alveolar exudate |
|
|
Why is an atypical Pneumonia considered "atypical"?
|
- Moderate to no sputum
- No physical findings of lung consolidation - Moderate to no elevation in WBCs - Lack of alveolar exudate |
|
|
What are the causes of Atypical Pneumonias?
|
- Mycoplasma pneumoniae
- Chylamydia pneumoniae - Chylamydia trachomatis (newborns) - Viruses (RSV, influenza, adenovirus) |
|
|
What is the smallest free living organism? Size?
|
Mycoplasma pneumonia (200 nm)
|
|
|
What are the features of Mycoplasma pneumonia?
|
- Smallest free living organism (200 nm)
- No cell wall - No gram staining |
|
|
What kind of antibiotics are not effective on Mycoplasma Pneumonia? Why?
|
- Cell wall inhibiting antibiotics
- No cell wall |
|
|
What symptoms does a Mycoplasma Pneumonia infection cause?
|
- Peribronchial and peribronchiolar inflammation w/ occasional organizing pneumonia
- Extrapulmonary manifestations common (rashes, hematologic effects) |
|
|
What are the features of rashes caused by Mycoplasma Pneumonia?
|
- Found on trunk and extremities in 10-20%
- Most common cause of rash + pneumonia |
|
|
What is the most common cause of a rash + pneumonia?
|
Mycoplasma Pneumonia
|
|
|
What are the hematologic effects of Mycoplasma Pneumonia? How long do symptoms last?
|
Anemia (hemolytic)
Cold agglutinins (up to 70%) - IgM Abs directed at I antigen on RBCs - May cause hemolytic anemia if high titers are present - Appear at 2 weeks, peaks at 4 weeks, and disappears in 2 months |
|
|
Who is most likely to get Aspiration Pneumonia?
|
- Markedly debilitated patients (eg, post-stroke)
- Alcoholism - Repeated vomiting - Intubated patients |
|
|
What causes Aspiration Pneumonia?
|
Aspiration of gastric contents
- Gastric acid irritates lung parenchyma - Bacteria from oral flora start infection - More often, polymicrobial and aerobic, more than anaerobic |
|
|
What are the features of an Aspiration Pneumonia?
|
Often necrotizing w/ abscess formation
|
|
|
What is a lung abscess?
|
Localized suppurative process within the lung, characterized by necrosis of lung tissue
|
|
|
What does a lung abscess look like?
|
- Cavitary lesion (few mm to 6 cm or larger)
- Cavity is filled w/ suppurative material (neutrophils and necrotic debris) - More common in R lung |
|
|
Why are lung abscesses more common in R lung?
|
Features of R bronchial make an aspiration to R lung more common
|
|
|
What are the clinical symptoms of Aspiration Pneumonia?
|
- Cough (copious foul-smelling sputum)
- Fever - Weight loss - Chest pain - Clubbing of digits |
|
|
What organisms commonly cause Aspiration Pneumonia?
|
Frequently aerobes and anaerobes
Common Anaerobes: - Streptococci - Bacteroides - Fusobacterium - Peptococcus |
|
|
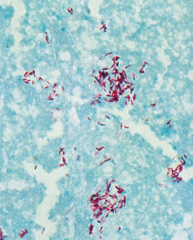
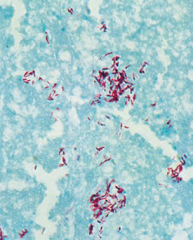
What causes tuberculosis? Characteristics of this microbe?
|
Mycobacterium tuberculosis:
- Strict aerobe - Acid fast |
|
|
Why is Mycobacterium tuberculosis acid fast?
|
Presence of mycolic acid in cell wall
|
|
|
What are the stages of Tuberculosis?
|
- Primary TB
- Secondary TB |
|
|
Who gets Primary TB? What are the symptoms?
|
- Previously unexposed TB
- Usually asymptomatic - May have low-grade fever, cough, rarely fatigued, pharyngitis, arthralgias |
|
|
How do you get primary TB?
|
- Inhalation of contaminated droplets in previously unexposed person
- MTB taken up by alveolar macrophages |
|
|
Where are there lesions in Primary TB? Characteristics?
|
- Subpleural lesion on lower part of upper lobe
- Peripheral 1-2 cm nodule w/ central caseous necrosis = Ghon focus - Granulomatous inflammation w/ necrosis |
|
|
What is a Ghon Focus?
|
- Primary lesion usually subpleural
- Often in the mid to upper zones - Caused by mycobacterium bacilli (tuberculosis) - Developed in the lung of a non-immune host |
|
|
What can happen to the lesions in primary TB?
|
- Lesions may resolve and heal w/ normal tissue
- Lesions may become fibrotic and/or calcify |
|
|
What happens to the organisms in primary TB?
|
Organisms remain viable, can reactivate and cause secondary TB
|
|
|
What causes Secondary TB?
|
Reactivation of primary site of TB
|
|
|
Where does secondary TB often occur?
|
Apex: Ventilation (oxygenation) is highest in upper lobes
|
|
|
What are the clinical findings of secondary TB?
|
- Fever
- Night sweats - Weight loss - Massive hemoptysis - Bronchiectasis |
|
|
What causes Miliary Pulmonary spread?
|
Bronchial or lymphatic invasion
|
|
|
What causes Miliary Extra-Pulmonary spread?
|
Pulmonary venous invasion (kidney is most common site)
|
|
|
What are the features of secondary TB?
|
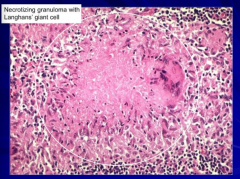
Granulomatous inflammation w/ necrosis:
- Epithelioid histiocytes - Multinucleate giant cells - Lymphocytes - Macrophages Bacteria found in necrotic material |
|
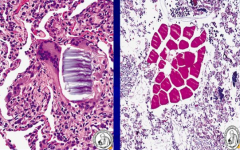
What is this?
|
Mycobacterium tuberculosis
|
|
|
What does Miliary TB look like?
|
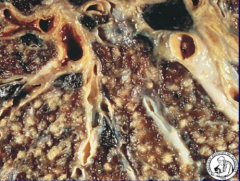
- Resembles millet seeds (small-seeded species of cereal crops or grains) in organs
- Organisms seed pulmonary venous return and enter systemic circulation - Numerous small gray-white nodules in affected organs |
|
|
What organs can be affected by miliary TB?
|
- Liver
- Kidney - Bone marrow - Spleen - Adrenals - Fallopian tubes - Epididymis |
|
|
What kind of atypical infection can commonly infect AIDS patients?
|
Mycobacterium Avium Intracellulare Complex (MAC)
|
|
|
Who is commonly infected by Mycobacterium Avium Intracellulare Complex (MAC)?
|
AIDS patients w/ CD4 T cell counts < 50 cells / µL
|
|
|
What happens in pneumonia caused by inhaled fungal infections?
|
Granulomatous inflammatory reaction w/ or w/o necrosis
|
|
|
What common pathogens cause Pneumonia in immunocompromised hosts?
|
- Cytomegalovirus (CMV)
- Pneumocystis jiroveci - Aspergillus fumigatus |
|
|
How do you treat / prevent Pneumocystis jiroveci?
|
Bactrim (Trimethoprim-Sulfamethoxazole)
|

