![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
How is water balance, and therefore serum Na+, maintained in setting of increased water intake?
|
Excretion of dilute urine
|
|
|
What are the ways to lose water?
|
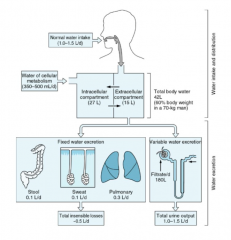
Fixed Water Excretion / total insensible losses: 0.5 L/day
- Stool (0.1 L/day) - Sweat (0.1 L/day) - Pulmonary (0.3 L/day) Variable Water Excretion: - Urine (1.0 - 1.5 L/day) |
|
|
What is osmolarity?
|
Total solute / ECF volume
|
|
|
What are the approximate concentrations of K+ and Na+ intracellularly?
|
K+: 140 mEq/L
Na+: 10 mEq/L |
|
|
What are the approximate concentrations of K+ and Na+ extracellularly?
|
K+: 4 mEq/L
Na+: 140 mEq/L |
|
|
What is the primary determinant of extracellular fluid osmolarity?
|
** Na+ concentration (140 mEq/L)
|
|
|
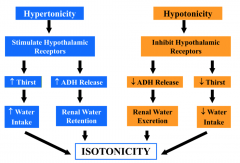
How does a hypertonic osmolarity return to isotonicity?
|
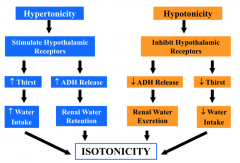
- Stimulates hypothalamic receptors
- ↑ Thirst → ↑ Water intake - ↑ ADH release → Renal water retention Causes return to isotonicity |
|
|
How does a hypotonic osmolarity return to isotonicity?
|
- Inhibits hypothalamic receptors
- ↓ Thirst → ↓ Water intake - ↓ ADH release → Renal water excretion Causes return to isotonicity |
|
|
What receptors control stimuli for ADH release? How?
|
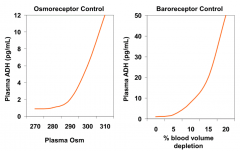
- Osmoreceptors: ↑ plasma Osm → ↑ ADH
- Baroreceptors: ↑ volume depletion → ↑ ADH |
|
|
How does osmolarity relate to ADH release? What receptors control this?
|
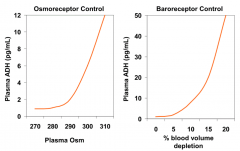
- As plasma osmolarity increases above 280, ADH release into plasma increases
- Controlled by osmoreceptors |
|
|
How does blood volume relate to ADH release? What receptors control this?
|
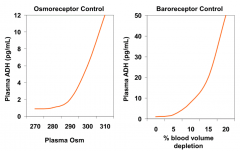
- As % blood volume depletion increases above 5%, ADH release into plasma increases
- Controlled by baroreceptors |
|
|
Where is the tubular fluid the most concentrated (highest osmolarity?
|
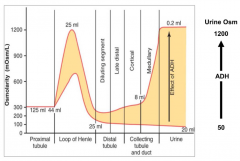
- Loop of Henle
- Medullary collecting duct (depending on amount of ADH) |
|
|
Where is the tubular fluid the least concentrated (highest osmolarity?
|
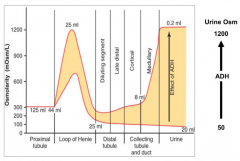
- Distal Tubule
- Cortical Collecting Tubule / Duct |
|
|
How does ADH affect urine osmolarity?
|
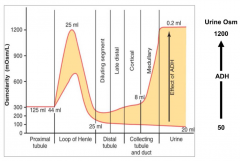
- The more ADH there is, the greater the urine osmolarity (up to 1200)
- The less ADH there is, the lower the urine osmolarity (as low as 50) |
|
|
Why did the woman in the water drinking contest die?
|
- Her serum Na+ was estimated to be 114 mEq/L (normal is 135 - 145 mEq/L)
- She overrode her decrease thirst mechanism, so continued to dilute her Na+ / hypotonic fluid |
|
|
What are the signs and symptoms of Hyponatremia?
|
- Nausea / vomiting
- Weakness - Headache - Lethargy - Seizures - Respiratory depression - Death |
|
|
What factors alter water balance?
|
- ADH (appropriate or inappropriate)
- Water intake - Altered renal water handling |
|
|
What can cause inappropriate secretion of ADH?
|
- Cancer (eg, small cell lung)
- CNS disease - Pulmonary disease - Drugs: narcotic, anti-emetics, SSRIs - HIV |
|
|
How is ECF osmolarity regulated?
|
Tightly by changes in thirst and ADH secretion
|
|
|
How does the kidney prevent hypo-osmolarity d/t increased water intake?
|
Excretes a dilute urine (osm < 100 mOsm/kg)
|
|
|
What effects can inappropriately elevated ADH have?
|
- Hyponatremia
- Hypo-osmolarity since urinary dilution is impaired (osm > 300 mOsm/kg) |
|
|
What is the GFR? Normal values?
|
-Amount of plasma filtered through glomeruli per unit time
- Normal: ~90 - 125 mL/min |
|
|
What is BUN? Function?
|
- Blood Urea Nitrogen, nitrogenous waste product of protein metabolism
- Less accurate indicator of GFR than creatinine d/t variation in protein intake, catabolic rate, tubular reabsorption - Useful in conjunction w/ creatinine in differential diagnosis of renal disease |
|
|
Why is BUN less accurate of an indicator of GFR than creatinine?
|
BUN levels vary d/t:
- Protein intake - Catabolic rate - Tubular reabsorption |
|
|
What is Creatinine? Why is it useful for estimating GFR?
|
- Breakdown product of skeletal muscle
- Production remains constant over time - Filtered at glomerulus |
|
|
Why is creatinine less accurate of an indicator of GFR than inulin?
|
- Creatinine is also secreted in nephron
- Creatinine clearance therefore overestimates GFR |
|
|
What are the limitations of creatinine for determining GFR?
|
- Creatinine is also secreted in nephron
- Creatinine clearance therefore overestimates GFR - Differences in individual muscle mass affect creatinine clearance |
|
|
How can you very roughly estimate GFR if you know creatinine?
|
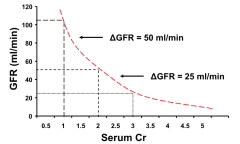
GFR ~ 100 / Cr
E.g., Serum Cr of 1 → GFR = 100 E.g., Serum Cr of 2 → GFR = 50 E.g., Serum Cr of 3 → GFR = 33 |
|
|
When is a change in serum creatinine more serious?
|
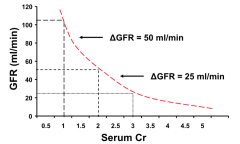
When the change is a greater percentage of the total creatinine it has a greater impact on GFR
E.g., change from 1 to 1.5 is more serious than 3 to 3.5 |
|
|
How can you use inulin values to calculate GFR?
|
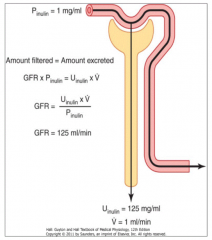
GFR = Uinulin * V / Pinulin
|
|
|
What is the Cockcroft-Gault equation used for?
|
Estimating GFR from serum creatinine (takes into account age, weight, and gender too)
|
|
|
What are the ways to calculate Creatinine Clearance?
|
- CrCl = U*V/P
- Cockcroft - Gault equation |
|
|
Why are serum creatinine based GFR estimates sometimes inaccurate?
|
Extremes in age, BMI, or muscle mass
|
|
|
Which of the following does not contribute to systemic response to extracellular fluid volume depletion?
- increased reabsorption of Na+ at PT - decreased renal nerve activity - increase ADH secretion - activation of baroreceptors |
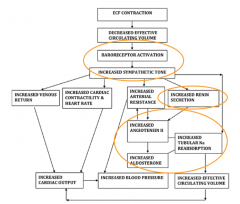
Decreased renal nerve activity
|
|
|
What factors contribute to systemic response to extracellular fluid volume depletion?
|
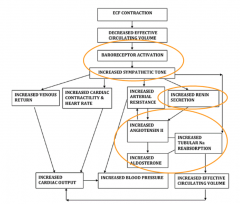
- Baroreceptor activation (increased sympathetic tone)
- Increased renin secretion - Increased AngII / increased Aldosterone = increased tubular Na reabsorption |
|
|
What are the direct tubular effects on Na+ reabsorption?
|
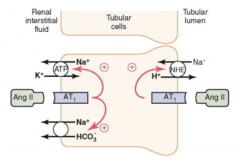
Renal sympathetic nerves:
- multiple tubular receptors stimulate Na+ reabsorption Angiotensin II: - tubular receptors - increases activity of PT Na/H counter-transporter Aldosterone: - stimulates Na+ reabsorption in cortical collecting duct principal cells - increases number of luminal Na+ channels and BL Na/K-ATPases |
|
|
What percentage of filtered load of Na+ has its excretion dependent on aldosterone action?
|
~2%
|
|
|
What controls Aldosterone secretion?
|
Angiotensin II:
- most important stimulus for aldosterone secretion relating to Na balance - AngII is dependent upon renin secretion and therefore baroreceptors, macula densa, and renal sympathetic tone |
|
|
What is the action of ADH? Where?
|
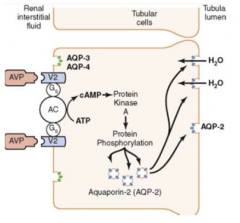
- Binds to V2 receptors on cells in late distal tubule, collecting tubules, and collecting ducts
- Leads to increased Aquaporin-2 (AQP-2) channels on the tubular lumen side to increase reabsorption of H2O - Mediated via ↑cAMP, activation of PKA, and protein phosphorylation |
|
|
What should be done to treat a patient with volume depletion due to nausea, vomiting, and diarrhea?
|
- Give normal saline (150 cc/hour IV)
- Anti-emetics - Increase oral fluid intake |
|
|
What does the systemic response to decreased ECF volume involve? Implications?
|
- Baroreceptor and sympathetic nerve activation
- Activation of Renin-AngII-Aldo system - Increased ADH - Leads to enhanced renal tubular Na+ and H2O reabsorption (leads to low urine Na+, low FENa, and elevated urine osmolarity) |
|
|
28 yo male w/ 20y hx of CKD d/t vesicoureteral reflux presents w/ weakness, bone pain, headaches, blurred vision, and nausea. BP 220/160. Ill appearing, pale sclera and nail beds, flow murmur LLSB, knobby knees/ankles w/ valgus knee deformity, ↑ DTRs w/ clonus.
Labs: Hct 7 g/dl, serum creatinine 16 mg/dl, BUN 180 mg/dl, Ca 6.5 mg/dl, phosphorus 11 mg/dl, PTH 1200 (11-54 pg/ml) What factor contributes to his parathyroidism? |
Increased serum phosphorus
|
|
|
What stimulates PTH release?
|
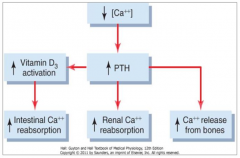
- Low Ca2+
- High Phosphorus |
|
|
What are the endocrine functions of the kidney?
|
- Renin release from juxtaglomerular cells
- Erythropoetin (epo) produced by renal cortical tubular cells, stimulates RBC production in marrow - 1,25-dihydroxy-vitamin D production formed in proximal tubule cells, regulates calcium and phosphate balance |
|
|
What are the effects of increased PTH?
|
- ↑ Vitamin D3 activation → ↑ intestinal Ca2+ reabsorption
- ↑ Renal Ca2+ reabsorption - ↑ Ca2+ release from bones |
|
|
How are calcium and phosphorus affected by kidney disease?
|

- ↑ Serum PO4 (increased retention)
- ↓ 1,25-Dihydroxy-Vitamin D - ↓ Serum Ca2+ - Decreased calcitriol production ↓ Ca2+ absorption, hypocalcemia Leads to ↑PTH release (2° Hyperparathyroidism) |

