![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
105 Cards in this Set
- Front
- Back
|
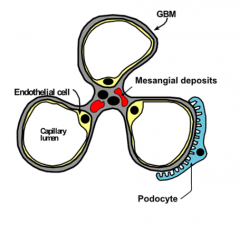
What are the mechanisms that cause glomerular disease?
|
- Immunocomplex deposition in glomerulus (activates complement resulting in neutrophil chemotaxis)
- Antibodies against GBM or glomerular Ags - Cytokine production by inflammatory cells |
|
|
How do immunocomplexes injure the kidney?
|
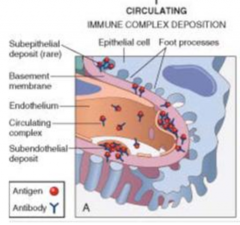
- Immunocomplexes can circulate in blood
- Then they get deposited in glomerulus - Activates complement resulting in neutrophil chemotaxis |
|
|
What is an example of immunocomplexes that injure the glomerulus?
|
DNA-anti-DNA complexes in Lupus
|
|
|
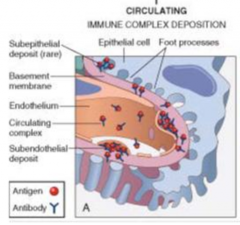
How do antibodies injure the kidney?
|
Antibodies that target the GBM or glomerular antigens
|
|
|
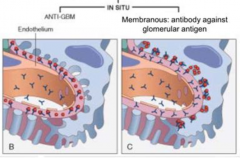
How can glomerular disease be categorized?
|
- Diffuse (all glomeruli) vs Focal (some glomeruli) injury to glomeruli
- Global (entire glomerulus) vs Segmental (fraction of glomerulus) injury to glomeruli |
|
|
How does glomerular disease present?
|
- Loss of GFR (temporal change)
- Hematuria (quality) - Proteinuria (quantity) |
|
|
What are the types of glomerular disease based on symptoms?
|
- Nephrotic syndrome
- Nephritis |
|
|
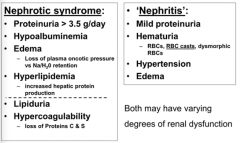
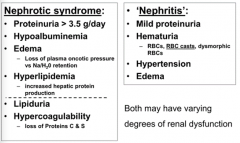
What are the features of Nephrotic Syndrome?
|
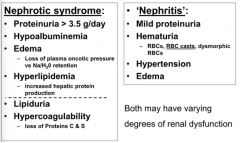
- Proteinuria >3.5 g/day
- Hypoalbuminemia - Edema - Hyperlipidemia - Lipiduria - Hypercoagulability |
|
|
What are the features of Nephritis?
|
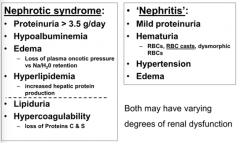
- Mild proteinuria
- Hematuria (RBCs, RBC casts, dysmorphic RBCs) - HTN - Edema |
|
|
What is similar between Nephrotic Syndrome and Nephritis?
|
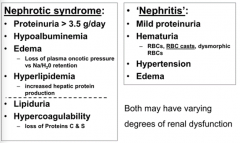
- Both have proteinuria (although >3.5g/day in nephrotic syndrome)
- Both have edema |
|
|
What factors distinguish Nephrotic Syndrome and Nephritis?
|
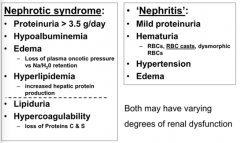
Nephrotic Syndrome:
- More proteinuria (>3.5 g/day) - Hypoalbuminemia - Hyperlipidemia - Lipiduria - Hypercoagulability Nephritis: - Mild proteinuria - Hematuria - Hypertension |
|
|
What causes edema in Nephrotic Syndrome?
|
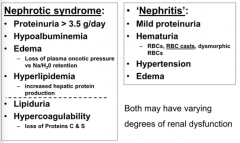
- Loss of plasma oncotic pressure
- Na/H2O retention |
|
|
What causes hyperlipidemia in Nephrotic Syndrome?
|
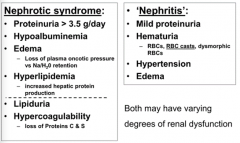
Increased hepatic protein production
|
|
|
What causes hypercoagulability in Nephrotic Syndrome?
|
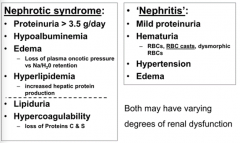
Loss of proteins C & S
|
|
|
What are the features of hematuria in Nephritis?
|
In urine: RBCs, RBC casts, dysmorphic RBCs
|
|
|
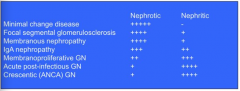
What glomerular diseases have "nephrotic syndromes" clinical manifestations?
|
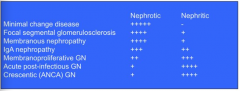
- Minimal change disease
- Focal segmental glomerulosclerosis - Membranous nephropathy |
|
|
What glomerular diseases have "nephritis" clinical manifestations?
|
- Crescentic (ANCA) Glomerulonephritis
- Acute Post-Infectious GN - Membranoproliferative GN - IgA Nephropathy |
|
|
What are the causes of Acute Glomerulonephritis (GN)?
|
- IgA nephropathy
- Post-infectious GN - Anti-GBM disease (Goodpasture's) - Small vessel vasculitis (ANCA) - Lupus nephritis - Membranoproliferative GN |
|
|
What is the most common cause of Glomerulonephritis worldwide?
|
IgA Nephropathy
|
|
|
What kind of kidney injury/disease is caused by IgA nephropathy? Who is affected by it?
|
- Glomerulonephritis
- Most between age 10-50 |
|
|
What are the most prominent features of IgA Nephropathy?
|
* Hematuria (50-60% have episodic gross hematuria, 30% persistent microhematuria, 10% acute GN or nephrotic syndrome)
- Mild proteinuria - Many sub-clinical - Dysuria and loin pain may accompany hematuria - HTN in advanced dz |
|
|
What does hematuria in IgA nephropathy occur in conjunction with?
|
*Upper respiratory infection ("synpharyngitic hematuria")
|
|
|
What is Synpharyngitic hematuria? What is it a feature of?
|
- Hematuria in conjunction with an upper respiratory infection
- Frequently in IgA nephropathy |
|
|
How do you diagnose IgA nephropathy?
|
** Immunofluorescence: Mesangial IgA deposition
- LM: variable mesangial hyper-cellularity (may see segmental proliferation, segmental sclerosis, and necrosis w/ crescents) - EM: mesangial e- dense deposits (paramesangial) |
|
|
What determines the prognosis of IgA Nephropathy?
|
- Serum creatinine
- BP - Degree of proteinuria |
|
|
What is the systemic disorder characterized by IgA deposition in multiple organs?
|

Henoch-Schönlein Purpura
|
|
|
What are the symptoms of Henoch-Schönlein Purpura? Cause?
|

- Skin: non-blanching purpura (legs / buttocks)
- Joints: transient arthralgias - GI: abdominal pain, vomiting, melena (dark smelly stool w/ blood), hematochezia (fresh blood in stool) - Kidney: hematuria, proteinuria, rarely progressive renal failure Cause: IgA deposition in multiple organs |
|
|
What is the classic cause of post-infectious GN?
|
Post-streptococcal GN
- Follows infection in nephritogenic strain of Group A β-hemolytic streptococcus - 7-14 days after pharyngitis - 14-28 days after skin infection |
|
|
What kind of streptococcal infections can cause post-infectious GN? How long does each take to cause GN?
|
- Pharyngitis: 7-14 days later
- Skin infection: 14-28 days later |
|
|
What are the most prominent features of Post-Strep GN?
|
- Sudden onset HTN
- Azotemia - Oliguria - Edema - Cola or tea colored urine |
|
|
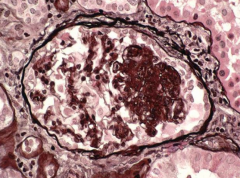
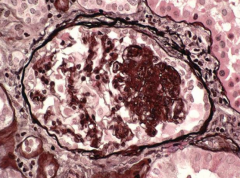
How do you diagnose Post-Strep GN?
|
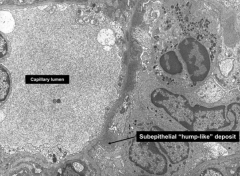
** EM: mesangial and large sub-epithelial "hump-like" deposits
- LM: enlarged, hypercellular glomeruli; diffuse mesangial and endocapillary proliferation w/ neutrophils (may see crescents) - IF: granular capillary wall and mesangial IgG and C3 - Low C3 complement level - Anti-streptolysin O (ASO) can be elevated - Urinalysis: RBC casts and mild proteinuria (nephritis) |
|
What does this EM signify?
|
Post-Strep GN
|
|
|
What is the prognosis for Post-Strep GN depending on age?
|
- Children: 95% recover w/ conservative management, 1% progress to renal failure
- Adults: 60% recover promptly |
|
|
What kind of syndrome is Rapidly Progressive GN? How long does it take to "rapidly progress"? AKA?
|
- Classic nephritic syndrome
- Rapid progression (days to weeks) to renal failure - AKA: Crescentic GN |
|
|
What are the types of Rapidly Progressive GN? Causes?
|
* Anti-GBM / Goodpasture's
* ANCA associated GN (Pauci immune) - Immune complex GN (lupus nephritis, post-infectious, cryoglomulinemia) |
|
|
Who is more commonly affected by Anti-GBM / Goodpasture's Syndrome? Cause?
|
- Males > Females
- Due to circulating anti-GBM antibody to α3-chain of type IV collagen |
|
|
What are the symptoms of Anti-GBM / Goodpasture's Syndrome?
|
May present as a pulmonary-renal syndrome:
- Hemoptysis (coughing blood) - Pulmonary infiltrates - Glomerulonephritis |
|
|
How do you diagnose Anti-GBM / Goodpasture's Syndrome?
|
** IF: LINEAR IgG and C3 on kidney biopsy
- + anti-GBM antibody in blood |
|
|
How do you treat Anti-GBM / Goodpasture's Syndrome?
|
- Plasmapheresis (remove anti-GBM)
- Prednisone - Cytoxan |
|
|
What signifies Pauci-immune GN?
|
- Crescenteric GN w/ little deposition of immune reactants
- Idiopathic OR associated w/ anti-neutrophil cytoplasmic antibody (ANCA) vasculitis |
|
|
If there is little deposition of immune reactants, what is the cause of the GN?
|
Pauci-immune GN:
- Idiopathic OR - ANCA vasculitis (anti-neutrophil cytoplasmic antibody) |
|
|
What small vessel vasculitis are associated with Pauci Immune GN?
|
- Microscopic Polyangitis (no granulomatous inflammation and no asthma)
- Wegener's Granulomatosis (necrotizing granulomatous inflammation, no asthma) - Churg-Strauss Syndrome (necrotizing granulomatous inflammation, asthma, eosinophilia) |
|
|
Which vasculitis causes no granulomatous inflammation and no asthma?
|
Microscopic polyangitis (small vessel vasculitis)
|
|
|
Which vasculitis causes necrotizing granulomatous inflammation and no asthma?
|
Wegener's Granulomatosis (small vessel vasculitis)
|
|
|
Which vasculitis causes necrotizing granulomatous inflammation, asthma, and eosinophilia?
|
Chrug-Strauss Syndrome (small vessel vasculitis)
|
|
|
What are the features of Wegener's Granulomatosis?
|
- Granulomatous vasculitis of medium to small arterioles
- c-ANCA + in 80% - URI (sinusitis, nasal lesions, hemoptysis) - Mononeuritis multiplex - Purpura - Nephritis |
|
|
What would you find on a renal biopsy with Wegener's Granulomatosis?
|
Crescenteric GN w/o immune deposits (pauci-immune)
(c-ANCA+ in 80%) |
|
|
What are the types of Rapidly Progressive GN?
|
- Anti-GBM
- Immune-complex - Pauci-immune |
|
|
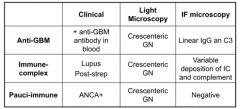
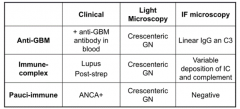
What are the clinical, LM, IF microscopy features of Anti-GBM Rapidly Progressive GN?
|
- Clinical: + anti-GBM Ab in blood
- LM: crescenteric GN - IF: LINEAR IgG and C3 |
|
|
What are the clinical, LM, IF microscopy features of Immune-Complex Rapidly Progressive GN?
|
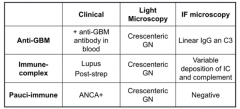
- Clinical: Lupus, Post-strep
- LM: Crescenteric GN - IF: Variable deposition of IC and complement |
|
|
What are the clinical, LM, IF microscopy features of Pauci-Immune Rapidly Progressive GN?
|
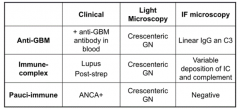
- Clinical: ANCA+
- LM: Crescenteric GN - IF: Negative |
|
|
What are the primary renal disease causes of Nephrotic Syndrome?
|
- Membranous nephropathy
- Focal segmental glomerulosclerosis (FSGS) - Minimal Change Disease (80% of children) |
|
|
What are the secondary causes of Nephrotic Syndrome?
|
- Systemic disease: *DM*, SLE, amyloidosis
- Infection: HIV, HepB, HepC, syphilis - Drugs: NSAIDs, gold, penicillamine |
|
|
What lab studies are helpful for diagnosing secondary causes of Nephrotic Syndrome?
|
- ANA, anti-dsDNA, complement levels
- Serum and urine protein electrophoreses - HBV and HCV serologies - Cryoglobulins - Syphilis serology - Renal biopsy usually indicated |
|
|
How is Nephrotic Syndrome treated?
|
All causes of nephrotic syndrome:
- ACE-I or ARBs - lower intraglomerular pressure and reduce proteinuria - Statins - lipid-lowering therapy - Diuretics or salt restriction - improve edema |
|
|
What is the most common cause of nephrotic syndrome in children?
|
Minimal Change Disease
|
|
|
When is Minimal Change Disease peak in occurrence? What kind of disease?
|
- Peak: ages 2-6
- Nephrotic syndrome |
|
|
What are the potential outcomes of Minimal Change Disease?
|
- 5% progress to ESRD
- Spontaneous remissions can occur - Tx w/ steroids can induce remission, relapses in 75% - Fewer relapses after puberty |
|
|
What can cause Minimal Change Disease in adults?
|
Idiopathic or associated with:
- Drugs: *NSAIDs* - Neoplasms: *Hodgkin's Lymphoma*, pancreatic, prostate, lung, colon, and renal cell carcinomas, mesothelioma, oncocytoma - Infections: syphilis, HIV |
|
|
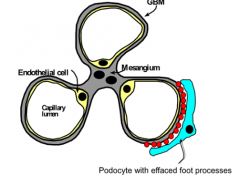
How do you diagnose Minimal Change Disease?
|
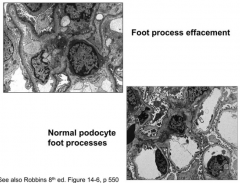
* LM: Glomeruli, interstitium, and tubules are NORMAL (hence minimal change)
* EM: Podocyte foot process effacement (FUSION) - IF: negative or mesangial IgM |
|
|
How do you treat Minimal Change Disease?
|
- Children: corticosteroids
- Adults: steroids (but takes longer to respond than children, partial remissions may occur) |
|
|
What is the most common cause of Nephrotic Syndrome in Caucasian adults?
|
Membranous Nephropathy
|
|
|
What are the secondary causes of Membranous Nephropathy? How common are secondary causes?
|
- Infection: *HBV*
- CT Disease: *SLE* - Neoplasms: *Carcinoma of lung, colon, stomach, breast; non-Hodgkin's lymphoma* - Drugs: gold, penicillamine, mercury, NSAIDs, captopril - 15-20% of cases of membranous neuropathy have secondary causes |
|
|
What infection can cause Membranous Nephropathy?
|
Hepatitis B Virus
|
|
|
What disease can cause Membranous Nephropathy?
|
CT disease: Systemic Lupus Erythematous
|
|
|
What neoplasms can cause Membranous Nephropathy?
|
- Carcinomas: lung, colon, stomach, breast
- Non-Hodgkin's Lymphoma **consider age-appropriate cancer screening |
|
|
What are the features of Membranous Nephropathy?
|
Nephrotic syndrome
- Insidious onset (gradual) - Heavy proteinuria - HTN and Azotemia - Occult malignancies and infections - Renal vein thrombosis (~20%) |
|
|
How do you diagnose Membranous Nephropathy?
|
** LM: diffuse thickening of GBM, GBM "spikes" on silver stain
- IF: granular GBM deposits of IgG - EM: SUB-EPITHELIAL deposits |
|
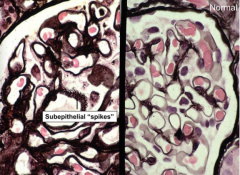
What disease is characterized by "sub-epithelial spikes"?
|
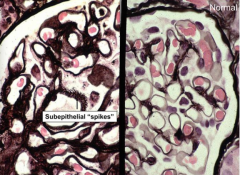
Membranous Nephropathy
|
|
|
What are the possible outcomes of Membranous Nephropathy?
|
Rule of thirds:
- 1/3 spontaneous remission - 1/3 partial remissions w/ stable function - 1/3 slowly progressive loss of renal function |
|
|
How should a patient with Membranous Nephropathy be treated?
|
- Without poor prognostic factors: manage conservatively w/ ACE-I and/or ARB (and closely follow)
- Others, steroids +/i other immunosuppressive drugs |
|
|
What is the most common cause of idiopathic nephrotic syndrome in African-Americans?
|
Focal Segmental Glomerulosclerosis (FSGS)
|
|
|
What are the symptoms of Focal Segmental Glomerulosclerosis (FSGS)?
|
- Most common idiopathic nephrotic syndrome in African Americans
- More aggressive than minimal change disease - HTN, hematuria more common - Renal dysfunction commonly progressive - ESRD 5-20 years after presentation |
|
|
What is the prognosis for patients with Focal Segmental Glomerulosclerosis (FSGS)?
|
- ESRD 5-20 years after presentation
- 50% progression to ESRD in 10 years |
|
|
What are the types of Focal Segmental Glomerulosclerosis (FSGS)?
|
- Primary FSGS: acute onset of nephrotic syndrome
- Secondary FSGS: slowly increasing renal insufficiency and proteinuria - Hereditary FSGS: mutations in proteins that make up glomerular slit diaphragm |
|
|
What can be caused by mutations in proteins that make up glomerular slit diaphragm?
|
Focal Segmental Glomerulosclerosis (FSGS)
|
|
|
What are the causes of secondary Focal Segmental Glomerulosclerosis (FSGS)?
|
* Infections: HIV *
- Drugs (NSAIDs, Heroin) - Massive obesity - Healed previous glomerular injury - Loss of functioning renal mass (unilateral agenesis, reflux nephropathy, etc) |
|
|
How do you diagnose Focal Segmental Glomerulosclerosis (FSGS)?
|
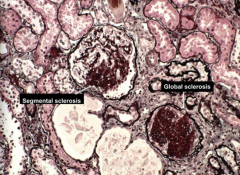
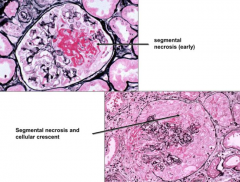
* LM: Focal and segmental glomerular sclerosis* w/ capillary collapse, hyaline and lipid deposition, and adhesion to Bowman's capsule
- IF: Negative of IgM and C3 in mesangium or in segmental scars - EM: podocyte foot process effacement, may see segmental sclerosis |
|
What does this image show? What is it diagnostic of?
|
- Segmental glomerular sclerosis
- Focal Segmental Glomerulosclerosis (FSGS) |
|
|
What determines the prognosis of Focal Segmental Glomerulosclerosis (FSGS)?
|
Degree of proteinuria (ACE-I ↓ proteinuria)
|
|
|
What are the treatment options for Focal Segmental Glomerulosclerosis (FSGS)?
|
- ACE-I - decrease proteinuria (better for prognosis)
- Corticosteroids can induce remission in some patients - Immunosuppressives for steroid-resistant patients and patients who relapse |
|
|
What glomerular diseases have nephrotic and nephritis features?
|
- Membranoproliferative Glomerulo-nephritis (MPGN)
- Lupus Nephritis (Systemic Lupus Erythematous) |
|
|
What are the features of Membranoproliferative Glomerulo-nephritis (MPGN)?
|
- Proteinuria and hematuria
- Hypertension (1/3) - Low C3 complement - 50% nephrotic syndrome - 30% asymptomatic proteinuria ± hematuria - 20% acute glomerulonephritis |
|
|
What are the potential causes of secondary Membranoproliferative Glomerulo-nephritis (MPGN)?
|
* Infections: Hepatitis C virus *, HBV, endocarditis, abscesses
- CT disease: SLE - Cryoglobulinemia - Neoplasms |
|
|
How do you diagnose Membranoproliferative Glomerulo-nephritis (MPGN)?
|
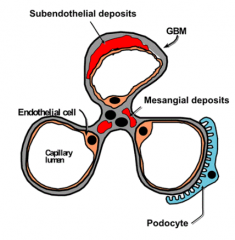
- LM: hypercellular glomeruli, endocapillary cell proliferation, lobular appearing glomeruli
- IF: granular C3 deposition - EM: subendothelial deposits |
|
|
What is Systemic Lupus Erythematosus (SLE)?
|
Multi-system auto-immune disorder:
- Abnormal auto-Ab production - Immune complex deposition - Inflammatory cell infiltration |
|
|
What is a common cause of diffuse proliferative glomerulonephritis?
|
Lupus Nephritis
|
|
|
What percentage of patients with SLE develop overt nephritis?
|
40%
|
|
|
How many types of Lupus Nephritis are there?
|
6 classes (I-VI)
|
|
|
How do you treat Lupus Nephritis?
|
- Aggressive BP control
- Control lipids - Treatment of extra-renal involvement - Classes III-V usually treated w/ corticosteroids + cytotoxic therapy |
|
|
How common is renal failure in Lupus Nephritis?
|
Class IV: renal failure rate 25% by 5-10 years
|
|
|
1. Most common Glomerulonephritis?
2. Most common nephrotic syndrome in children? 3. Most common cause of Nephrotic Syndrome in Caucasian adults? 4. Most common cause of idiopathic nephrotic syndrome in African-Americans? |
1. IgA Nephropathy
2. Minimal Change Disease 3. Membranous Nephropathy 4. Focal Segmental Glomerulosclerosis (FSGS) |
|
|
What disease is characterized by hematuria frequently occurring in conjunction w/ an upper respiratory infection ("synpharyngitis hematuria")?
|
IgA Nephropathy
|
|

What disease is diagnosed by mesangial IgA deposition on IF?
|
IgA Nephropathy
|
|

What disease is diagnosed by mesangial and large sub-epithelial "hump-like" deposits on EM?
|
Post-Strep Glomerulonephritis
|
|
|
What classic nephritic syndrome progresses rapidly (days to weeks) to renal failure?
|
Rapidly Progressive GN
|
|
|
What diseases are caused by anti-GBM antibodies or anti-neutrophil cytoplasmic antibodies (ANCA)?
|
Rapidly Progressing GN
- Anti-GBM - Goodpasture's - ANCA associated GN (Pauci Immune) |
|
|
What disease is diagnosed by linear IgG and C3 in kidney biopsy on IF?
|
Anti-GBM / Goodpasture's Syndrome
|
|
|
What disease is classically caused by NSAIDs or Hodgkin's Lymphoma?
|
Minimal Change Disease
|
|
|
What disease is diagnosed by podocyte foot process effacement (fusion) on EM and normal appearing glomeruli, interstitium, and tubules on LM?
|
Minimal Change Disease
|
|
|
What disease is classically caused either by Hepatitis B Virus, SLE, carcinoma of lung, colon, stomach, or breast, or non-Hodgkin's Lymphoma?
|
Membranous Nephropathy
|
|
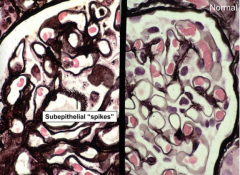
What disease is diagnosed by diffuse thickening of GBM and GBM "spikes" on silver stain in LM?
|
Membranous Nephropathy
|
|
|
What disease is classically caused by HIV infection?
|
Focal Segmental Glomerulosclerosis (FSGS)
|
|
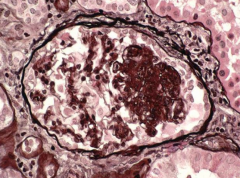
What disease is diagnosed by focal and segmental glomerular sclerosis on LM?
|
Focal Segmental Glomerulosclerosis (FSGS)
|
|
|
What disease is classically caused by Hepatitis C virus?
|
Membranoproliferative Glomerulo-nephritis (MPGN)
|

