![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
112 Cards in this Set
- Front
- Back
|
Give me the route of the right heart
|
Vena cava, atrium AV valve, ventricle, semilunar valve, pulmonary arteries
|
|
|
Give me the route of the left heart
|
pulmonary veins, atrium, av valve, ventricle, semilunar valve, aorta
|
|
|
Myogenic
|
self contracting
|
|
|
How many chambers does the heart have?
|
4
|
|
|
How many directions can blood flow through a heart valve
|
one
|
|
|
Are cardiac muscle cells and pacemaker cells the same thing?
|
No
|
|
|
Blood comes back from the venus system through the
|
vena cava
|
|
|
From the vena cava ino the
|
right atrium
|
|
|
From the right atrium through the
|
Right AV valve
|
|
|
Right AV valve names
|
tricuspid
|
|
|
Through the tricuspid to the
|
right ventrical
|
|
|
From the right ventricle to the ____ through the ____
|
lungs, Right pulmonary semilunar valve
|
|
|
From the lungs back to the heart via the
|
pulmonary veins
|
|
|
From the pulmonary veins into the
|
left atrium
|
|
|
From the left atrium through the
|
av valve
|
|
|
Left av valve other names
|
mitral valve, bicuspid
|
|
|
Through the left av valve into the
|
left ventricle
|
|
|
From the left ventricle through the
|
left semilunar valve
|
|
|
Through the left semilunar valve and into the
|
aorta
|
|
|
Which heart is working more the left or right?
|
Left
|
|
|
How can you tell visibly that the left is working harder
|
it has more muscle
|
|
|
Why is the left heart working harder
|
because its pumping blood through the entire body, righty is just going to the lungs.
|
|
|
What valve opens first
|
tricuspid
|
|
|
What valve opens second
|
pulmonary semilunar
|
|
|
What valve opens third
|
bicuspid
|
|
|
What valve opens fourth
|
aortic semilunar
|
|
|
What allows for the blood to be pushed through valves
|
pressure gradient
|
|
|
When the left ventrical contracts, what contracts to close semilunar valve?
|
Chordae tendinea and papillary muscles
|
|
|
Difference between myogenic and neurogenic cells
|
myogenic is in verts. Neuro is in inverts
|
|
|
How does an action potential arise in pacemaker cells
|
Permeability to sodium channels open. However important note: complete refractory period so that tetanus doesn’t occur |
|
|
What are the 2 characteristics of cardiac muscle account for the plateau
|
ap is caused by fast NA and slow Ca-Na channels. They open slow and stay open longer and cause the plateau. Plus calcium entering the cell enhance the contractile process. Immediately after onset of AP, permeability to K decreases by 5X, reducing outflux of K+ that is needed to return fibers to resting potential
|
|
|
Syncytium
|
the heart is made of many cells but functions as a hunit
|
|
|
Heart cells are connected via
|
gap junctions/electrical synapse
|
|
|
2 types of heart cells
|
autorhythmic and cardiac muscles
|
|
|
What are the autorhythmic cells?
|
SA node, AV node, purkinje fibers. They don’t contract.
|
|
|
Where do cardiac and autorhythmic cells originate?
|
Muscle blas cells
|
|
|
What is distinctive about the action potential in pacemaker cells?
|
Action potential ocilates
|
|
|
What is different between heart cells and skeletal muscles in terms of DHPR?
|
DHPR is not connected to the RyR.
|
|
|
SERCA
|
ATP bound pump which functions to pump calcium ions back into the sarcoplasmic reticulum
|
|
|
HCN
|
hyperpolarization activated cyclic nucleotide gated channel. The funny channel.
|
|
|
What conducts the calcium current?
|
Funny Current
|
|
|
Chronotropes
|
chemicals that change heart rate
|
|
|
Neuropenephrine and epinephrine are examples of?
|
Positive chronotropes
|
|
|
Ach is an example of?
|
Negative chronotropes
|
|
|
Why is Ach inhibitory?
|
Receptors in the heart are different than in the NMJ
|
|
|
What causes muscle contraction?
|
AP in muscle
|
|
|
Why is the falling phase more prolonged in the cardiac muscles?
|
Ca2+
|
|
|
How much more prolonged is the cardiac muscle than the skeletal muscle?
|
20-30X
|
|
|
Sodium calcium exchanger
|
Antiporter which removes calcium from the muscle cells to the extracellular fluid
|
|
|
Calcium triggered calcium release
|
calcium goes through channels to open the RyR to open the SR to release calcium
|
|
|
Why regulate calcium?
|
Heart can’t bulk up like a regular bicep muscle. So you can regulate the calcium. The more comes in, the more is removed.
|
|
|
Event leading to Vth?
|
Skeletal is through the AChR, but cardiac is through an electrical synapse. Pacemaker has a funny channel.
|
|
|
Why is there no refractory period in a pacemaker cell?
|
It’s continuously ocilating
|
|
|
Skeletal cardiac and pacemaker: Difference in Vm
|
S:-70mV stable C: -90mV stable P:-60mV Unstable
|
|
|
Skeletal cardiac and pacemaker: Difference of rising phase of ap
|
S: Na+ entry C: Na+ Entry P: Ca2+ Entry
|
|
|
Skeletal cardiac and pacemaker: Difference in repolarization
|
S: Rapid K+ Efflux C: Plateau due to Ca2+ entry, K+ efflux increases, Ca2+ decreases P: Rapid K+ efflux
|
|
|
Skeletal cardiac and pacemaker: Difference in the Duration of AP
|
S: Short 1-2ms C: extended 200+ms P: Variable (150+ms)
|
|
|
Skeletal cardiac and pacemaker: Difference in refractory period
|
S: Brief, just enough to reset the Na+Ch gates C: Long. resetting of Ca+ Ch delated until end of AP. P: None
|
|
|
What generates the action potential?
|
Atrium
|
|
|
How does the heart pulse signal send?
|
SA node passes it to the AV node. Atrium contracts. AV node to the bundle of his to perkinjie fibers. Ventricle contracts
|
|
|
Why is there an AV node delay?
|
The blood from the atrium should go through the ventrical, then from the ventrical out. If it happens simultaneously the blood wouldn’t move anywhere
|
|
|
ECG
|
Electrical view of the 3D heart, sum of total electrical activities
|
|
|
3 major components of the ECG
|
P wave QRS complex and T wave
|
|
|
P wave
|
atrial contraction
|
|
|
QRS wave
|
ventrical depolarization
|
|
|
T wave
|
Ventrical repolarization
|
|
|
Where does the ECG start?
|
Atrial depolarization
|
|
|
Where does the ECG end
|
just before the next atrial depolarization
|
|
|
PR interval
|
atrial contraction
|
|
|
QT interval
|
ventrical contraction
|
|
|
Why is the QT interval longer than PR
|
because of the AV delay
|
|
|
Diastole
|
relaxation/filling 70% of the cycle
|
|
|
Systole
|
contraction 30% of the cycle
|
|
|
5 phases of the cycle
|
mid/end diastole, atrial systole, isovolumic contraction, ventricular ejection, isovolumic relaxation
|
|
|
What parts of the cardiac cycle are in systole? What parts in diastole?
|
Systole is the isovolumic contraction and relaxation and the ventricular ejection. Diastole is the mid/end diastole and atrial systole
|
|
|
Describe the pressure in the heart during late diastole
|
Pvc>Pa>Pv
|
|
|
Describe the pressure in the heart during Atrial systole
|
Pa>>Pv (so the blood is forced into the ventricle)
|
|
|
Describe the pressure in the heart during EDV
|
Paorta>>Pv>Pa. Blood is not moving because the SL and AV are closed
|
|
|
Describe the pressure in the heart during Ventricular ejection
|
Pv>Paorta. Ventrical pressure exceeds arteries and SL valves open and blood is ejected
|
|
|
Describe the pressure in the heart during Isovolumic ventricular relaxation
|
Paorta>Pv>>Pa blood flows back into the cups of the semilunar valves and closes them. Blood may flow into the atrium
|
|
|
Where is the Lub in the wiggers diagram and where is the dub?
|
Lub is S1, Dub is S2
|
|
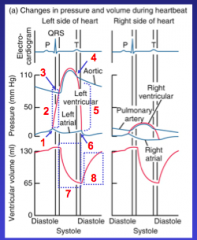
Label this diagram:
|
1: AV valves close. 2: Isovolumetric contraction. 3: SL valves open. 4: SL valves close. 5: Isovolumetric relaxation. 6: AV valves open. 7: Ventricular ejection. 8: Ventricular filling
|
|
|
Draw a pressure volume loop of one cardiac cycle. Label it.
|
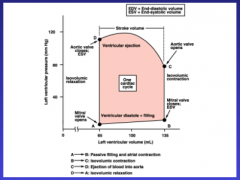
|
|
|
EDV
|
Preload, the amount of blood loaded before the heart ejects blood
|
|
|
Is big or little EDV better for heart function?
|
Big
|
|
|
Factors affecting the work done by the heart
|
EDV and afterload
|
|
|
Cardiac output is impacted by?
|
Heart rate and stroke volume
|
|
|
EDV is affected by
|
elasticity of ventricle wall, filling time, venous return, filling pressure, venous return
|
|
|
ESV is affected by
|
afterload and intropy
|
|
|
What do ESV and EDV dictate?
|
The work done by the heart
|
|
|
If preload is high, stroke volume will?
|
Increase
|
|
|
If after load is high, stroke volume will?
|
Decrease
|
|
|
What determines how much blood goes into a ventricle?
|
The more an artery contracts
|
|
|
Good of ventrical compliance?
|
More blood can get into the ventricle
|
|
|
Venous compliance is bad because?
|
More blood can get stuck int the venous system, then you can’t increase the pressure.
|
|
|
The higher the heart beat
|
the shorter the fill time, stroke volume decreases
|
|
|
Venous return is reliant upon
|
muscle contraction, respiration, gravity, vasoconstriction.
|
|
|
Respiration and EDV
|
Diaphragm constricts, relieving pressure around the heart, dropping ventricular pressure.
|
|
|
Afterload
|
resistance to ventricular ejection, the load that the heart must eject the blood against, aortic pressure.
|
|
|
Starlings law of the heart
|
as EDV increases pressure generated increases
|
|
|
Positive intropes
|
increase pressure without change in volume by increasing contractility
|
|
|
Increaseing afterload on stroke volume?
|
Decrease
|
|
|
Decreasing intropy on stroke volume?
|
Incrase
|
|
|
Increase preload on stroke volume?
|
Increase
|
|
|
How is blood pressure monitored?
|
Baroreceptors (aortic and carotid)
|
|
|
If baroreceptors sense that your BP is too high
|
vasodilation
|
|
|
If baroreceptors sense that your BP is too low
|
vasoconstriction
|
|
|
Cardiac outputs most important function?
|
Maintain MAP
|
|
|
Cardiac function is to
|
maintain blood pressure
|
|
|
What affects TPR?
|
Arterioles
|
|
|
What affects arterioles?
|
ANS (chronotropes and ionotropes) and hormones
|
|
|
What affects heart rate?
|
ANS (Chronotropes and ionotropes)
|

