![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
Explain a normal quiet breathing cycle, including pleural pressure, alveolar pressure, airflow and lung volume changes?
|
Breathing cycle:
1) Inspiratory muscles contract (Diaphragm, External intercostals, Accessory muscles-sternomastoids, scalenes) 2) Thoracic cavity expands, pulling on the pleural space and generating "- ve" P(IP) 3) "- ve" P(IP) expands the lungs (-5cm H2O at rest to -8 cm H2O) 4) Lungs increase in size/volume and thus P(A) drops to sub-atmospheric levels 5) Air flows down P(ATM) → P(A) gradient until gradient is 0 (flow stops) 6) Muscles totally relax & thoracic volume declines 7) P(IP) becomes less negative (back to -5 cm H2O) 8) Lungs decrease in size & P(A) rises above P(ATM) flowing down the P(A)→P(ATM) gradient |
|
|
At maximal inspiration, what will the P(IP) be:
A) most negative (-8 cm H2O) B) slightly negative (-5 cm H2O) C) less negative (-2 cm H2O) |

A) most negative (-8 cm H2O)
|
|
|
At maximal inspiration, what will the P(A) be:
A) most negative (-5 cm H2O) B) slightly negative (-1 cm H2O) C) none negative (0 cm H2O) |

C) none negative (0 cm H2O)
|
|
|
At maximal inspiration, what will the Flow be:
A) most negative (-8 cm H2O) B) slightly negative (-5 cm H2O) C) none negative (0 cm H2O) |

C) none negative (0 cm H2O)
|
|
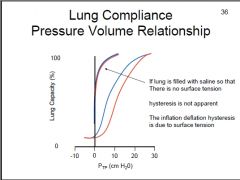
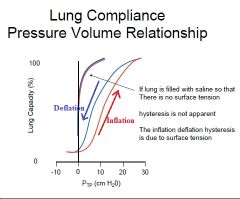
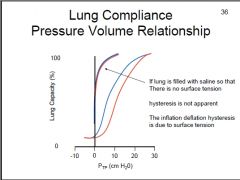
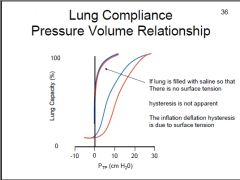
What line represents inflation?
What line represents deflation? |
|
|
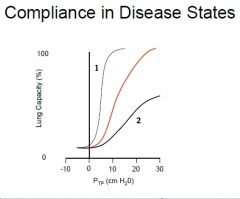
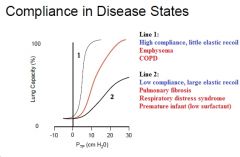
How would emphysema affect the lung compliance curve?
How would pulmonary fibrosis affect the lung compliance curve? |
Emphysema would cause a steep gradient in the pressure/volume curve or a large change in volume for a given pressure. (high compliance - ie. 10cm H2O results in 1 L volume increase)
Pulmonary fibrosis would cause a shallow gradient in the pressure/volume curve or a small change in volume for a given pressure change. (low compliance - ie. 10 cm H2O results in 0.25 L volume increase) |
|
|
What causes 'Hysteresis' of the lung compliance curve?
What is the significance of 'Hysteresis'? If we remove Hysteresis, what happens to compliance? |
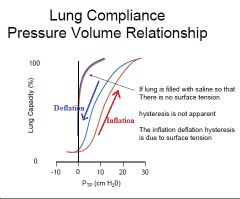
Surface tension regulates Hysteresis.
During inflation, a higher P(TP)/TLC ratio is required whereas during deflation a lower P(TP)/TLC ratio is needed. Removal of Hysteresis will increase compliance |
|
What are (3) pathological conditions that would cause high elastic recoil?
What are (2) pathological conditions that would cause high compliance? |
|
|
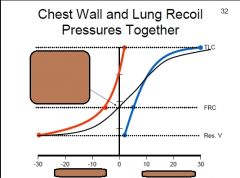
Which line represents the:
Chest wall? Lung recoil? Respiratory system? What does the point indicated by the arrow represent? |
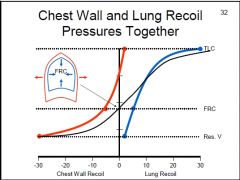
The arrow represents the Functional Residual Capacity (FRC) which is the point where chest expansion forces equal lung collapse forces.
|
|
|
How does Obstructive lung diseases affect the Vital capacity & Total lung capacity of the individual?
What are (3) Obstructive diseases? |
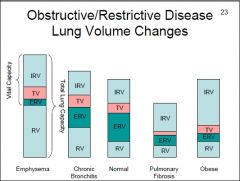
Obstructive diseases ↑ TLC at the expense of VC.
e.g. Emphysema, COPD, Chronic Bronchitis, Asthma |
|
|
How does Restrictive lung diseases affect the Vital capacity & Total lung capacity of the individual?
What are (3) restrictive lung conditions? |
Restrictive diseases ↓TLC at the expense of RV, ERV & TV.
Restrictive conditons: Pulmonary fibrosis, Respiratory distress syndrome & Premature infants |
|
|
How does surface tension affect alveolar function?
What does our body use to decrease surface tension? |
P=2T/r
A small alveolus must sustain high pressures to counterbalance a small radius. Whereas a large alveolus has a low pressure to counterbalance a larger radius. In turn, air will flow down the pressure gradient, from small to large alveoli. Thus, small alveoli have a high tendency to collapse. Surfactant decreases surface tension. |
|
|
What is atelectasis?
How does the respiratory system prevent atelectasis? |
Atelectasis is the lack of gas exchange due to alveolar collapse.
Important properties of surfactant: * ↑surface area = ↓effective surfactant concentration = ↑surface tension * ↓surface area = ↑effective surfactant concentration = ↓surface tension Thus, small alveoli are prevented from collapsing while large alveoli are prevented from expanding any further. Air is then distributed more evenly into alveoli...filling air can't move into large alveoli so smaller alveoli are then filled. |
|
|
What are the effects of airway diameter and turbulent flow on airway resistance?
|
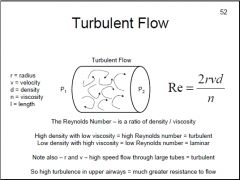
Turbulent flow in upper airways creates a much greater resistance to flow
|
|
|
How does airway resistance effect dynamic lung compliance?
|
↑airway resistance will ↑time for air to flow into or out of the lungs, as the frequency of breathing increases then ΔV experienced by the lung falls
The effect is to reduce TV w/ increasing frequency of breathing In asthma high muscle tone of the airways produces high resistance which causes the TV to decrease at even modest increases in breathing frequency Dynamic compliance falls as resistance increases!! |
|
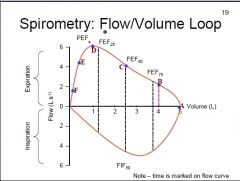
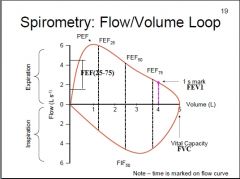
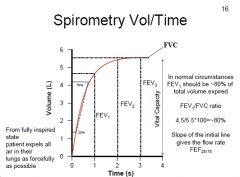
Which point represents:
FVC? FEV1? FEF(25-75) |
|
|
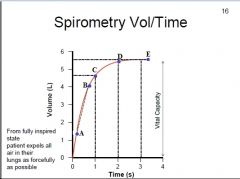
What point represents:
FVC? FEV1? FEF(25-75)? |
|
|
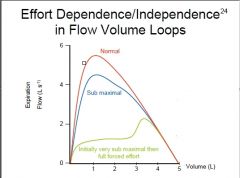
Which part of the graph is effort dependent and independent?
|
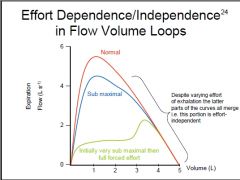
|
|
|
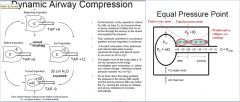
Explain Dynamic airway compression and why this makes expiratory flow effort-independent?
How does Forced expiration affect TAP? |
|
|
|
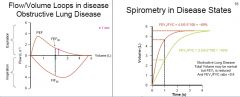
Define the spirometric abnormalities w/ Restrictive lung disease? (both volume-time & flow-volume)
|
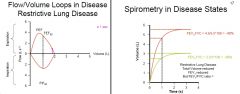
|
|
|
Define the spirometric abnormalities w/ Obstructive lung disease? (both volume-time & flow-volume)
|
|

